WHAT IS IN THIS LEAFLET
This leaflet answers some common questions about Exemestane Sandoz.
It does not contain all the available information. It does not take the place of talking to your doctor or pharmacist.
All medicines have risks and benefits. Your doctor has weighed the risks of you taking this medicine against the benefits they expect it will have for you.
If you have any concerns about taking this medicine, ask your doctor or pharmacist.
Keep this leaflet with the medicine. You may need to read it again.
WHAT EXEMESTANE SANDOZ IS USED FOR
This medicine is used:
- to treat breast cancer in women who no longer have their menstrual periods, either naturally due to their age (after menopause) or because they have had their ovaries surgically removed
- to reduce the risk of recurrence or spreading of the breast cancer
- when the cancer has not responded or has returned after treatment with another medicine or medicines.
It contains the active ingredient exemestane.
Exemestane is an aromatase inactivator.
It works by significantly reducing the supply of oestrogen to cancer cells. This stops the growth of those cancer cells which need oestrogen, a natural female sex hormone, to grow.
Ask your doctor if you have any questions about why this medicine has been prescribed for you. Your doctor may have prescribed it for another reason.
This medicine is not addictive.
This medicine is available only with a doctor's prescription.
BEFORE YOU TAKE EXEMESTANE SANDOZ
When you must not take it
Do not take this medicine if you have an allergy to:
- exemestane, the active ingredient, or to any of the other ingredients listed at the end of this leaflet under Product Description.
Some of the symptoms of an allergic reaction may include:
- shortness of breath
- wheezing or difficulty breathing
- swelling of the face, lips, tongue or other parts of the body
- rash, itching or hives on the skin.
Do not take this medicine if you are pregnant or intend to become pregnant. It may affect your developing baby if you take it during pregnancy.
Do not breastfeed if you are taking this medicine. The active ingredient in Exemestane Sandoz passes into breast milk and there is a possibility that your baby may be affected.
Exemestane Sandoz is not recommended for use in children.
Do not take this medicine after the expiry date printed on the pack or if the packaging is torn or shows signs of tampering. If it has expired or is damaged, return it to your pharmacist for disposal.
If you are not sure whether you should start taking this medicine, talk to your doctor.
Before you start to take it
Tell your doctor if you have allergies to any other medicines, foods, preservatives or dyes.
Tell your doctor if you:
- are still having your monthly period
- have or have had kidney problems
- have or have had liver problems
- have osteoporosis (disease which causes bones to be more brittle and likely to break).
- have a vitamin D deficiency
If you have not told your doctor about any of the above, tell him/her before you start taking Exemestane Sandoz.
Taking other medicines
Tell your doctor or pharmacist if you are taking any other medicines, including any that you get without a prescription from your pharmacy, supermarket or health food shop.
Some medicines and Exemestane Sandoz may interfere with each other. These include:
- medicines which contain oestrogen, such as hormone replacement therapy (HRT)
- oral contraceptives.
Some health food products for menopausal symptoms contain natural oestrogens.
Tell your doctor or pharmacist if you are taking any medicines or health food products containing oestrogens.
These medicines may be affected by Exemestane Sandoz or may affect how well it works. You may need different amounts of your medicines, or you may need to take different medicines.
Your doctor and pharmacist have more information on medicines to be careful with or avoid while taking this medicine.
HOW TO TAKE EXEMESTANE SANDOZ
Follow all directions given to you by your doctor or pharmacist carefully. They may differ from the information contained in this leaflet.
If you do not understand the instructions, ask your doctor or pharmacist for help.
How much to take
The recommended dose is one 25 mg tablet taken once daily.
Ask your doctor or pharmacist if you are unsure of the correct dose for you. They will tell you exactly how much to take.
Follow the instructions they give you. If you take the wrong dose, Exemestane Sandoz may not work as well and your problem may not improve.
When to take Exemestane Sandoz
Take the tablet once daily after a meal at about the same time each day. Taking it at the same time each day will have the best effect. It will also help you remember when to take it.
How long to take Exemestane Sandoz
Your doctor or pharmacist will tell you how long to take Exemestane Sandoz.
Do not stop taking this medicine unless your doctor tells you to, even if you feel better.
If you forget to take it
Take your dose as soon as you remember, and continue to take it as you would normally.
If it is almost time for your next dose, skip the dose you missed and take your next dose when you are meant to.
Do not take a double dose to make up for the dose that you missed. This may increase the chance of you getting an unwanted side effect.
If you are not sure what to do, ask your doctor or pharmacist.
If you have trouble remembering to take your medicine, ask your pharmacist for some hints.
If you take too much (overdose)
Immediately telephone your doctor or the Poisons Information Centre (telephone Australia 13 11 26) for advice, or go to Accident and Emergency at the nearest hospital, if you think that you or anyone else may have taken too much Exemestane Sandoz. Do this even if there are no signs of discomfort or poisoning. You may need urgent medical attention.
Keep the telephone numbers for these places handy.
WHILE YOU ARE TAKING EXEMESTANE SANDOZ
Things you must do
If you are about to be started on any new medicine, remind your doctor, dentist and pharmacist that you are taking Exemestane Sandoz.
Tell any other doctors, dentists, and pharmacists who treat you that you are taking this medicine.
If you feel that your medicine is not helping your condition, talk to your doctor.
If you go into hospital whilst taking this medicine, let the medical staff know that you are taking Exemestane Sandoz.
If you become pregnant while taking this medicine, tell your doctor immediately.
Keep all of your doctor's appointments so that your progress can be checked.
Things you must not do
Do not take Exemestane Sandoz to treat any other complaints unless your doctor tells you to.
Do not give your medicine to anyone else, even if they have the same condition as you.
Do not stop taking your medicine or lower the dosage without checking with your doctor.
Things to be careful of
Be careful driving or operating machinery until you know how Exemestane Sandoz affects you. This medicine may cause dizziness or tiredness in some people. If you have any of these symptoms, do not drive, operate machinery or do anything else that could be dangerous.
If this medicine makes you feel dizzy, be careful when getting up from a sitting or lying position.
SIDE EFFECTS
Tell your doctor or pharmacist as soon as possible if you do not feel well while you are taking Exemestane Sandoz.
All medicines can have side effects. Sometimes they are serious, most of the time they are not. You may need medical attention if you get some of the side effects.
Do not be alarmed by the following lists of side effects. You may not experience any of them.
Ask your doctor or pharmacist to answer any questions you may have.
Tell your doctor or pharmacist as soon as possible if you notice any of the following side effects or other effects that you think may be related to your treatment:
- hot flushes
- nausea, vomiting, loss of appetite, indigestion, pain (including stomach ache)
- constipation
- diarrhoea
- tiredness
- swelling in your legs
- dizziness and headache
- increased sweating
- difficulty sleeping
- depression
- disturbed vision such as blurriness
- pain in your muscle or joints
- increase in weight
- skin rash or itching
- hair loss
- bleeding or bruising more easily than normal
- pain and/or numbness of hands, loss of feeling in fingers/thumb
- frequent infections such as fever, severe chills, sore throat or mouth ulcers
- symptoms of gastric ulcer such as blood in stools, black tarry stools or vomiting of blood
- abnormal vaginal bleeding
- hepatitis, yellowing of the skin or eyes, also called jaundice.
Tell your doctor or pharmacist if you notice anything else that is making you feel unwell. Other side effects not listed above may also occur in some people. Some of these side effects can only be found when your doctor does tests from time to time to check your progress.
AFTER TAKING EXEMESTANE SANDOZ
Storage
Keep your medicine in the original container.
If you take it out of its original container it may not keep well.
Keep your medicine in a cool dry place where the temperature stays below 25°C.
Do not store Exemestane Sandoz or any other medicine in the bathroom or near a sink. Do not leave it on a window sill or in the car.
Heat and dampness can destroy some medicines.
Keep it where children cannot reach it. A locked cupboard at least one-and-a-half metres above the ground is a good place to store medicines.
Disposal
If your doctor tells you to stop taking this medicine or the expiry date has passed, ask your pharmacist what to do with any medicine that is left over.
PRODUCT DESCRIPTION
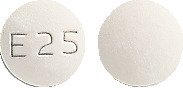
What it looks like
Exemestane Sandoz comes in one strength:
Exemestane Sandoz 25mg - white to off-white, round biconvex film-coated tablets, marked with 'E25' on one side and plain on the other.
Available in blisters of 30 film-coated tablets.
Ingredients
Active ingredient:
- Exemestane Sandoz 25mg - 25mg exemestane.
Inactive ingredients:
- mannitol
- microcrystalline cellulose
- crospovidone
- sodium starch glycollate (type A)
- hypromellose
- polysorbate 80
- colloidal anhydrous silica
- magnesium stearate
- macrogol 400
- titanium dioxide.
This medicine does not contain lactose, sucrose, gluten, tartrazine or any other azo dyes.
Supplier
Sandoz Pty Ltd
ABN 60 075 449 553
54 Waterloo Road
Macquarie Park, NSW 2113
Australia
Tel: 1800 726 369
This leaflet was revised in February 2022.
Australian Register Number
25mg film-coated tablets: AUST R 174337 (blisters)
Published by MIMS April 2022

 The incidence of myocardial infarction (0.6% vs 0.2%, p = 0.030) and cardiac failure (1.1% versus 0.7%, p = 0.123) in patients treated with exemestane compared with those treated with tamoxifen was not significant at the nominal significance level of 0.01 used to allow for multiple testing.
The incidence of myocardial infarction (0.6% vs 0.2%, p = 0.030) and cardiac failure (1.1% versus 0.7%, p = 0.123) in patients treated with exemestane compared with those treated with tamoxifen was not significant at the nominal significance level of 0.01 used to allow for multiple testing.

 Efficacy was also observed in patients having progressed following multiple hormone therapies (third line therapy). Three peer reviewed uncontrolled phase II studies were conducted at the recommended dose of 25 mg exemestane. In the combined analysis, which was of the descriptive type, exemestane induced objective response, with a median duration of 61 weeks, in 9% of the patients (95% C.I. 6-12) and overall clinical benefit, with a median duration of 37 weeks, in 26% of the cases (95% C.I. 22-31). Although survival cannot yet be estimated in each of the three studies, median survival in the overall population (intent to treat) was approximately 30 months (131.1 weeks, 95% C.I. 100.0-147.1 weeks). Exemestane was effective both in patients experiencing failure of megestrol acetate and failure of other nonsteroidal aromatase inhibitors.
Efficacy was also observed in patients having progressed following multiple hormone therapies (third line therapy). Three peer reviewed uncontrolled phase II studies were conducted at the recommended dose of 25 mg exemestane. In the combined analysis, which was of the descriptive type, exemestane induced objective response, with a median duration of 61 weeks, in 9% of the patients (95% C.I. 6-12) and overall clinical benefit, with a median duration of 37 weeks, in 26% of the cases (95% C.I. 22-31). Although survival cannot yet be estimated in each of the three studies, median survival in the overall population (intent to treat) was approximately 30 months (131.1 weeks, 95% C.I. 100.0-147.1 weeks). Exemestane was effective both in patients experiencing failure of megestrol acetate and failure of other nonsteroidal aromatase inhibitors.
