What is in this leaflet
This leaflet answers some common questions about sotalol. It does not contain all the available information. It does not take the place of talking to your doctor or pharmacist.
All medicines have risks and benefits. Your doctor has weighed the risks of you using this medicine against the benefits they expect it will have for you.
If you have any concerns about taking this medicine, ask your doctor or pharmacist.
Keep this leaflet with the medicine. You may want to read it again.
What this medicine is used for
Sotalol is used to prevent and treat an irregular heart rhythm or heartbeat, also known as an 'arrhythmia'.
Sotalol belongs to a group of medicines called beta-blockers.
How it works
Sotalol works by changing the body's response to some nervous impulses, especially in the heart. By doing so, sotalol helps the heart to beat more regularly and reduce the effort to which the heart has to pump blood.
Ask your doctor if you have any questions about why this medicine has been prescribed for you. Your doctor may have prescribed this medicine for another reason.
This medicine is available only with a doctor's prescription.
This medicine is not addictive.
There is not enough information to recommend the use of this medicine in children.
Before you take this medicine
When you must not take it
Do not take this medicine if you have an allergy to:
- sotalol
- any of the ingredients listed at the end of this leaflet.
Some of the symptoms of an allergic reaction may include:
- shortness of breath
- wheezing or difficulty breathing
- swelling of the face, lips, tongue, throat or other parts of the body
- rash, itching or hives on the skin.
Do not take this medicine if you have or have had any of the following medical conditions:
- bronchospasm (e.g. bronchial asthma or chronic obstructive airway disease)
- allergic disorders, such as allergic rhinitis
- severe kidney disease
- certain cardiovascular conditions.
Ask your doctor if you have any cardiovascular conditions or diseases that would stop you from taking this medicine.
Do not take this medicine if you are going to receive certain anaesthetics. You must tell your doctor if you're going to receive an anaesthetic.
Do not take this medicine after the expiry date printed on the pack or the packaging is torn or shows signs of tampering. If it has expired or is damaged, return it to your pharmacist for disposal.
If you are not sure whether you should start taking this medicine, talk to your doctor.
Before you start to take it
Tell your doctor if you have allergies to any other medicines, foods, preservatives or dyes.
Tell your doctor if you have or have had any of the following medical conditions:
- diabetes
- kidney problems
- an overactive thyroid
- phaeochromocytoma, which is a rare tumour of the adrenal gland
- any blood vessel disorders causing poor circulation in the arms and legs
- a recent heart attack
- certain types of angina (such as Prinzmetal angina or variant angina)
- any other heart problems
- problems with the levels of certain salts in your blood
- psoriasis
- eye or skin reactions, which were caused from using beta-blockers in the past.
Tell your doctor if you are pregnant or you plan to become pregnant.
Do not take this medicine whilst pregnant until you and your doctor have discussed the risks and benefits involved.
Tell your doctor if you are breastfeeding.
Do not take this medicine whilst breastfeeding.
- You are planning to have surgery or an anaesthetic.
- You are currently receiving or are planning to receive dental treatment.
If you have not told your doctor about any of the above, tell them before you start taking this medicine.
Taking other medicines
Tell your doctor or pharmacist if you are taking any other medicines, including any that you get without a prescription from your pharmacy, supermarket or health food shop.
Some medicines and sotalol may interfere with each other. These include:
- other medicines used to treat an irregular heart rhythm or heartbeat
- digoxin, a medicine used to treat heart failure
- some medicines used to treat high blood pressure, angina or other heart conditions
- insulin and other medicines used to treat diabetes
- certain types of diuretics (fluid tablets)
- some medicines used to treat depression
- antihistamines such as terfenadine and astemizole, which are used to treat hay fever and allergies
- some medicines used for asthma or other lung problems
- some medicines used during surgery or emergency situations such as anaesthetics
- some antibiotics.
These medicines may be affected by this medicine or may affect how well it works. You may need different amounts of your medicines, or you may need to take different medicines.
Your doctor and pharmacist have more information on medicines to be careful with or avoid while taking this medicine.
Other interactions not listed above may also interact with sotalol.
How to take this medicine
Follow all directions given to you by your doctor or pharmacist carefully. They may differ to the information contained in this leaflet.
If you do not understand the instructions on the bottle, ask your doctor or pharmacist for help.
How much to take
Your doctor will tell you how much of this medicine you should take. This depends on your condition and whether you are taking any other medicines.
How to take it
Swallow the tablets whole with a full glass of water.
Do not take the tablets with any drinks that contains milk. Milk can interfere with the absorption of sotalol.
When to take it
Take your medicine on an empty stomach, at least half an hour (ideally 1-2 hours) before, or two hours after, a meal or milk-containing products.
Take this medicine at about the same time each day. Taking it at the same time each day will have the best effect and will also help you remember when to take it.
How long to take it for
Continue taking your medicine for as long as your doctor tells you.
Make sure you have enough to last over weekends and holidays.
If you forget to take it
If it is almost time to take your next dose, skip the dose you missed and take your next dose when you are meant to.
Otherwise, take it as soon as you remember, and then go back to taking your medicine as you would normally.
Do not take a double dose to make up for the dose that you missed. This may increase the chance of you experiencing side effects.
If you are not sure what to do, ask your doctor or pharmacist.
If you have trouble remembering to take your medicine, ask your pharmacist for some hints.
If you take too much (overdose)
Immediately telephone your doctor or the Poisons Information Centre (telephone 13 11 26) for advice, or go to Accident and Emergency at your nearest hospital, if you think that you or anyone else may have taken too much of this medicine. Do this even if there are no signs of discomfort or poisoning. You may need urgent medical attention.
While you are taking it
Things you must do
If you are about to be started on any new medicine, remind your doctor and pharmacist that you are taking this medicine.
Tell any other doctors, dentists and pharmacists who are treating you that you take this medicine.
If you become pregnant while taking this medicine, tell your doctor immediately.
you are breastfeeding or are planning to breast-feed
you are about to have any blood tests
you are going to have surgery or an anaesthetic or are going into hospital.
If you have a history of allergies, there is a chance that sotalol may cause allergic reactions to be worse or harder to treat.
If you are being treated for diabetes, make sure you check your blood sugar levels regularly. Sotalol may affect how well your diabetes is controlled. It may also cover up some of the symptoms of low blood sugar (also called hypoglycaemia), such as a fast heartbeat. Sotalol may also make low blood sugar last longer. Your doctor may need to change the dose of diabetes medicines (such as insulin).
Keep all of your doctor's appointments so that your progress can be checked. Your doctor may occasionally do tests to make sure the medicine is working and to prevent side effects.
Things you must not do
Do not give this medicine to anyone else, even if they have the same condition as you.
Do not take your medicine to treat any other complaints unless your doctor tells you to.
Do not stop taking your medicine or change the dosage without checking with your doctor.
Things to be careful of
Be careful while driving or operating machinery until you know how medicine affects you. Sotalol may cause dizziness, light-headedness or drowsiness in some people. If this occurs do not drive or operate machinery or any other activity that could be dangerous if dizzy, light-headed or drowsy.
Dizziness, light-headedness or fainting may occur, especially when you get up from a sitting or lying position. Getting up slowly may help.
Make sure you drink enough water in hot weather and during exercise when you are taking sotalol, especially if you sweat a lot. If you do not drink enough water while taking sotalol, you may feel faint or light-headed or sick. This is because your blood pressure is dropping suddenly. If you continue to feel unwell, tell your doctor.
Side effects
Tell your doctor or pharmacist as soon as possible if you do not feel well while you are taking sotalol.
This medicine helps most people, but it may have unwanted side effects in a few people. All medicines can have side effects. Sometimes they are serious, most of the time they are not. You may need medical attention if you get some of the side effects.
Do not be alarmed by the following lists of side effects. You may not experience any of them.
Ask your doctor or pharmacist to answer any questions you may have.
Tell your doctor or pharmacist if you notice any of the following and they worry you:
- dizziness, light-headedness or fainting, especially when getting up quickly
- tiredness, lack of energy, weakness
- cramps
- headache, fever
- feeling sick, vomiting, stomach upset, diarrhoea, wind
- change in taste sensation
- problems with sexual function
- sleep problems, unusual dreams
- worsening of psoriasis
The above list includes the more common side effects of your medicine. They are usually mild.
Tell your doctor as soon as possible if you notice any of the following:
- hearing disturbances
- tingling or numbness in the hands or feet, cold limbs
- irritated eyes, blurred vision, worsening of eyesight, increased sensitivity of the eyes to sunlight
- anxiety, depression, mood changes
The above list includes serious side effects that may require medical attention.
If any of the following happen, stop taking your medicine and either tell your doctor immediately or go to Accident and Emergency at your nearest hospital:
- chest tightness, wheezing, shortness of breath
- very slow heartbeat
- fast, irregular heartbeat, palpitations
- chest pain
- any type of skin rash, itching
- shortness of breath (sometimes with tiredness, weakness and a reduced ability to exercise), which may occur together with swelling of the feet or legs due to fluid build-up
- shortness of breath, wheezing or difficulty breathing; swelling of the face, lips, tongue, throat or other parts of the body; rash, itching or hives on the skin (signs of an allergic reaction).
The above list includes very serious side effects. You may need urgent medical attention or hospitalisation.
Tell your doctor or pharmacist if you notice anything that is making you feel unwell.
Other side effects not listed above may occur in some patients.
Storage and disposal
Storage
Keep your medicine in the bottle until it is time to take them. If you take the tablets out of the bottle they may not keep well.
Keep your medicine in a cool dry place where the temperature stays below 25°C. Protect from light.
Do not store your medicine or any other medicine in the bathroom or near a sink. Do not leave it on a window sill or in the car. Heat and dampness can destroy some medicines.
Keep this medicine where children cannot reach it. A locked cupboard at least one-and-a-half metres above the ground is a good place to store medicines.
Disposal
If your doctor tells you to stop taking this medicine or it has passed its expiry date, ask your pharmacist what to do with any medicine that is left over.
Product description
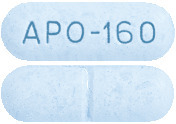
What APO-Sotalol Tablets looks like
80 mg tablets:
Blue, capsule-shaped, biconvex tablets, engraved APO-80 on one side and scored on the other. AUST R 83094.
160 mg tablets:
Blue, capsule-shaped, biconvex tablets, engraved APO-160 on one side and scored on the other. AUST R 73846.
These tablets are packed in a bottle containing 60 tablets.
*Not all strengths, pack types and/or pack sizes may be available.
Ingredients
Each tablet contains 80mg or 160 mg of sotalol hydrochloride as the active ingredient.
It also contains the following:
- dextrates
- methylcellulose
- magnesium stearate
- colloidal anhydrous silica
- indigo carmine aluminium lake.
This medicine contains sugars as dextrose
This medicine does not contain gluten, lactose, sucrose, tartrazine and other azo dyes.
Sponsor
Apotex Pty Ltd
16 Giffnock Avenue
Macquarie Park NSW 2113
APO- and APOTEX are registered trademarks of Apotex Inc.
This leaflet was prepared in September 2018.
Published by MIMS March 2019


 Other risk factors for torsade de pointes were excessive prolongation of the QTc and history of cardiomegaly or congestive heart failure. Patients with sustained ventricular tachycardia and a history of congestive heart failure have the highest risk of serious proarrhythmia (approximately 7%). Proarrhythmic events must be anticipated not only on initiating therapy, but with every upward dose adjustment; events tend to occur within 7 days of initiating therapy or with an increase in dose. Initiating therapy at 80 mg twice a day with gradual upward dose titration thereafter decreases the risk of proarrhythmia (see Section 4.2 Dose and Method of Administration). Sotalol should be used with caution if the QTc is greater than 500 msec on therapy, and serious consideration should be given to reducing the dose or discontinuing therapy when the QT interval exceeds 550 msec. Due to the multiple risk factors associated with torsade de pointes, however caution should be exercised regardless of the QTc interval.
Other risk factors for torsade de pointes were excessive prolongation of the QTc and history of cardiomegaly or congestive heart failure. Patients with sustained ventricular tachycardia and a history of congestive heart failure have the highest risk of serious proarrhythmia (approximately 7%). Proarrhythmic events must be anticipated not only on initiating therapy, but with every upward dose adjustment; events tend to occur within 7 days of initiating therapy or with an increase in dose. Initiating therapy at 80 mg twice a day with gradual upward dose titration thereafter decreases the risk of proarrhythmia (see Section 4.2 Dose and Method of Administration). Sotalol should be used with caution if the QTc is greater than 500 msec on therapy, and serious consideration should be given to reducing the dose or discontinuing therapy when the QT interval exceeds 550 msec. Due to the multiple risk factors associated with torsade de pointes, however caution should be exercised regardless of the QTc interval. Overall, discontinuation of sotalol due to unacceptable adverse events was necessary in 18% of all patients in cardiac arrhythmia trials. The most common adverse events leading to discontinuation of sotalol were: fatigue 4%, bradycardia (< 50 bpm) 3%, dyspnoea 3%, proarrhythmia 2%, asthenia 2% and dizziness 2%.
Overall, discontinuation of sotalol due to unacceptable adverse events was necessary in 18% of all patients in cardiac arrhythmia trials. The most common adverse events leading to discontinuation of sotalol were: fatigue 4%, bradycardia (< 50 bpm) 3%, dyspnoea 3%, proarrhythmia 2%, asthenia 2% and dizziness 2%. Chemical Name: The active ingredient sotalol hydrochloride is the hydrochloride salt of (RS)- 4'-(1-hydroxy-2-isopropylaminoethyl)-methanesulfonanilide.
Chemical Name: The active ingredient sotalol hydrochloride is the hydrochloride salt of (RS)- 4'-(1-hydroxy-2-isopropylaminoethyl)-methanesulfonanilide.