What is in this leaflet
This leaflet answers some common questions about ADDOS XR.
It does not contain all the available information. It does not take the place of talking to your doctor or pharmacist.
All medicines have benefits and risks. Your doctor has weighed the risks of you taking ADDOS XR against the benefits they expect it will have for you.
Talk to your doctor or pharmacist if you have any concerns about taking this medicine.
Keep this leaflet with your medicine. You may need to read it again.
What ADDOS XR is used for
ADDOS XR is used either to treat high blood pressure or to prevent chronic stable angina, one of the different types of angina (chest pain).
It is not used for the relief of a sudden attack of angina or to manage unstable angina.
ADDOS XR contains the active substance nifedipine, which belongs to a group of medicines called calcium channel blockers. They work by opening up blood vessels in the body to lower blood pressure and improve the supply of blood and oxygen to the heart.
This medicine is designed to allow the slow release of the nifedipine from the tablet after it is taken.
Your doctor may have prescribed ADDOS XR for another reason. Ask your doctor if you have any questions about why ADDOS XR has been prescribed for you.
It is available only with a doctor's prescription.
This medicine is not addictive.
Before you take it
When you must not take it
Do not take ADDOS XR if you are allergic to:
- medicines containing nifedipine
- other calcium channel blockers such as amlodipine, felodipine or israldipine
- any of the ingredients listed at the end of this leaflet.
Some of the symptoms of an allergic reaction may include skin rash, itching or hives, swelling of the face, lips or tongue that may cause difficulty in swallowing or breathing, wheezing or shortness of breath.
Do not take ADDOS XR if you are taking another medicine containing rifampicin.
Do not take this medicine if you have or have had:
- heart attack in the last 8 days
- cardiogenic shock (very low blood pressure due to a failing heart)
- Kock Pouch or an ileostomy.
Do not take ADDOS XR if you are pregnant. It may affect your developing baby if you take it during pregnancy.
Do not take it if you are breastfeeding. ADDOS XR passes into breast milk and may affect your baby.
Do not take it if the expiry date (Exp.) printed on the pack has passed. It may not work as well if you do.
Do not take it if the packaging shows signs of tampering or the tablets do not look quite right.
Before you start to take it
Tell your doctor if you are allergic to any other medicines, foods, dyes or preservatives.
Tell your doctor if you have or have had the following medical conditions:
- heart failure
- other heart or blood vessel disorders
- low blood pressure
- stroke
- mini-stroke (also known as TIA or transient ischaemic attack)
- liver disease
- diabetes
- narrowing of your oesophagus or intestine, e.g. due to previous injury, infection of surgery
- prolonged diarrhoea e.g. due to Crohn’s disease or ulcerative colitis.
Tell your doctor if you are pregnant or intend to become pregnant.
Tell your doctor if you are breastfeeding or intend to breastfeed.
If you have not told your doctor about any of the above, tell them before you start taking ADDOS XR.
Taking other medicines
Tell your doctor if you are taking any other medicines, including those you buy without a prescription from a pharmacy, supermarket or health food shop.
Some medicines may be affected by ADDOS XR, or may affect how well it works. These include:
- beta blockers, e.g. metoprolol, atenolol
- other medicines used to treat high blood pressure or angina, e.g. diltiazem
- medicines used to treat arrhythmia (fast or irregular heartbeats), e.g. quinidine
- other medicines used to treat heart disease, e.g. digoxin
- some medicines used to treat stomach ulcers and heartburn, e.g. cimetidine, cisapride
- rifampicin, used to treat tuberculosis and other serious infections
- other medicines used to treat bacterial infections, e.g. erythromycin, quinupristin, dalfopristin
- medicines used to treat fungal infections, e.g. ketoconazole
- medicines used to treat HIV, e.g. ritonavir
- medicines used to treat epilepsy, e.g. phenytoin, carbamazepine, valproic acid, phenobarbitone
- anti-depressants, e.g. fluoxetine, nefazodone
- tacrolimus, used to prevent rejection after organ transplant
Your doctor can tell you what to do if you are taking any of these medicines.
If you are not sure whether you are taking any of these medicines, check with your doctor or pharmacist.
Your doctor and pharmacist have more information on medicines to be careful with or avoid while taking ADDOS XR.
You should not eat grapefruit or drink grapefruit juice while you are taking this medicine because this can cause unwanted changes in the blood pressure lowering effect of the tablets.
If you have not told your doctor or pharmacist about any of the above, tell them before you start taking ADDOS XR.
How to take it
How much to take
The usual starting dose is 30 mg (one tablet) daily. Your doctor may increase the dose slowly over several weeks depending on how you respond to this medicine.
Your doctor may have prescribed a different dose.
Ask your doctor or pharmacist if you are unsure of the correct dose for you. They will tell you exactly how much to take.
Do not remove tablets from the blister pack until you are ready to take them.
Follow the instructions they give you. If you take the wrong dose, ADDOS XR may not work as well and your problem may not improve.
How to take it
Swallow the tablets whole with a glass of liquid, with or without food. ADDOS XR should not be chewed or broken up.
When to take it
The tablets are generally taken in the morning.
Take the tablets at about the same time of each day. Taking your tablets at the same time each day will have the best effect on your conditions. It will also help you to remember when to take them.
How long to take it for
ADDOS XR helps control your condition, but does not cure it. Therefore, you must take it every day. Continue taking your tablets for as long as your doctor tells you to.
If you forget to take it
If it is almost time for your next dose, skip the dose you missed and take your next dose when you are meant to.
Otherwise, take the missed dose as soon as you remember (if less than 12 hours to the next dose), and then go back to taking your tablets as you would normally.
Do not take more than one dose at a time to make up for the dose you missed.
If you are not sure what to do, ask your doctor or pharmacist.
If you take too much ADDOS XR (overdose)
Immediately telephone your doctor, or the Poisons Information Centre (telephone 13 11 26), or go to Accident and Emergency at the nearest hospital, if you think that you or anyone else may have taken too much ADDOS XR.
Do this even if there are no signs of discomfort or poisoning. You may need urgent medical attention.
Symptoms of overdose may include feeling dizzy and fainting due to a drop in blood pressure, irregular or rapid heartbeats, shortness of breath and even loss of consciousness.
While you are taking ADDOS XR
Things you must do
Take ADDOS XR exactly as your doctor has prescribed. If you do not follow your doctor's instructions, you may not get control of your blood pressure or relief from your angina.
Tell your doctor if you continue to have angina attacks or if they become more frequent while you are taking ADDOS XR.
Before starting any new medicine, tell your doctor or pharmacist that you are taking ADDOS XR.
Tell all the doctors, dentists and pharmacists who are treating you that you are taking ADDOS XR.
If you are about to be started on any new medicine, remind your doctor and pharmacist that you are taking ADDOS XR.
The use of ADDOS XR may affect results of certain laboratory tests or x-rays. If you are about to have any tests or x-rays, tell your doctor that you are taking this medicine.
If you become pregnant while taking ADDOS XR, tell your doctor immediately.
Tell your doctor if, for any reason, you have not taken your medicine exactly as directed. Otherwise, your doctor may think that it is not working and change your treatment unnecessarily.
Things you must not do
Do not use ADDOS XR to treat any other conditions unless your doctor tells you to.
Do not stop taking the tablets suddenly, or change the dosage, without checking with your doctor. You may suffer unwanted side effects if you do.
Do not give ADDOS XR to anyone else, even if they have the same condition as you.
Things to be careful of
Be careful driving or operating machinery until you know how ADDOS XR affects you. ADDOS XR may cause dizziness, light-headedness or fainting in some patients who have low blood pressure, especially when they first start taking the medicine, change dose, or drink alcohol.
Make sure you know how you react to ADDOS XR before driving a car, operating machinery, or doing anything else that could be dangerous if you are affected.
If you feel light-headed, dizzy or faint when getting out of bed or standing up, get up slowly.
This may be more noticeable when you first start taking ADDOS XR.
Standing up slowly, especially when you get up from lying down or sitting, will help your body get used to the change in position and blood pressure. If this problem continues or gets worse, talk to your doctor.
If you have angina, be careful not to overdo physical activities when you first start taking ADDOS XR. You may feel better when you start taking it, but you will need time to improve your physical fitness.
Things that may help your condition
Some self-help measures suggested below may help your condition.
Talk to your doctor or pharmacist about them:
- Alcohol - your doctor may advise you to limit your alcohol intake.
- Smoking - your doctor may advise you to stop smoking or at least cut down.
- Exercise - regular exercise helps reduce blood pressure and helps get the heart fitter, but it is important not to overdo it. Walking is good exercise, but try to find a route that is fairly flat. Before starting any exercise, ask your doctor for the program that best suits you.
- Weight – if you are overweight, your doctor may suggest losing some weight to help lower your blood pressure and lessen the amount of work your heart has to do. Some people may need a dietician’s help to lose weight.
- Diet - eat a healthy low-fat diet that includes plenty of fresh vegetables, fruit, bread, cereals and fish. Also eat less fat and sugar.
- Salt - your doctor may advise you to watch the amount of salt in your diet. To reduce your salt intake, you can use minimum salt in cooking and avoid salt at the table.
Side effects
Tell your doctor or pharmacist as soon as possible if you do not feel well while you are taking ADDOS XR.
Like other medicines, ADDOS XR can cause some side effects. Sometimes they are serious, most of the time they are not. You may need medical treatment if you get some of the side effects.
Do not be alarmed by this list of possible side effects. You may not experience any of them.
Ask your doctor or pharmacist to answer any questions you may have.
Tell your doctor if you notice any of the following and they worry you:
- headache
- dizziness or light-headedness
- feeling sick (nausea)
- flushing
- loss of energy, unusual weakness, tiredness
- constipation
- numbness in the hands and feet
- generally feeling unwell
- General swelling and/or swelling of the arms, ankles or legs.
These are the more common side effects of ADDOS XR. They are usually mild.
Bleeding, tender or swollen gums may occur some time after starting ADDOS XR. Muscle pain, trembling, visual disturbances and an increase in the need to pass water may also occur.
Occasionally, the treatment of high blood pressure may lead to slight breast swelling in older men. This side effect goes away when treatment is stopped.
Tell your doctor immediately if you notice any of the following:
- fast or irregular heartbeat
- fainting
- signs of frequent infections such as fever, severe chills, sore throat or mouth ulcers.
These side effects are rare but could be serious. You may need medical attention.
If any of the following happen after taking ADDOS XR, stop taking it and tell your doctor immediately or go to Accident and Emergency at your nearest hospital:
- chest pain
- symptoms of allergy such as rash, itching or hives on the skin, swelling of the face, lips, tongue, or other parts of the body, shortness of breath, wheezing, or trouble breathing
- symptoms of liver problems such as yellowing of the skin and/or eyes (jaundice)
- signs of frequent infections such as fever, severe chills, sore throat or mouth ulcers.
These side effects are rare but very serious. You may need urgent medical attention or hospitalisation.
Very rarely, some people experience a purple or brown discolouration of the skin, or redness, flaking and itching of the skin. Also, it has been reported that some people develop a rash or blistering of the skin when they are exposed to sunlight.
In a small number of cases of in vitro fertilisation, medicines like nifedipine appeared to have interfered with the normal function of sperm. This effect went away after the medicine was stopped. In those men who are taking ADDOS XR and are repeatedly unsuccessful in fathering a child by in vitro fertilisation, the medicine should be considered as one of the possible causes if no other explanation can be found.
Tell your doctor if you notice anything else that is making you feel unwell. Other side effects not listed above may occur in some patients.
After using it
Storage
Keep ADDOS XR where children cannot reach it. A locked cupboard at least one-and- a-half metres above the ground is a good place to store medicines.
Keep your tablets in a cool dry place where the temperature stays below 25°C.
Keep the tablets in their packs until it is time to take them. If you take the tablets out of the packs, they may not keep well.
Do not store ADDOS XR or other medicines in the bathroom or near a sink.
Do not leave ADDOS XR in the car or on window sills. Heat and dampness can destroy some medicines.
Disposal
If your doctor tells you to stop taking ADDOS XR, or your tablets have passed their expiry date, ask your pharmacist what to do with any that are left over.
Product description
What it looks like
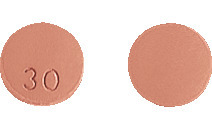
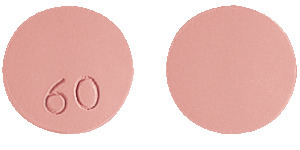
ADDOS XR comes in two strengths of tablets:
- ADDOS XR 30 – round, pale red tablet marked “30” on one side
- ADDOS XR 60 - round pale red tablet marked “60” on one side.
Each blister pack contains 30 tablets.
Ingredients
The active ingredient in ADDOS XR is nifedipine.
- each ADDOS XR 30 tablet contains 30 mg of nifedipine
- each ADDOS XR 60 tablet contains 60 mg of nifedipine.
The tablets also contain:
- purified talc
- lactose monohydrate
- povidone
- carbomer 934P
- hypromellose
- colloidal anhydrous silica
- magnesium stearate
- titanium dioxide
- iron oxide red CI77491
- macrogol 4000
- Eudragit E100.
ADDOS XR tablets contains lactose. The tablets do not contain gluten, sucrose,tartrazine or any azo dyes.
Sponsor
Arrow Pharma Pty Ltd
15-17 Chapel Street
Cremorne VIC 3121 Australia
Australian registration numbers:
ADDOS XR 30 - AUST R 114825
ADDOS XR 60 - AUST R 98806
This leaflet was revised in November 2021.
Published by MIMS January 2022


 Molecular Formula: C17H18N2O6.
Molecular Formula: C17H18N2O6.