What is in this leaflet
This leaflet answers some common questions about Briviact.
It does not contain all the available information. It does not take the place of talking to your doctor or pharmacist.
All medicines have risks and benefits. Your doctor has weighed the risks of you taking Briviact against the benefits they expect it will have for you.
If you have any concerns about taking this medicine, ask your doctor or pharmacist.
Keep this leaflet with the medicine. You may need to read it again.
What Briviact is used for
Briviact tablets and oral solution are used in combination with other medicines to control epilepsy. Epilepsy is a condition where you have repeated seizures. There are many different types of seizures, ranging from mild to severe.
This medicine belongs to a group of medicines called antiepileptics. These medicines are thought to work by controlling brain chemicals which send signals to nerves so that seizures do not happen.
Your doctor may have prescribed this medicine for another reason.
Ask your doctor if you have any questions about why this medicine has been prescribed for you.
There is no evidence that Briviact is addictive.
This medicine is available only with a doctor’s prescription.
Briviact is not recommended for use in children under the age of 4 years as its safety and effectiveness has not been established in this age group.
Before you take Briviact
When you must not take it
Do not take Briviact if you have an allergy to:
- any of the ingredients listed at the end of this leaflet.
Some of the symptoms of an allergic reaction may include:
- shortness of breath
- wheezing or difficulty breathing
- swelling of the face, lips, tongue or other parts of the body
- rash, itching or hives on the skin.
If you are not sure whether any of the above conditions apply to you, ask your doctor.
Do not take this medicine after the expiry date printed on the pack.
Do not take this medicine if the packaging is torn or shows signs of tampering. If it has expired or is damaged, return to your pharmacist for disposal.
If you are not sure whether you should start taking this medicine, talk to your doctor or pharmacist.
Before you start to take it
Tell your doctor or pharmacist if you have allergies to:
- any other medicines, especially barbiturates (such as phenobarbitone) or any other antiepileptic medicines (such as carbamazepine, lamotrigine or levetiracetam)
- any other substances, such as foods, preservatives or dyes.
Tell your doctor if you have, or have had, any medical conditions, especially the following:
- kidney problems
- liver problems.
Tell your doctor if you are pregnant or intend to become pregnant. Briviact may affect your developing baby if you take it during pregnancy. However, it is very important to control your seizures while you are pregnant. Your doctor will outline and weigh up all the risks and benefits of taking Briviact during pregnancy to help decide whether or not you should take it.
Tell your doctor if you are breastfeeding or plan to breastfeed. Your doctor will discuss the risks and benefits of using Briviact if you are breastfeeding.
If you have not told your doctor or pharmacist about any of the above, tell them before you start taking Briviact.
Taking other medicines
Tell your doctor or pharmacist if you are taking any other medicines, including any that you buy without a prescription from your pharmacy, supermarket or health food shop.
Some medicines and Briviact may interfere with each other. These include:
- rifampicin, a medicine used to treat tuberculosis
Briviact does not interact with the oral contraceptive pill.
However, you may be given Briviact together with other antiepileptic medicines that do interact and may affect the effectiveness of your contraceptive. Your doctor may advise you to use an additional method of contraception if you take Briviact with other antiepileptic medicines.
How to take Briviact
How much to take
Follow all directions given to you by your doctor carefully. They may differ from the information contained in this leaflet.
Your doctor will tell you how much Briviact you will need to take each day. This may depend on your condition and whether or not you are taking any other medicines.
If you do not understand the instructions on the pack, ask your doctor or pharmacist for help.
How to take it
Tablets
Swallow Briviact tablets whole with a glass of water.
Oral Solution
- Press the cap and turn it anticlockwise to open the bottle.

- Separate the adaptor from the syringe.

- Insert the adaptor into the bottle neck. Ensure it is well fixed.

- Take the syringe and put it in the adaptor opening.

- Turn the bottle upside down.

Fill the syringe with a small amount of solution by pulling the piston down (5A), then push the piston upward in order to remove any possible bubble (5B). Pull the piston down to the graduation mark corresponding to the quantity in milliliters (mL) prescribed by your doctor (5C)



- Turn the bottle the right way up (6A). Remove the syringe from the adaptor (6B).


- Empty the contents of the syringe in a glass of water by pushing the piston to the bottom of the syringe. Drink the whole contents of the glass. Close the bottle with the plastic screw cap.

- Wash the syringe with water only

When to take it
Take Briviact twice a day, once in the morning and once at night. Take it at about the same time each day. Taking your medicine at the same time each day will have the best effect. It will also help you remember when to take it.
It does not matter if you take this medicine before or after food.
If you forget to take it
Contact your doctor if you have missed one or more doses.
Do not take a double dose to make up for the dose that you missed. This may increase the chance of you getting an unwanted side effect.
If you are not sure what to do, ask your doctor or pharmacist.
If you have trouble remembering to take your medicine, ask your pharmacist for some hints.
How long to take it
Most antiepileptic medicines take time to work, so do not be discouraged if you do not feel better straight away.
Continue taking your medicine for as long as your doctor tells you to. This medicine helps control your condition, but does not cure it. Therefore you must take your medicine every day, even if you feel well.
Do not stop taking Briviact, or change the dosage, without checking with your doctor. Do not let yourself run out of medicine over the weekend or on holidays. Stopping Briviact suddenly may cause unwanted side effects or make your condition worse. Your doctor will slowly reduce your dose before you can stop taking it completely.
If you take too much (overdose)
Immediately telephone your doctor or the Poisons Information Centre (telephone in Australia 13 11 26), or go to Accident and Emergency at your nearest hospital if you think that you or anyone else may have taken too much Briviact. Do this even if there are no signs of discomfort or poisoning. You may need urgent medical attention.
Symptoms of overdose may include feeling dizzy or drowsy.
While you are using Briviact
Things you must do
Tell your doctor immediately if you notice an increase in seizures or a change in the type of seizures you usually have.
Tell your doctor immediately if you have symptoms of depression or thoughts of harming yourself.
Tell any other doctors, dentists, and pharmacists who are treating you that you are taking this medicine.
If you are about to be started on any new medicine, tell your doctor, dentist or pharmacist that you are taking Briviact.
Before you have any surgery or emergency treatment, tell your doctor or dentist that you are taking Briviact.
Tell your doctor if you feel Briviact is not helping your condition. Your doctor may need to change your medicine.
Tell your doctor if, for any reason, you have not taken this medicine exactly as prescribed. Otherwise, your doctor may change your treatment unnecessarily.
If you become pregnant while taking this medicine, tell your doctor.
Be sure to keep all of your doctor’s appointments so that your progress can be checked. Your doctor will check your progress and may want to take some tests from time to time. This helps to prevent unwanted side effects.
Things you must not do
Do not give Briviact to anyone else, even if their symptoms seem similar to yours or they have the same condition as you.
Do not take Briviact to treat any other complaints unless your doctor tells you to.
Do not stop taking Briviact or change the dosage unless your doctor tells you to. Stopping Briviact suddenly may cause unwanted side effects or make your condition worse.
Things to be careful of
Be careful driving or operating machinery until you know how Briviact affects you.
As with other antiepileptic medicines Briviact may cause dizziness or drowsiness.
If you are feeling dizzy or drowsy, do not drive a car, operate machinery, or do anything else that could be dangerous.
Combining this medicine with alcohol is not recommended. If you drink alcohol while taking Briviact the negative effects of alcohol may be increased.
Side effects
Tell your doctor or pharmacist as soon as possible if you do not feel well while you are taking Briviact.
This medicine helps most people with epilepsy but it may have unwanted side effects in a few people. All medicines can have side effects. Sometimes they are serious, most of the time they are not. You may need medical treatment if you get some of the side effects.
Do not be alarmed by this list of side effects. You may not experience any of them.
Ask your doctor or pharmacist to answer any questions you may have.
If you get any side effects, do not stop taking Briviact without first talking to your doctor or pharmacist.
Tell your doctor or pharmacist if you notice any of the following and they worry you:
- flu and upper respiratory tract infections
- cough
- dizziness
- nausea (feeling sick) or vomiting
- constipation
- feeling tired, drowsy or sleepy
The above list includes the more common side effects of your medicine. They are mostly mild and short-lived.
Tell your doctor as soon as possible if you notice any of the following:
- feelings of depression, anxiety or nervousness
- feeling aggressive
- spinning sensations
- recurrent infections
The above list includes serious side effects that may require medical attention.
If any of the following happen, tell your doctor immediately or go to Accident and Emergency at your nearest hospital:
- thoughts of harming yourself
- more frequent or more severe seizures
- shortness of breath
- wheezing or difficulty breathing
- swelling of the face, lips, tongue or other parts of the body
- rash, itching or hives on the skin.
The above list includes more serious side effects. You may need urgent medical attention or hospitalisation.
Tell your doctor if you notice anything else that is making you feel unwell. Other side effects not listed above may happen in some people.
After using Briviact
Storage
Keep your medicine in the pack until it is time to take them. If you take the tablets out of the pack they will not keep well.
Keep your tablets & oral solution in a cool dry place where the temperature stays below 30°C.
Do not store Briviact or any other medicine in the bathroom or near a sink.
Do not leave your medicine on a window sill or in the car on hot days. Heat and dampness can destroy some medicines.
Keep Briviact where children cannot reach it. A locked cupboard at least one-and-a-half metres above the ground is a good place to store medicines.
Disposal
If your doctor tells you to stop taking this medicine or the expiry date has passed, ask your pharmacist what to do with any medicine that is left over.
Dispose of any unused oral solution within 5 months of opening the bottle.
Product description
What it looks like
Tablets
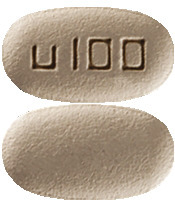
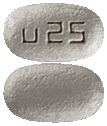
Briviact tablets are available in five strengths:
- 10 mg – White to off white, round, film-coated, and debossed with "u10" on one side.
- 25 mg – Grey, oval, film-coated, and debossed with "u25" on one side.
- 50 mg – Yellow, oval, film-coated, and debossed with "u50" on one side.
- 75 mg – Purple, oval, film-coated, and debossed with “u75” on one side.
- 100 mg - Green-grey, oval, film-coated, and debossed with “u100” on one side.
Oral Solution
Briviact oral solution is packed in a 300 mL glass bottle and is available as 10 mg/mL strength. The pack also contains a 10 mL oral syringe and an adaptor for the syringe.
Ingredients
Tablets
Each Briviact tablet contains either 10 mg, 25 mg, 50 mg, 75 mg, 100 mg of brivaracetam as the active ingredient.
Other ingredients in Briviact tablets include:
- croscarmellose sodium
- lactose monohydrate
- betadex
- lactose
- magnesium stearate
- polyvinyl alcohol
- purified talc
- macrogol 3350
- titanium dioxide
The following strengths also contain:
- 25 mg - iron oxide yellow, iron oxide black
- 50 mg - iron oxide yellow, iron oxide red
- 75 mg - iron oxide yellow, iron oxide red, iron oxide black
- 100 mg - iron oxide yellow, iron oxide black
Briviact tablets do not contain sucrose, gluten, tartrazine or any other azo dyes.
Briviact tablets contain lactose.
Oral Solution
Briviact oral solution contains the following ingredients: sodium citrate, citric acid anhydrous, methyl hydroxybenzoate, carmellose sodium, sucralose, sorbitol solution (70 percent)(crystallising), glycerol, raspberry flavour 7557-A and purified water.
Australian Sponsor:
UCB Pharma
A division of UCB Australia Pty Ltd
Level 1, 1155 Malvern Road
Malvern Vic 3144
Australia
Briviact 10 mg tablets
- AUST R 243794
Briviact 25 mg tablets
- AUST R 243796
Briviact 50 mg tablets
- AUST R 243797
Briviact 75 mg tablets
- AUST R 243798
Briviact 100 mg tablets
- AUST R 243792
Briviact 10 mg/mL oral solution
- AUST R 243793
Date of preparation:
April 2019
BRIVIACT is a registered trademark of UCB Biopharma SPRL
Published by MIMS July 2019



 The relative risk for suicidal thoughts or behaviour was higher in clinical trials for epilepsy than in clinical trials for psychiatric or other conditions, but the absolute risk differences were similar for the epilepsy and psychiatric indications.
The relative risk for suicidal thoughts or behaviour was higher in clinical trials for epilepsy than in clinical trials for psychiatric or other conditions, but the absolute risk differences were similar for the epilepsy and psychiatric indications. Brivaracetam is a moderate reversible inhibitor of epoxide hydrolase resulting in an increased concentration of carbamazepine epoxide, an active metabolite of carbamazepine. In controlled studies, the carbamazepine epoxide plasma concentration increased by a mean of 37%, 62% and 98% with little variability at brivaracetam doses of 50 mg/day, 100 mg/day and 200 mg/day respectively. No toxicity was observed, however, if tolerability issues arise when coadministered, carbamazepine dose reduction should be considered.
Brivaracetam is a moderate reversible inhibitor of epoxide hydrolase resulting in an increased concentration of carbamazepine epoxide, an active metabolite of carbamazepine. In controlled studies, the carbamazepine epoxide plasma concentration increased by a mean of 37%, 62% and 98% with little variability at brivaracetam doses of 50 mg/day, 100 mg/day and 200 mg/day respectively. No toxicity was observed, however, if tolerability issues arise when coadministered, carbamazepine dose reduction should be considered.
 Figure 1 shows the percentage of patients (excluding patients with concomitant levetiracetam) by category of reduction from baseline in partial onset seizure frequency per 28 days across all 3 studies. Patients with more than a 25% increase in partial onset seizure are shown at left as "worse". Patients with an improvement in percent reduction from baseline in partial onset seizure frequency are shown in the 4 right-most categories. The percentages of patients with at least a 50% reduction in seizure frequency were 20.3%, 34.2%, 39.5%, and 37.8% for placebo, 50 mg/day, 100 mg/day, and 200 mg/day, respectively.
Figure 1 shows the percentage of patients (excluding patients with concomitant levetiracetam) by category of reduction from baseline in partial onset seizure frequency per 28 days across all 3 studies. Patients with more than a 25% increase in partial onset seizure are shown at left as "worse". Patients with an improvement in percent reduction from baseline in partial onset seizure frequency are shown in the 4 right-most categories. The percentages of patients with at least a 50% reduction in seizure frequency were 20.3%, 34.2%, 39.5%, and 37.8% for placebo, 50 mg/day, 100 mg/day, and 200 mg/day, respectively.

