SUMMARY CMI
CADIVAST®
Consumer Medicine Information (CMI) summary
The full CMI on the next page has more details. If you are worried about taking this medicine, speak to your doctor or pharmacist.
1. Why am I taking CADIVAST?
CADIVAST contains the active ingredient amlodipine besilate and atorvastatin calcium trihydrate. It is used to treat high blood pressure and high cholesterol (fat in the blood) and angina (a certain type of chest pain). CADIVAST is also used to help reduce the risk of having a heart attack or stroke in people who have high blood pressure and coronary heart disease (CHD) or who are at risk of CHD (for example, if they have diabetes, a history of stroke, or small blood vessel disease). For more information, see Section 1. Why am I taking CADIVAST? in the full CMI.
2. What should I know before I take CADIVAST?
Do not use if you have ever had an allergic reaction to CADIVAST or any of the ingredients listed at the end of the CMI.
Talk to your doctor if you have any other medical conditions, take any other medicines, or are pregnant or plan to become pregnant or are breastfeeding. For more information, see Section 2. What should I know before I take CADIVAST? in the full CMI.
3. What if I am taking other medicines?
Some medicines may interfere with CADIVAST and affect how it works.
A list of these medicines is in Section 3. What if I am taking other medicines? in the full CMI.
4. How do I take CADIVAST?
CADIVAST is taken once a day. Your doctor will decide which strength is suitable for you. More instructions can be found in Section 4. How do I take CADIVAST? in the full CMI.
5. What should I know while taking CADIVAST?
| Things you should do |
|
| Things you should not do |
|
| Driving or using machines |
|
| Drinking alcohol |
|
| Looking after your medicine |
|
For more information, see Section 5. What should I know while taking CADIVAST? in the full CMI.
6. Are there any side effects?
Speak to your doctor if you have any of these: headache; flushing; dizziness; tiredness or weakness; drowsiness or sleepiness; stomach pain or nausea (feeling sick); constipation, diarrhoea, wind; heartburn, indigestion; urine infection; stuffy or runny nose; nose bleeds; rash. Call your doctor straight away or go straight to the Emergency Department at your nearest hospital if you have any of these: symptoms of allergy such as skin rash, itching, swelling of the face, lips, mouth, throat or neck which may cause difficulty in swallowing and breathing; shortness of breath; unexpected muscle pain, tenderness or weakness not caused by exercise (particularly if you also feel unwell or have a fever); changes in heart beat either fast, slow or irregular; chest pain; sudden severe headache which may be accompanied by nausea, vomiting, loss of sensation, tingling in any part of the body or ringing in the ears; severe blisters and bleeding of the lips, eyes, mouth, nose or genitals; severe upper stomach pain often with nausea and vomiting. For more information, including what to do if you have any side effects, see Section 6. Are there any side effects? in the full CMI.
FULL CMI
CADIVAST®
Active ingredient(s): amlodipine (as besilate) and atorvastatin (as calcium trihydrate)
Consumer Medicine Information (CMI)
This leaflet provides important information about taking CADIVAST. You should also speak to your doctor or pharmacist if you would like further information or if you have any concerns or questions about taking CADIVAST.
Where to find information in this leaflet:
1. Why am I taking CADIVAST?
2. What should I know before I take CADIVAST?
3. What if I am taking other medicines?
4. How do I take CADIVAST?
5. What should I know while taking CADIVAST?
6. Are there any side effects?
7. Product details
1. Why am I taking CADIVAST?
CADIVAST contains the active ingredient amlodipine and atorvastatin.
Amlodipine belongs to a group of medicines called calcium channel blockers. They work by relaxing your blood vessels, making it easier for your heart to pump blood around the body and help increase the supply of blood and oxygen to your heart. Calcium channel blockers do not change the amount of calcium in your blood or bones.
Atorvastatin belongs to a group of medicines called statins. It works by reducing the amount of cholesterol made by the liver. It reduces the 'bad' cholesterol and can raise the 'good' cholesterol. Atorvastatin also helps to protect you from a heart attack or stroke.
CADIVAST may be used alone, or in combination with other medicines, to treat your condition.
CADIVAST is used to treat:
- high blood pressure and high cholesterol (fat in the blood)
- angina (a certain type of chest pain)
- people who have high blood pressure and coronary heart disease (CHD) or who are at risk of CHD (for example, if they have diabetes, a history of stroke, or small blood vessel disease). In these people, CADIVAST is used to help reduce the risk of having a heart attack or stroke.
Ask your doctor if you have any questions about why this medicine has been prescribed for you.
Your doctor may have prescribed it for another reason.
This medicine is not addictive.
Use in children
There is not enough information to recommend the use of this medicine for children.
Use in the elderly
If you are 65 years or older, you should be especially careful while taking CADIVAST. Report any side effects promptly to your doctor.
Some people in this age group may be more likely to experience side effects such as swelling of the feet and ankles, muscle cramps and dizziness.
What is high blood pressure?
There are usually no symptoms of high blood pressure (hypertension). The only way of knowing that you have hypertension is to have your blood pressure checked on a regular basis. If high blood pressure is not treated it can lead to serious health problems.
What is cholesterol?
Everyone has cholesterol in their blood. It is a type of blood fat needed by the body for things such as building cell lining, making bile acids (which help to digest food) and some hormones. However, too much cholesterol can be a problem.
Cholesterol is present in many foods and is also made in your body by the liver. If your body makes too much cholesterol or you take too much cholesterol in your diet, then your level becomes too high.
High cholesterol is more likely to occur with certain diseases or if you have a family history of high cholesterol.
There are different types of cholesterol. LDL, or low-density lipoprotein, is the 'bad' cholesterol that can block your blood vessels. HDL, or high-density lipoprotein, is the 'good' cholesterol that is thought to remove the 'bad' cholesterol from the blood vessels.
When you have high levels of 'bad' cholesterol in your blood, it may begin to 'stick' to the inside of your blood vessels instead of being carried to the parts of the body where it is needed. Over time, this can form hard areas, also called plaque, on the walls of your blood vessels, making it more difficult for the blood to flow. Sometimes, the plaque can detach from the vessel wall and float in the bloodstream; it can then reach a smaller vessel and completely block it. This blocking of your blood vessels can lead to several types of blood vessel disease, heart attack, angina and stroke.
There is another type of blood fat called triglyceride that is a source of energy. However, high levels of triglyceride can be associated with a low level of 'good' cholesterol and may increase your risk of heart disease.
In some patients, CADIVAST is used to treat high cholesterol and high triglycerides together.
In most people, there are no symptoms of abnormal cholesterol or triglyceride levels. Your doctor can measure your levels with a simple blood test.
What is angina?
Angina is a pain or uncomfortable feeling in the chest, often spreading to the arms or neck, and sometimes to the shoulders and back. The pain of angina is due to a shortage of oxygen to the heart. CADIVAST is used to treat chronic angina.
2. What should I know before I take CADIVAST?
Warnings
Do not take CADIVAST if you:
- are allergic to any medicine containing amlodipine
- are allergic to any medicine containing atorvastatin
- are allergic to any of the ingredients listed at the end of this leaflet.
Some of the symptoms of an allergic reaction may include:
- shortness of breath
- wheezing or difficulty breathing
- swelling of the face, lips, tongue or other parts of the body
- rash, itching or hives on the skin.
Always check the ingredients to make sure you can take this medicine. - have active liver disease
- are pregnant or intend to become pregnant
- are breastfeeding or intend to breastfeed
- are taking the antibiotic fusidic acid hemihydrate which is used to treat infections
- are taking the antivirals glecaprevir/pibrentasvir for the treatment of hepatitis C.
Do not give this medicine to children.
Safety and effectiveness in children have not been established.
Do not take this medicine after the expiry date printed on the pack or if the packaging is torn or shows signs of tampering.
If you are not sure whether you should start taking this medicine, talk to your doctor.
Check with your doctor if you:
- have or have had any of the following medical conditions:
- heart disease such as heart failure
- liver problems
- kidney problems
- muscle pain, tenderness or weakness from other medicines used to treat cholesterol or triglycerides
- vision problems, eye muscle weakness and drooping eyelid
- breathing problems
- a type of stroke called a haemorrhagic stroke or a type of stroke called a lacunar stroke.
If you have had one of these strokes before, this medicine may increase the risk of you having a haemorrhagic stroke. - have allergies to any other medicines, foods, preservatives or dyes
- take medicines for any other condition
- Tell your doctor if you are consuming alcohol regularly.
Your doctor will ask you to have your liver function tested before you start to take CADIVAST.
During treatment, you may be at risk of developing certain side effects. It is important you understand these risks and how to monitor for them. See additional information under Section 6. Are there any side effects?
Pregnancy and breastfeeding
Do not take this medicine if you are pregnant or intend to become pregnant.
Check with your doctor if you are pregnant or intend to become pregnant.
If you are a woman of child-bearing age and are taking this medicine, use a proven method of birth control to avoid pregnancy.
This medicine may affect your developing baby if you take it during pregnancy.
Do not take this medicine if you are breastfeeding or intend to breastfeed.
Talk to your doctor if you are breastfeeding or intend to breastfeed.
This medicine may pass into breast milk and there is a possibility that your baby may be affected.
Your doctor can discuss with you the risks and benefits involved.
If you have not told your doctor about any of the above, tell him/her before you start taking CADIVAST.
3. What if I am taking other medicines?
Tell your doctor or pharmacist if you are taking any other medicines, including any medicines, vitamins or supplements that you buy without a prescription from your pharmacy, supermarket or health food shop.
Some medicines may interfere with CADIVAST and affect how it works.
You may need different amounts of your medicines, or you may need to take different medicines. Your doctor will advise you.
Tell your doctor or pharmacist if you are taking:
- other calcium channel blockers. These medicines include amlodipine which is also in CADIVAST; other calcium channel blockers include medicines with the active ingredient felodipine or nifedipine.
- other statins. These medicines include atorvastatin which is also in CADIVAST. Other statins include medicines with active ingredient fluvastatin, pravastatin, rosuvastatin, simvastatin or simvastatin containing medicines.
Check with your doctor or pharmacist if you are unsure.
Tell your doctor or pharmacist if you are taking any of the following:
- digoxin, a medicine used to treat some heart problems
- the antibiotics erythromycin, clarithromycin, rifampicin or fusidic acid hemihydrate
- phenytoin, a medicine used to treat epilepsy (seizures)
- oral contraceptives for birth control
- other medicines to treat high cholesterol or triglycerides (fats)
- other medicines to treat high blood pressure
- some medicines to treat low potassium
- ciclosporin, tacrolimus, sirolimus or everolimus, medicines used to suppress the immune system
- temsirolimus, a medicine used to treat kidney cancer
- some medicines used to treat some fungal infections, such as ketoconazole or itraconazole
- protease inhibitors for the treatment of HIV infections and/or Hepatitis C, such as efavirenz, fosamprenavir, ritonavir, boceprevir, telaprevir, tipranavir/ritonavir, elbasvir/grazoprevir and simprevir
- HCV non-structural protein 5A (NS5A)/5B (NS5B) inhibitors such as daclatasvir and ledipasvir
- letermovir
- diltiazem, a medicine used to treat angina
- antacids, medicines used to treat reflux or ulcers
- spironolactone, a medicine used to treat high blood pressure and certain types of swelling
- vitamin B3
- colchicine, a medicine used to treat a disease with painful swollen joints caused by uric acid crystals
- ticagrelor, a medicine used to prevent blood clots.
It is also possible that CADIVAST may be affected by some medicines used to treat heart palpitations (or arrhythmias) and St John's Wort.
If you have not told your doctor about any of the above, tell him/her before you start taking CADIVAST.
Your doctor and pharmacist have more information on medicines to be careful with or avoid while taking CADIVAST.
Check with your doctor or pharmacist if you are not sure about what medicines, vitamins or supplements you are taking and if these affect CADIVAST.
4. How do I take CADIVAST?
How much to take
- CADIVAST is taken once a day.
- Your doctor will decide which strength is suitable for you.
This will depend on your blood pressure, cholesterol and triglyceride levels. - Your doctor may need to adjust your dose after your blood pressure and the fat levels in your blood have been checked. It is important that you keep your appointments to have these tests done.
- If you do not understand the instructions on the bottle, ask your doctor or pharmacist for help.
- Follow the instructions provided and use CADIVAST until your doctor tells you to stop.
When to take CADIVAST
- Take your medicine at about the same time each day.
Taking it at the same time each day will have the best effect. It will also help you remember when to take it. - CADIVAST can be taken with or without food.
How to take CADIVAST
- Swallow the tablets whole with a full glass of water.
- Do not crush or chew the tablets.
- Take CADIVAST exactly as your doctor has prescribed.
- Follow all directions given to you by your doctor or pharmacist carefully. They may differ from the information contained in this leaflet.
- Your doctor may discuss with you the need to be on a diet. Follow your agreed diet plan carefully.
How long to take CADIVAST
Take CADIVAST every day and continue taking it for as long as your doctor tells you.
This medicine helps to lower cholesterol levels and blood pressure and control the symptoms of angina but it does not cure your condition.
It is important to keep taking your medicine even if you feel well. If you stop taking CADIVAST, your blood pressure and cholesterol levels may rise again.
If you forget to take CADIVAST
CADIVAST should be taken regularly at the same time each day.
If you miss your dose at the usual time and it is less than 12 hours before your next dose, skip the dose you missed and take your next dose when you are meant to.
Otherwise, take it as soon as you remember, and then go back to taking your medicine as you would normally.
Do not take a double dose to make up for the dose you missed. This may increase the chance of you getting an unwanted side effect.
If you are not sure what to do, ask your doctor or pharmacist.
If you have trouble remembering to take your medicine, ask your pharmacist for some hints.
If you take too much CADIVAST
If you think that you or anyone else may have taken too much CADIVAST, urgent medical attention may be needed.
You should immediately:
- phone the Poisons Information Centre
(Australia telephone 13 11 26) for advice, or - contact your doctor, or
- go to the Emergency Department at your nearest hospital.
You should do this even if there are no signs of discomfort or poisoning.
Keep telephone numbers of these facilities handy.
Symptoms of an overdose may include dizzy, lightheaded or faint and have an irregular heartbeat.
5. What should I know while taking CADIVAST?
Things you should do
- If you are about to be started on any new medicine, remind your doctor and pharmacist that you are taking CADIVAST.
- If you are going to have surgery, tell the surgeon or anaesthetist that you are taking this medicine.
It may affect other medicines used during surgery. - If you are about to have any blood tests, tell your doctor that you are taking this medicine. It may interfere with the results of some tests.
- Keep all of your doctor's appointments so that your progress can be checked.
- Your cholesterol and triglyceride levels and your liver function tests need to be checked regularly while you are taking this medicine.
- A regular blood test to check an enzyme called creatine kinase (CK) may be needed. CK in your blood can rise after muscle injury which can be caused by medicines used to treat cholesterol or triglycerides, such as CADIVAST.
This helps to make sure that CADIVAST is working and to avoid some possible side-effects. - Your blood pressure may also be checked regularly.
Call your doctor straight away if you:
- become pregnant while taking this medicine.
Remind any doctor, dentist or pharmacist you visit that you are taking CADIVAST.
Things you should not do
- Do not take CADIVAST to treat any other complaints unless your doctor tells you to.
- Do not give your medicine to anyone else, even if they have the same condition as you.
- Do not stop taking your medicine or lower the dosage without checking with your doctor.
If you stop taking it suddenly, your condition may worsen or you may have unwanted side effects.
Things to be careful of
- Avoid eating large quantities of grapefruit or drinking large quantities of grapefruit juice.
Grapefruit juice contains one or more components that alter the metabolism of some medicines, including CADIVAST.
Drinking very large quantities (over 1.2 litres) of grapefruit juice each day while taking CADIVAST increases your chance of getting side effects. - If you feel light-headed, dizzy or faint when getting out of bed or standing up, get up slowly.
Standing up slowly, especially when you get up from bed or chairs, will help your body get used to the change in position and blood pressure. If this problem continues or gets worse, talk to your doctor.
Driving or using machines
Be careful before you drive or use any machines or tools until you know how CADIVAST affects you.
CADIVAST may cause dizziness or drowsiness in some people and affect alertness.
If you have any of these symptoms, do not drive, operate machinery or do anything else that could be dangerous.
Drinking alcohol
Avoid drinking large quantities of alcohol. Tell your doctor if you drink alcohol.
Drinking large quantities of alcohol while taking CADIVAST may increase your chance of getting liver problems.
Excessive alcohol intake can raise your cholesterol levels or affect your liver function, which could increase the chance of you getting unwanted side effects.
Your doctor may discuss with you whether you should reduce the amount of alcohol you drink.
Lifestyle measures that help reduce heart disease risk
By following these simple measures, you can further reduce the risk from heart disease.
- Quit smoking and avoid second-hand smoke. Smoking increases the risk of you suffering from heart problems. Your doctor may advise you to stop smoking.
- Limit alcohol intake.
- Enjoy healthy eating by:
- eating plenty of vegetables and fruit
- reducing your saturated fat intake (eat less fatty meats, full fat dairy products, butter, coconut and palm oils, most take-away foods, commercially-baked products)
- reducing your salt intake. Your doctor may advise you to watch the amount of salt in your diet. To reduce your salt intake, avoid using salt at the table or in cooking. - Be active. Progress, over time, to at least 30 minutes of moderate-intensity physical activity on 5 or more days each week. Can be accumulated in shorter bouts of 10 minutes duration. If you have been prescribed anti-angina medicine, carry it with you when being physically active.
- Regular exercise can help lower your cholesterol levels and blood pressure and can strengthen your heart. It is important not to overdo it. Before commencing regular exercise, you should consult your doctor who will suggest the most suitable exercise for you. If you experience any discomfort when exercising, see your doctor.
- Maintain a healthy weight. While you are taking CADIVAST, you may need to follow a diet plan agreed to with your doctor. This may include measures to lose some weight.
- Discuss your lifestyle and lifestyle plans with your doctor.
- For more information and tools to improve your heart health, call Heartline, the Heart Foundation's national telephone information service, on 1300 36 27 87 (local call cost).
Know warning signs of heart attack and what to do:
- Tightness, fullness, pressure, squeezing, heaviness or pain in your chest, neck, jaw, throat, shoulders, arms or back.
- You may also have difficulty breathing, or have a cold sweat or feel dizzy or light headed or feel like vomiting (or actually vomit).
- If you have heart attack warning signs that are severe, get worse or last for 10 minutes even if they are mild, call triple zero (000). Every minute counts.
Looking after your medicine
- Keep your tablets in the pack until it is time to take them.
If you take the tablets out of the pack they may not keep well. - Keep your tablets in a cool dry place where the temperature stays below 25°C.
Follow the instructions in the carton on how to take care of your medicine properly.
Store it in a cool dry place away from moisture, heat or sunlight; for example, do not store it:
- in the bathroom or near a sink, or
- in the car or on window sills.
Heat and dampness can destroy some medicines.
Keep it where young children cannot reach it.
A locked cupboard at least one-and-a-half metres above the ground is a good place to store medicines.
Getting rid of any unwanted medicine
If you no longer need to take this medicine or it is out of date, take it to any pharmacy for safe disposal.
Do not take this medicine after the expiry date.
6. Are there any side effects?
All medicines can have side effects. If you do experience any side effects, most of them are minor and temporary. However, some side effects may need medical attention.
If you are over 65 years of age you may have an increased chance of getting side effects.
Do not be alarmed by the following lists of side effects. You may not experience any of them.
See the information below and, if you need to, ask your doctor or pharmacist if you have any further questions about side effects.
Less serious side effects
| Less serious side effects | What to do |
| Speak to your doctor if you have any of these less serious side effects and they worry you. This list includes the more common side effects of your medicine. They are usually mild and short-lived. |
Serious side effects
| Serious side effects | What to do |
| Call your doctor straight away if you notice any of these serious side effects. This list includes serious side effects that may require medical attention. |
Very serious side effects
| Very serious side effects | What to do |
| Call your doctor straight away, or go straight to the Emergency Department at your nearest hospital if you notice any of these very serious side effects. This list includes very serious side effects. You may need urgent medical attention or hospitalisation. |
Tell your doctor or pharmacist if you notice anything else that may be making you feel unwell.
Other side effects not listed here may occur in some people.
Ask your doctor or pharmacist to answer any questions you may have.
Reporting side effects
After you have received medical advice for any side effects you experience, you can report side effects to the Therapeutic Goods Administration online at www.tga.gov.au/reporting-problems. By reporting side effects, you can help provide more information on the safety of this medicine.
Always make sure you speak to your doctor or pharmacist before you decide to stop taking any of your medicines.
7. Product details
This medicine is only available with a doctor's prescription.
What CADIVAST contains
| Active ingredient (main ingredient) | amlodipine besilate 5 mg or 10 mg and atorvastatin calcium trihydrate 10 mg, 20 mg, 40 mg or 80 mg per tablet |
| Other ingredients (inactive ingredients) |
|
| Potential allergens | Soya bean products |
Do not take this medicine if you are allergic to any of these ingredients.
What CADIVAST looks like
CADIVAST 5/10 mg tablet: A white to off-white, film-coated, oval, biconvex tablet debossed with “AA 4” on one side of the tablet and “M” on the other side. (AUST R 199213)
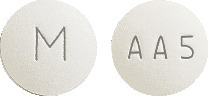
CADIVAST 5/20 mg tablet: A white to off-white, film-coated, round, biconvex tablet debossed with “AA 5” on one side of the tablet and “M” on the other side. (AUST R 199222)
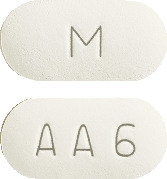
CADIVAST 5/40 mg tablet: A white to off-white, film-coated, capsule shaped, biconvex tablet debossed with “AA 6” on one side of the tablet and “M” on the other side. (AUST R 199214)
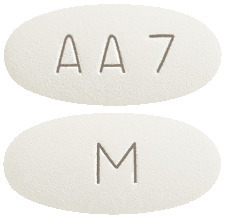
CADIVAST 5/80 mg tablet: A white to off-white, film-coated, oval, biconvex tablet debossed with “AA 7” on one side of the tablet and “M” on the other side. (AUST R 199210)
CADIVAST 10/10 mg tablet: A blue, film-coated, barrel shaped, biconvex tablet debossed with “AA 8” on one side of the tablet and “M” on the other side. (AUST R 199215)
CADIVAST 10/20 mg tablet: A blue, film-coated, oval, biconvex tablet debossed with “AA 9” on one side of the tablet and “M” on the other side. (AUST R 199223)
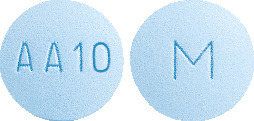
CADIVAST 10/40 mg tablet: A blue, film-coated, round, biconvex tablet debossed with “AA 10” on one side of the tablet and “M” on the other side. (AUST R 199225)
CADIVAST 10/80 mg tablet: A blue, film-coated, capsule shaped, biconvex tablet debossed with “AA 11” on one side of the tablet and “M” on the other side. (AUST R 199217)
CADIVAST is available in bottles of 30 tablets.
Who distributes CADIVAST
Alphapharm Pty Ltd trading as Viatris
Level 1, 30 The Bond
30-34 Hickson Road
Millers Point NSW 2000
www.viatris.com.au
Phone: 1800 274 276
This leaflet was prepared in January 2024.
CADIVAST® is a Viatris company trade mark
CADIVAST_cmi\Jan24/01
Published by MIMS March 2024





 The safety profile of the combination product is consistent with the adverse events previously reported for amlodipine and/or atorvastatin that are detailed below.
The safety profile of the combination product is consistent with the adverse events previously reported for amlodipine and/or atorvastatin that are detailed below. Other adverse experiences which were not clearly dose related but which were reported with an incidence greater than 1.0% in placebo controlled clinical trials include the following (see Table 3).
Other adverse experiences which were not clearly dose related but which were reported with an incidence greater than 1.0% in placebo controlled clinical trials include the following (see Table 3). The following events occurred in ≤ 1% but > 0.1% of patients in controlled clinical trials or under conditions of open trials or marketing experience where a causal relationship is uncertain; they are listed to alert the physician to a possible relationship.
The following events occurred in ≤ 1% but > 0.1% of patients in controlled clinical trials or under conditions of open trials or marketing experience where a causal relationship is uncertain; they are listed to alert the physician to a possible relationship. In the AVALON double blind, placebo controlled study, a total of 847 patients with comorbid hypertension and dyslipidaemia received once daily placebo, 5 mg amlodipine, 10 mg of atorvastatin or the combination of 5 mg amlodipine and 10 mg atorvastatin. The primary objective of the study was the percentage of patients on the combination of amlodipine and atorvastatin reaching JNC VI and NCEP III goals compared to atorvastatin, amlodipine and placebo alone. The results following 8 weeks of treatment are summarised in Table 5. Significantly more patients treated with the combination (45.5%) reached both their blood pressure (BP) and LDL-C goals compared to amlodipine or atorvastatin alone. Amlodipine besilate and atorvastatin calcium trihydrate tablet was not studied in patients with decompensated chronic cardiac failure or postmyocardial infarction (within 3 to 6 months).
In the AVALON double blind, placebo controlled study, a total of 847 patients with comorbid hypertension and dyslipidaemia received once daily placebo, 5 mg amlodipine, 10 mg of atorvastatin or the combination of 5 mg amlodipine and 10 mg atorvastatin. The primary objective of the study was the percentage of patients on the combination of amlodipine and atorvastatin reaching JNC VI and NCEP III goals compared to atorvastatin, amlodipine and placebo alone. The results following 8 weeks of treatment are summarised in Table 5. Significantly more patients treated with the combination (45.5%) reached both their blood pressure (BP) and LDL-C goals compared to amlodipine or atorvastatin alone. Amlodipine besilate and atorvastatin calcium trihydrate tablet was not studied in patients with decompensated chronic cardiac failure or postmyocardial infarction (within 3 to 6 months).
 In a long-term (follow-up at least 6 months, mean 13.8 months) placebo controlled mortality/morbidity study of amlodipine 5 to 10 mg in 1153 patients with NYHA classes III (n = 931) or IV (n = 222) heart failure on stable doses of diuretics, digoxin and angiotensin converting enzyme (ACE) inhibitors, amlodipine had no effect on the primary endpoint of the study which was the combined endpoint of all cause mortality and cardiac morbidity (as defined by life threatening arrhythmia, acute myocardial infarction, or hospitalisation for worsened heart failure), or on NYHA classification, or symptoms of heart failure. Total combined all-cause mortality and cardiac morbidity events were 222/571 (39%) for patients on amlodipine and 246/583 (42%) for patients on placebo: the cardiac morbid events represented about 25% of the endpoints in the study.
In a long-term (follow-up at least 6 months, mean 13.8 months) placebo controlled mortality/morbidity study of amlodipine 5 to 10 mg in 1153 patients with NYHA classes III (n = 931) or IV (n = 222) heart failure on stable doses of diuretics, digoxin and angiotensin converting enzyme (ACE) inhibitors, amlodipine had no effect on the primary endpoint of the study which was the combined endpoint of all cause mortality and cardiac morbidity (as defined by life threatening arrhythmia, acute myocardial infarction, or hospitalisation for worsened heart failure), or on NYHA classification, or symptoms of heart failure. Total combined all-cause mortality and cardiac morbidity events were 222/571 (39%) for patients on amlodipine and 246/583 (42%) for patients on placebo: the cardiac morbid events represented about 25% of the endpoints in the study. In three further trials, 1,148 patients with either heterozygous familial hypercholesterolaemia, non-familial forms of hypercholesterolaemia, or mixed dyslipidaemia were treated with atorvastatin for one year. The results were consistent with those of the dose response study and were maintained for the duration of therapy.
In three further trials, 1,148 patients with either heterozygous familial hypercholesterolaemia, non-familial forms of hypercholesterolaemia, or mixed dyslipidaemia were treated with atorvastatin for one year. The results were consistent with those of the dose response study and were maintained for the duration of therapy. The primary endpoint examined in ASCOT was the rate of fatal coronary heart disease or non-fatal myocardial infarction over 3.3 years. These coronary events occurred in 1.9% of atorvastatin treated patients compared to 3% of placebo treated patients, a relative risk reduction of 36% (p = 0.0005) (Table 8). Although this difference was statistically significant for the whole trial population, this difference was not statistically significant in specified subgroups such as diabetes, patients with left ventricular hypertrophy (LVH), previous vascular disease or metabolic syndrome.
The primary endpoint examined in ASCOT was the rate of fatal coronary heart disease or non-fatal myocardial infarction over 3.3 years. These coronary events occurred in 1.9% of atorvastatin treated patients compared to 3% of placebo treated patients, a relative risk reduction of 36% (p = 0.0005) (Table 8). Although this difference was statistically significant for the whole trial population, this difference was not statistically significant in specified subgroups such as diabetes, patients with left ventricular hypertrophy (LVH), previous vascular disease or metabolic syndrome.

 Chemical name: 3-ethyl, 5-methyl (4RS)-2-[(2-aminoethoxy)methyl]-4-(2-chlorophenyl)-6-methyl-1,4-dihydropyridine-3,5-dicarboxylate benzene sulfonate.
Chemical name: 3-ethyl, 5-methyl (4RS)-2-[(2-aminoethoxy)methyl]-4-(2-chlorophenyl)-6-methyl-1,4-dihydropyridine-3,5-dicarboxylate benzene sulfonate. Chemical name: (3R, 5R)-7-[2-(4-fluorophenyl)-5-(1-methylethyl)-3-phenyl-4-(phenylcarbamoyl)-1H-pyrrol-1-yl]-3,5-dihydroxyheptanoate calcium trihydrate.
Chemical name: (3R, 5R)-7-[2-(4-fluorophenyl)-5-(1-methylethyl)-3-phenyl-4-(phenylcarbamoyl)-1H-pyrrol-1-yl]-3,5-dihydroxyheptanoate calcium trihydrate.