What is in this leaflet
This leaflet answers some common questions about DISTAPH.
It does not contain all the available information. It does not take the place of talking to your doctor or pharmacist.
All medicines have benefits and risks. Your doctor has weighed the risks of you taking DISTAPH against the benefits expected for you.
If you have any concerns about taking this medicine, talk to your doctor or pharmacist.
Keep this leaflet with your medicine. You may need to read it again.
What DISTAPH is used for
DISTAPH is used to treat infections in different parts of the body caused by bacteria.
DISTAPH is an antibiotic that belongs to a group of medicines called penicillins. These medicines work by killing the bacteria that are causing your infection.
DISTAPH will not work against infections caused by viruses, such as colds or flu.
Ask your doctor if you have any questions about why DISTAPH has been prescribed for you. Your doctor may have prescribed DISTAPH for another purpose.
DISTAPH is not recommended for use in newborn infants as its safety and effectiveness have not been established in this age group.
DISTAPH is available only with a doctor's prescription.
There is no evidence that DISTAPH is addictive.
Before you take DISTAPH
When you must not take it
Do not take DISTAPH if you have had an allergic reaction to:
- medicines containing dicloxacillin or any other penicillin e.g. amoxicillin
- cephalosporin antibiotics
- any of the ingredients listed at the end of this leaflet
Some of the symptoms of an allergic reaction may include skin rash, itching or hives, swelling of the face, lips, mouth, throat or other parts of the body, shortness of breath, wheezing or troubled breathing.
Check with your doctor or pharmacist if you are not sure about any of the above.
Do not take DISTAPH if the expiry date (EXP.) printed on the bottle has passed If you take this medicine after the expiry date, it may not work as well.
Do not take DISTAPH if the packaging shows signs of tampering or the capsules do not look quite right.
Before you start to take it
Be sure to tell your doctor if you have had any type of allergic reaction to:
- other penicillins, e.g. amoxicillin
- cephalosporin antibiotics
You may have an increased chance of being allergic to DISTAPH if you are allergic to cephalosporins.
Tell your doctor if you are allergic to any other medicines, foods, dyes or preservatives.
Tell your doctor if you have, or have had, any other health problems or medical conditions, especially the following:
- stomach problems such as feeling sick (nausea), vomiting, indigestion
- problems with food absorption
- liver problems
- kidney problems
- cystic fibrosis
Your doctor may want to take special care or adjust your dose if you have any of these conditions.
Tell your doctor if you are over 55 years old. Some side effects occur more frequently in this age group. Your doctor will discuss the risks and benefits of taking DISTAPH with you.
Tell your doctor if you are pregnant or plan to become pregnant. Your doctor will discuss the risks and benefits of taking DISTAPH during pregnancy.
Tell your doctor if you are breastfeeding or wish to breastfeed. Like many other medicines, DISTAPH can pass into breast milk. Your doctor will discuss the risks and benefits of taking DISTAPH when breastfeeding.
If you have not told your doctor or pharmacist about any of the above, tell them before you start taking DISTAPH.
Taking other medicines
Tell your doctor if you are taking any other medicines, including any that you buy without a prescription from a pharmacy, supermarket or health food shop.
Some medicines may be affected by DISTAPH, or may affect how well it works. These include:
- probenecid, a medicine used to treat gout
- warfarin, a medicine used to prevent blood clots
- phenytoin, a medicine used to treat epilepsy
Your doctor can tell you what to do if you are taking any of these medicines.
If you are not sure whether you are taking any of these medicines, check with your doctor or pharmacist. Your doctor and pharmacist have more information on medicines to be careful with or avoid while taking DISTAPH.
How to take DISTAPH
Follow all directions given to you by your doctor and pharmacist carefully. They may differ from the information contained in this leaflet.
If you do not understand the instructions on the bottle, ask your doctor or pharmacist.
How much to take
The dose varies from person to person.
Your doctor will tell you how much DISTAPH you need to take each day.
For most infections, the usual dose for adults and children over 12 years is 250 mg to 500 mg every 6 hours.
How to take DISTAPH
Swallow the capsules whole with a glass of water.
Take DISTAPH on an empty stomach, 1 to 2 hours before food. Taking the capsules on an empty stomach means that more of the medicine is absorbed into your body.
Take your medicine at about the same time each day. Taking it at the same time each day will have the best effect. It will also help you remember when to take it.
How long to take DISTAPH for
Keep taking DISTAPH until you finish your bottle, or for as long as your doctor recommends.
Do not stop taking DISTAPH, even if you feel better after a few days, unless advised by your doctor. Your infection may not clear completely if you stop taking your medicine too soon.
If you forget to take DISTAPH
If it is almost time for your next dose, skip the dose you missed and take your next dose when you are meant to.
Otherwise, take it as soon as you remember, and then go back to taking your capsules as you would normally.
Do not take a double dose to make up for the dose you missed. This may increase the chance of you getting an unwanted side effect.
If you miss more than one dose, or are not sure what to do, ask your doctor or pharmacist.
If you take too much DISTAPH (overdose)
Immediately telephone your doctor, or the Poisons Information Centre (telephone 13 11 26), if you think you or anyone else may have taken too much DISTAPH.
Do this even if there are no signs of discomfort or poisoning. You may need urgent medical attention
While you are taking DISTAPH
Things you must do
Tell all the doctors, dentists and pharmacists who are treating you that you are taking DISTAPH.
Before starting any new medicine, tell your doctor or pharmacist that you are taking DISTAPH.
If the symptoms of your infection do not improve within a few days, or if they become worse, tell your doctor.
If you get severe diarrhoea, tell your doctor or pharmacist immediately. Do this even if it occurs several weeks after stopping DISTAPH. Diarrhoea may mean that you have a serious condition affecting your bowel. You may need urgent medical care.
Do not take any medicine to stop your diarrhoea without first checking with your doctor.
If you develop a yellow discolouration of the skin or eyes, your stools become pale and you feel unwell, tell your doctor immediately. These symptoms may mean that you have a serious problem with your liver. You may need urgent medical care.
If you get a sore, white mouth or tongue while taking or soon after stopping DISTAPH, tell your doctor. Also tell your doctor if you get vaginal itching or discharge. This may mean you have a fungal infection called thrush. Sometimes, the use of DISTAPH allows fungi to grow and these symptoms to occur. DISTAPH does not work against fungi.
If you are taking more than one or two courses of DISTAPH, you may need to have tests to check your liver, kidneys or blood. Always follow your doctor's instructions and have the tests performed as directed.
Things you must not do
Do not stop taking DISTAPH, even if you feel better after a few days, unless advised to by your doctor. If you stop taking DISTAPH too soon, your infection may not clear completely and your symptoms may return.
Do not use DISTAPH to treat any other conditions unless advised to by your doctor.
Do not give this medicine to anyone else, even if their symptoms seem similar to yours.
Side effects
Tell your doctor or pharmacist as soon as possible if you do not feel well while you are taking DISTAPH. DISTAPH treats infections in most people, but it may have unwanted side effects in some people.
All medicines can have side effects. Sometimes they are serious, most of the time they are not. You may need medical treatment if you get some of the side effects.
Ask your doctor or pharmacist to answer any questions you may have.
Do not be alarmed by this list of possible side effects. You may not experience any of them.
While you are taking DISTAPH
Tell your doctor if you notice any of the following and they worry you:
- nausea (feeling sick), vomiting, stomach upset, wind, loose stools
- oral thrush (white, furry sore tongue and mouth)
- vaginal thrush (sore and itchy vagina, vaginal discharge)
Tell your doctor immediately or go to casualty at the nearest hospital if you notice any of the following:
- watery and severe diarrhoea, which may also be bloody
- blood in the urine
- excess protein in the urine
- severe stomach cramps
- yellowing of the skin or eyes (jaundice), pale stools
- kidney problems
Stop taking DISTAPH and tell your doctor immediately or go to casualty at the nearest hospital if any of the following happen:
- any type of skin rash, itching or hives
- swelling of the face, lips, mouth, throat or other parts of the body
- shortness of breath, wheezing or difficulty breathing
After you have finished taking DISTAPH
Tell your doctor immediately if you notice any of the following, even if they occur several weeks after stopping treatment with DISTAPH:
- watery and severe diarrhoea, which may also be bloody
- severe stomach cramps
This is not a complete list of all possible side effects. Others may occur in some people and there may be some side effects not yet known.
Tell your doctor if you notice anything that is making you feel unwell while you are taking, or soon after you have finished taking DISTAPH, even if it is not on this list.
After taking DISTAPH
Storage
Keep DISTAPH where children cannot reach it. A locked cupboard at least one-and-a-half metres above the ground is a good place to store medicines.
Keep your capsules in the bottle until it is time to take them. If you take the capsules out of the bottle they will not keep well.
Keep DISTAPH in a cool dry place where the temperature stays below 25°C.
Do not keep DISTAPH or any other medicine in the bathroom or near a sink.
Do not leave DISTAPH in the car or on window sills. Heat and dampness can destroy some medicines.
Disposal
If your doctor tells you to stop taking DISTAPH, or your medicine has passed its expiry date, ask your pharmacist what to do with any capsules that are left over.
Product description
What it looks like
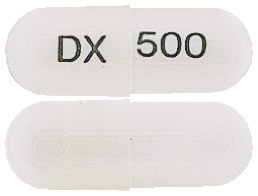
DISTAPH comes in two strengths of capsules:
- DISTAPH 250 - Size 2 capsule with white opaque body and cap, printed 'DX' on the cap and ‘250’ on the body in black
- DISTAPH 500 - Size 0 capsule with white opaque body and cap, printed 'DX' on the cap and '500' on the body in black
Each bottle contains 24 capsules.
Ingredients
The active ingredient in DISTAPH is dicloxacillin (as dicloxacillin sodium)
- each DISTAPH 250 capsule contains 250 mg of dicloxacillin
- each DISTAPH 500 capsule contains 500 mg of dicloxacillin
The capsules also contain:
- colloidal anhydrous silica
- magnesium stearate
- gelatin
- titanium dioxide
- purified water
- TekPrint SW-9008 Black Ink (ARTG PI No: 2328)
DISTAPH 250 tablets contains sulfites and 21.2 mg of sodium per dose.
DISTAPH 500 tablets contains sulfites and 42.5 mg of sodium per dose.
Supplier
DISTAPH is supplied by:
Alphapharm Pty Ltd trading as Viatris
Level 1, 30 The Bond30 - 34 Hickson Road
Millers Point NSW 2000
www.viatris.com.au
Phone: 1800 274 276
This leaflet was prepared in November 2022.
Australian registration numbers:
DISTAPH 250: AUST R 226506
DISTAPH 500: AUST R 226508
DISTAPH® is a Viatris company trade mark
DISTAPH_cmi\Nov22/00
Published by MIMS December 2022


 ^ Available from NCCLS, Lancaster avenue, Villanova, Pennsylvania 19085, USA
^ Available from NCCLS, Lancaster avenue, Villanova, Pennsylvania 19085, USA Molecular Formula: C19H16Cl2N3NaO5S,H2O. Molecular Weight: 510.3.
Molecular Formula: C19H16Cl2N3NaO5S,H2O. Molecular Weight: 510.3.