What is in this leaflet
Read this leaflet carefully before taking your medicine.
This leaflet answers some common questions about riluzole. It does not contain all the available information. It does not take the place of talking to your doctor or pharmacist.
The information in this leaflet was last updated on the date listed on the last page. More recent information on this medicine may be available.
Ask your doctor or pharmacist:
- if there is anything you do not understand in this leaflet,
- if you are worried about taking your medicine, or
- to obtain the most up-to-date information.
You can also download the most up to date leaflet from www.apotex.com.au.
All medicines have risks and benefits. Your doctor has weighed the risks of you using this medicine against the benefits they expect it will have for you.
Pharmaceutical companies cannot give you medical advice or an individual diagnosis.
Keep this leaflet with your medicine. You may want to read it again.
What this medicine is used for
The name of your medicine is APO-Riluzole. It contains the active ingredient Riluzole.
It is used to treat people with amyotrophic lateral sclerosis, which can cause muscle degeneration leading to muscle weakness. It is a form of Motor Neurone Disease.
Ask your doctor if you have any questions about why this medicine has been prescribed for you. Your doctor may have prescribed this medicine for another reason.
This medicine is available only with a doctor's prescription.
It is important to remember that you may not feel any different when you take riluzole. The benefits of using riluzole may not be noticeable to you.
You should not stop taking riluzole without speaking to your doctor first
There is no evidence that this medicine is addictive.
Use in children
This medicine should not be used in children.
Before you take this medicine
When you must not take it
Do not take this medicine if:
- You have liver disease
- You are pregnant.
Riluzole may affect your developing baby if you take it during pregnancy. - You are breastfeeding.
Riluzole may pass into human breast milk. - You are hypersensitive to, or have had an allergic reaction to, riluzole or any of the ingredients listed at the end of this leaflet.
Symptoms of an allergic reaction may include: cough, shortness of breath, wheezing or difficulty breathing; swelling of the face, lips, tongue, throat or other parts of the body; rash, itching or hives on the skin; fainting; or hay fever-like symptoms.
If you think you are having an allergic reaction, do not take any more of the medicine and contact your doctor immediately or go to the Accident and Emergency department at the nearest hospital. - The expiry date (EXP) printed on the pack has passed.
- The packaging is torn, shows signs of tampering or it does not look quite right.
Before you start to take it
Before you start taking this medicine, tell your doctor if:
- You have allergies to:
- any other medicines
- any other substances, such as foods, preservatives or dyes.
- You have or have had any medical conditions, especially the following:
- liver disease
- kidney disease
- lung disease
- You are currently pregnant or you plan to become pregnant. Do not take this medicine whilst pregnant.
- You are currently breastfeeding or you plan to breast-feed. Do not take this medicine whilst breastfeeding.
- You have recently been vaccinated or plan to get a vaccination.
- You are planning to have surgery or an anaesthetic.
- You are currently receiving or are planning to receive dental treatment.
- You are taking or are planning to take any other medicines. This includes vitamins and supplements that are available from your pharmacy, supermarket or health food shop.
Some medicines may interact with riluzole. These include:
- theophylline - a medicine used to treat asthma.
- amitriptyline - a medicine used to treat depression
- tacrine - a medicine used in patients with Alzheimer's Disease
- some types of antibiotics e.g. rifampicin and quinolones
- omeprazole - a medicine used to treat gastric ulcers.
- some medicines used to treat depression e.g. Clomipramine and fluvoxamine
- diazepam - a medicine for sedation.
- diclofenac - a medicine used to reduce pain and inflammation.
If you are taking any of these you may need a different dose or you may need to take different medicines.
Other medicines not listed above may also interact with riluzole.
Tell your doctor if you smoke and how much coffee you drink.
Nicotine and caffeine may affect the amount of Riluzole in your body.
How to take this medicine
Follow carefully all directions given to you by your doctor or pharmacist. Their instructions may be different to the information in this leaflet.
How much to take
Your doctor or pharmacist will tell you how much of this medicine you should take. This will depend on your condition and whether you are taking any other medicines.
Do not stop taking your medicine or change your dosage without first checking with your doctor.
How to take it
Swallow tablets with a full glass of water or other liquid.
When to take it
Riluzole should not be taken immediately before or after meals, especially meals which may contain food high in fat.
Riluzole may not work as well if it is taken at the same time as your meals.
Take this medicine at the same time each day. Taking it at the same time each day will have the best effect and will also help you remember when to take it.
How long to take it for
Continue taking your medicine for as long as your doctor tells you.
Make sure you have enough to last over weekends and holidays.
Do not stop taking riluzole unless your doctor tells you to, even if you feel better.
If you forget to take it
If it is almost time to take your next dose, skip the missed dose and take your next dose at the usual time. Otherwise, take it as soon as you remember and then go back to taking your medicine as you would normally.
Do not take a double dose to make up for missed doses.
This may increase the chance of you experiencing side effects.
If you have trouble remembering to take your medicine, ask your pharmacist for some hints to help you remember.
If you take too much (overdose)
If you think that you or anyone else may have taken too much of this medicine, immediately telephone your doctor, or the Poisons Information Centre (Tel: 13 11 26 in Australia or 0800 764 766 in New Zealand).
Alternatively go to the Accident and Emergency department at your nearest hospital, Do this even if there are no signs of discomfort or poisoning. You may need urgent medical attention.
While you are taking this medicine
Things you must do
Tell your doctor that you are taking this medicine if:
- you are about to be started on any new medicine
- you plan to have any vaccinations or immunisations
- you are pregnant or are planning to become pregnant
- you are breastfeeding or are planning to breast-feed
- you are about to have any blood tests
- you are going to have surgery or an anaesthetic or are going into hospital.
Your doctor may occasionally do tests to make sure the medicine is working and to prevent side effects. Go to your doctor regularly for a check-up.
Tell any other doctors, dentists and pharmacists who are treating you that you take this medicine.
Things you must not do
Do not:
- Give this medicine to anyone else, even if their symptoms seem similar to yours.
- Take your medicine to treat any other condition unless your doctor tells you to.
- Stop taking your medicine, or change the dosage, without first checking with your doctor.
Things to be careful of
Be careful when driving or operating machinery until you know how this medicine affects you.
This medicine may cause drowsiness or dizziness in some people. Make sure you know how you react to it before you drive a car, operate machinery, or do anything else that could be dangerous if you are dizzy.
Possible side effects
Tell your doctor as soon as possible if you do not feel well while you are taking riluzole or if you have any questions or concerns.
Do not be alarmed by the following lists of side effects. You may not experience any of them. All medicines can have side effects. Sometimes they are serious but most of the time they are not.
Tell your doctor if you notice any of the following:
- stomach ache, nausea or vomiting
- headache
- joint stiffness
- skin problems e.g. rash, flaking skin
- dizziness
- sleepiness
- weakness or loss of strength
If you experience any of the following, stop taking your medicine and contact your doctor immediately or go to the Accident and Emergency department at your nearest hospital.
These are very serious side effects and you may need urgent medical attention or hospitalisation:
- irregular or fast heartbeat
- frequent infections such as fever, severe chills, sore throat or mouth ulcers
- swelling of the hands, feet or legs
- tingling sensations around the mouth
- shortness of breath or difficulty breathing
- Severe upper stomach pain, often with nausea and vomiting
- If your skin becomes itchy or yellow or if you start to bleed or bruise easily. You may be developing a liver problem.
Other side effects not listed above may occur in some patients.
Allergic reactions
If you think you are having an allergic reaction to riluzole, do not take any more of this medicine and tell your doctor immediately or go to the Accident and Emergency department at your nearest hospital.
Symptoms of an allergic reaction may include some or all of the following:
- cough, shortness of breath, wheezing or difficulty breathing
- swelling of the face, lips, tongue, throat or other parts of the body
- rash, itching or hives on the skin
- fainting
- hay fever-like symptoms.
Storage and disposal
Storage
Keep your medicine in its original packaging until it is time to take it.
If you take your medicine out of its original packaging it may not keep well.
Keep your medicine in a cool dry place where the temperature will stay below 25°C.
Do not store your medicine, or any other medicine, in the bathroom or near a sink. Do not leave it on a window sill or in the car. Heat and dampness can destroy some medicines.
Keep this medicine where children cannot reach it.
A locked cupboard at least one-and-a-half metres above the ground is a good place to store medicines.
Disposal
If your doctor tells you to stop taking this medicine or it has passed its expiry date, your pharmacist can dispose of the remaining medicine safely.
Product description
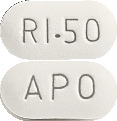
What APO-Riluzole looks like
The 50 mg tablets are white to off white coloured, film coated, capsule shaped, biconvex tablets "APO" engraved on one side and "RI-50" engraved on other side
APO-Riluzole comes in blister packs of 56 tablets
APO-Riluzole also comes in bottles* of 56, 100 & 500 tablets.
* Not all strengths, pack types and/or pack sizes may be available.
Ingredients
Each tablet contains 50 mg of riluzole as the active ingredient.
It also contains the following inactive ingredients:
- Calcium hydrogen phosphate
- microcrystalline cellulose
- croscarmellose sodium
- magnesium stearate
- hypromellose
- macrogol 8000
- titanium dioxide
- purified talc
This medicine is gluten-free, lactose-free, sucrose-free, tartrazine-free and free of other azo dyes.
Australian Registration Numbers
APO-Riluzole 50 mg tablets (blister pack):
AUST R 168091.
APO-Riluzole 50 mg tablets (bottle):
AUST R 168094.
Sponsor
Apotex Pty Ltd
16 Giffnock Avenue
Macquarie Park NSW 2113
Australia
Apotex NZ Ltd
32 Hillside Road
Glenfield
Private Bag 102-995
North Shore Mail Centre
Auckland, New Zealand
Apotex Pty Ltd is the licensee of the registered trademarks APO and APOTEX from the registered proprietor, Apotex Inc.
This leaflet was last updated in:
November 2015


 In a second dose ranging trial, 959 patients with ALS were randomised to one of four treatment groups: riluzole 50, 100, 200 mg/day, or placebo and were followed up for 18 months. In patients treated with riluzole 100 mg/day, survival was significantly longer compared to patients who received placebo. The median survival time approached 16.5 months versus 13.5 months for riluzole 100 mg/day and placebo, respectively. There were no changes from baseline observed in the functional evaluation. The effect of 50 mg/day was not statistically significant compared to placebo and the effect of 200 mg/day was essentially comparable to that of 100 mg/day. See Figure 2.
In a second dose ranging trial, 959 patients with ALS were randomised to one of four treatment groups: riluzole 50, 100, 200 mg/day, or placebo and were followed up for 18 months. In patients treated with riluzole 100 mg/day, survival was significantly longer compared to patients who received placebo. The median survival time approached 16.5 months versus 13.5 months for riluzole 100 mg/day and placebo, respectively. There were no changes from baseline observed in the functional evaluation. The effect of 50 mg/day was not statistically significant compared to placebo and the effect of 200 mg/day was essentially comparable to that of 100 mg/day. See Figure 2. A separate compassionate use study (n = 168), enabling access to treatment for patients excluded from the two pivotal studies, was designed to assess the efficacy and safety of riluzole in patients at a late stage of the disease. In this population with decreased respiratory function (baseline vital capacity less than 60%), survival time and motor function in the riluzole group did not differ significantly from that of placebo. It was anticipated that up to 300 patients would enter this study, but only 168 were enrolled (86 received placebo, 82 received riluzole). Thus the statistical power of the study was diminished.
A separate compassionate use study (n = 168), enabling access to treatment for patients excluded from the two pivotal studies, was designed to assess the efficacy and safety of riluzole in patients at a late stage of the disease. In this population with decreased respiratory function (baseline vital capacity less than 60%), survival time and motor function in the riluzole group did not differ significantly from that of placebo. It was anticipated that up to 300 patients would enter this study, but only 168 were enrolled (86 received placebo, 82 received riluzole). Thus the statistical power of the study was diminished. The following is a list of adverse reactions reported from clinical trials and postmarketing studies with an incidence of less than 1%: uncommon 0.1-1%; rare 0.01-0.1%; very rare < 0.01%; not known (cannot be estimated from the available data).
The following is a list of adverse reactions reported from clinical trials and postmarketing studies with an incidence of less than 1%: uncommon 0.1-1%; rare 0.01-0.1%; very rare < 0.01%; not known (cannot be estimated from the available data).