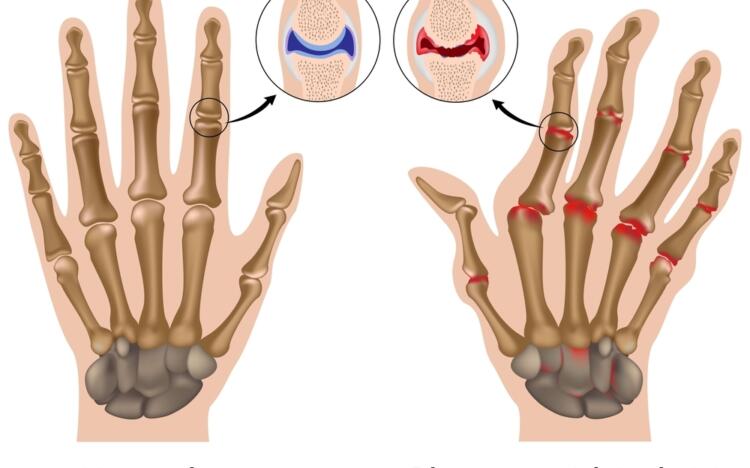
There is currently no cure for rheumatoid arthritis (RA) but treatment can help reduce joint inflammation and decrease pain and stiffness.
Starting medicines in the early stages of disease prevents permanent joint damage and improves the quality of life of people living with RA.
The type of medicines used will depend on a number of factors that determine how active the disease is and how likely it is to cause joint damage. Rheumatologists will often test different types of treatment to see which one works best. There are several types of medicine used to treat RA.
Disease-modifying antirheumatic drugs
Disease-modifying antirheumatic drugs (DMARDs) are a group of medicines that are usually given to people when first diagnosed with RA (see Table 1). These medicines reduce the activity of the immune system which is attacking and damaging healthy joints.
Methotrexate is a type of DMARD and is the recommended medicine for most people. It’s usually taken in the form of a tablet but can also be injected (just under the skin, not into a muscle or the blood stream). Methotrexate can be used in combination with other medicines, such as biological DMARDS (bDMARDS).
Table 1: Disease-modifying antirheumatic drugs | DMARD | Use |
| Conventional synthetic disease-modifying antirheumatic drugs (csDMARDs) eg, methotrexate | The first-line medicine for reducing joint damage and improving symptoms in early RA. Often given alongside other DMARDs. |
| Biological disease-modifying antirheumatic drugs (bDMARDS) eg, adalimumab, etanercept | Second-line medicine in RA. They are given as injections and are only used if other DMARDs are not working properly. |
Targeted synthetic disease-modifying antirheumatic drugs (tsDMARDS) eg, tofacitinib
| Also a second-line medicine in RA. They are given orally and may be used in place of csDMARDs and bDMARDs.
|
Steroids
Steroids, such as prednisone, can reduce inflammation in the joints and provide quick relief of symptoms. However, they’re only used short term to provide pain relief while waiting for DMARD medication to work. This is because long-term use of steroids is linked with serious side effects.
Non-steroidal anti-inflammatory drugs
Non-steroidal anti-inflammatory drugs (NSAIDs) are also given to people with RA to relieve pain and reduce inflammation in the joints. NSAIDs are only prescribed to help symptoms and do not slow down disease progression. Check with your doctor or pharmacist before taking NSAIDs over the counter particularly if you have problems with your blood pressure, heart, kidneys or stomach.