SUMMARY CMI
ARX-IMATINIB
Consumer Medicine Information (CMI) summary
The full CMI on the next page has more details. If you are worried about using this medicine, speak to your doctor or pharmacist.
1. Why am I using ARX-IMATINIB?
ARX-IMATINIB contains the active ingredient imatinib. ARX-IMATINIB is used to treat leukaemia and some other forms of cancer.
For more information, see Section 1. Why am I using ARX-IMATINIB? in the full CMI.
2. What should I know before I use ARX-IMATINIB?
Do not use if you have ever had an allergic reaction to imatinib or any of the ingredients listed at the end of the CMI.
Talk to your doctor if you have any other medical conditions, take any other medicines, or are pregnant or plan to become pregnant or are breastfeeding.
For more information, see Section 2. What should I know before I use ARX-IMATINIB? in the full CMI.
3. What if I am taking other medicines?
Some medicines may interfere with ARX-IMATINIB and affect how it works.
A list of these medicines is in Section 3. What if I am taking other medicines? in the full CMI.
4. How do I use ARX-IMATINIB?
- Your doctor will advise on the appropriate dose for your condition.
- ARX-IMATINIB is usually taken as a single dose each day, although twice daily dosing may be recommended by your doctor.
- Take ARX-IMATINIB with food and a large glass of water
- Capsules should be taken whole. If you have trouble swallowing, capsules may be opened and poured into a glass of water or apple juice and swallowed.
More instructions can be found in Section 4. How do I use ARX-IMATINIB? in the full CMI.
5. What should I know while using ARX-IMATINIB?
| Things you should do |
|
| Things you should not do |
|
| Driving or using machines |
|
| Drinking alcohol |
|
| Looking after your medicine |
|
For more information, see Section 5. What should I know while using ARX-IMATINIB? in the full CMI.
6. Are there any side effects?
Tell your doctor if you notice anything that is making you unwell while you are taking ARX-IMATINIB.
For more information, including what to do if you have any side effects, see Section 6. Are there any side effects? in the full CMI.
FULL CMI
ARX-IMATINIB
Active ingredient(s): imatinib
Consumer Medicine Information (CMI)
This leaflet provides important information about using ARX-IMATINIB. You should also speak to your doctor or pharmacist if you would like further information or if you have any concerns or questions about using ARX-IMATINIB.
Where to find information in this leaflet:
1. Why am I using ARX-IMATINIB?
2. What should I know before I use ARX-IMATINIB?
3. What if I am taking other medicines?
4. How do I use ARX-IMATINIB?
5. What should I know while using ARX-IMATINIB?
6. Are there any side effects?
7. Product details
1. Why am I using ARX-IMATINIB?
ARX-IMATINIB contains the active ingredient imatinib. ARX-IMATINIB is a protein‐tyrosine kinase inhibitor used to treat leukaemia and a number of other forms of cancer by slowing the growth of abnormal cells while leaving normal cells alone.
ARX-IMATINIB is used to treat adults and children/adolescents who have chronic myeloid leukaemia (CML) and acute lymphoblastic leukaemia with Philadelphia chromosome positive (Ph‐positive ALL).
CML and ALL are types of leukaemia in which an abnormal chromosome produces an enzyme that leads to uncontrolled growth of white blood cells.
ARX-IMATINIB is also used to treat adults for:
- myelodysplastic/myeloproliferative diseases (MDS/MPD).
These are a group of blood diseases in which some blood cells start growing out of control. - Aggressive systemic mastocytosis (ASM).
It is a cancer in which certain blood cells, called "mast" cells, grow out of control. - Hypereosinophilic syndrome (HES) or chronic eosinophilic leukaemia (CEL).
These are blood diseases in which some blood cells, named "eosinophils", start growing out of control. - gastro‐intestinal stromal tumours (GIST).
This is a type of cancer of the stomach and bowels. This cancer affects the tissue that surrounds the stomach and bowels and the cells grow uncontrollably. - dermatofibrosarcoma protuberans (DFSP).
DFSP is a cancer of the tissue beneath the skin in which some cells start growing out of control.
Your doctor may have prescribed it for another purpose.
There is not enough information to recommend the use of ARX-IMATINIB in children under 3 years of age for most uses. For use in CML, there is no experience with the use of ARX-IMATINIB in children below 2 years of age. For acute lymphoblastic leukaemia with Philadelphia chromosome positive (Ph‐positive ALL), there is no experience with the use of ARX-IMATINIB in children below 1 year of age.
Talk to your doctor or pharmacist if you have any questions about ARX-IMATINIB.
2. What should I know before I use ARX-IMATINIB?
Warnings
Do not use ARX-IMATINIB if:
- you are allergic to imatinib, or any of the ingredients listed at the end of this leaflet. Always check the ingredients to make sure you can use this medicine.
Some of the symptoms of an allergic reaction may include shortness of breath, wheezing or difficulty breathing; swelling of the face, lips, tongue or other parts of the body; rash, itching or hives on the skin. - Do not take ARX-IMATINIB after the expiry date printed on the pack or if the packaging is torn or shows signs of tampering. In that case, return the medicine to your pharmacist.
Check with your doctor if you:
- have ever had any other medical conditions or procedures:
- kidney or liver problems
- problems with your heart
- you have had your thyroid gland removed
- hepatitis B infection. As during treatment with ARX-IMATINIB, hepatitis B (an infection of the liver) may become active again. - take any medicines for any other condition
Your doctor may want to take special precautions in these cases.
During treatment, you may be at risk of developing certain side effects. It is important you understand these risks and how to monitor for them. See additional information under Section 6. Are there any side effects?
ARX-IMATINIB is not addictive.
Pregnancy and breastfeeding
Tell your doctor if you are pregnant or intend to become pregnant. This medicine may be harmful to your unborn baby. If it is necessary for you to take it during pregnancy, your doctor will discuss with you the risks and benefits involved.
Tell your doctor if you are breastfeeding or intend to breastfeed. It is not known if the active ingredient, imatinib, passes into the breast milk. Because this medicine could affect your baby, breast‐feeding is not recommended.
3. What if I am taking other medicines?
Tell your doctor or pharmacist if you are taking any other medicines, including any medicines, vitamins or supplements that you buy without a prescription from your pharmacy, supermarket or health food shop.
Some medicines and ARX-IMATINIB may interfere with each other. These include many medicines that are eliminated from the body through the liver:
- St. John's wort, a herbal medicine found in many products that you can buy without a prescription
- paracetamol, a medicine found in many common pain relievers and cold remedies (e.g. Panadol®, Panadeine®, Codral®, Tylenol®) which are known to be associated with liver toxicity. A patient, who was taking paracetamol regularly for fever, died of acute liver failure. Although the cause is currently unknown, special caution should be exercised when using paracetamol and ARX-IMATINIB.
- antibiotic medicines such as rifampicin, ketoconazole, erythromycin, clarithromycin, itraconazole
- antiviral medicines used to treat HIV/AIDS
- dexamethasone, a steroid medicine
- medicines for high cholesterol, such as simvastatin
- medicines used to treat epilepsy, such as phenytoin, carbamazepine, phenobarbitone
- warfarin, a medicine used to prevent blood clots
- some medicines used to treat mental disorders and depression
- some medicines used to treat high blood pressure and heart problems
- cyclosporin
You may need to take different amounts of these medicines or you may need to take different medicines. Your doctor and pharmacist have more information.
If you have not told your doctor about any of these things, tell him/her before you start taking this medicine.
Check with your doctor or pharmacist if you are not sure about what medicines, vitamins or supplements you are taking and if these affect ARX-IMATINIB.
4. How do I use ARX-IMATINIB?
Follow the instructions provided and use ARX-IMATINIB until your doctor tells you to stop. These instructions may differ from the information contained in this leaflet.
If you do not understand the instructions on the label, ask your doctor or pharmacist for help.
How much to take/use
For CML, the usual dose for an adult is 400 to 600 mg each day and the maximum dose is 800 mg each day. The dose depends on what stage of CML you have. For Ph‐positive ALL the usual dose is 600 mg each day.
For children treated with CML and Ph‐positive ALL, the dose depends on the size of the child.
For MDS/MPD, the starting dose is 400 mg.
For ASM and HES/CEL, the usual starting dose is 400 mg. For some patients the starting dose may be 100 mg.
For GIST, the usual dose is 400 mg or 600 mg each day.
For DFSP, the starting dose is 800 mg per day.
Daily dose of 400 mg should be taken as one tablet of 400 mg once a day.
Daily dose of 600 mg should be taken as either:
- six capsules of 100 mg or
- one capsule of 400 mg plus two 100 mg capsules once a day.
A daily dose of 800 mg should be taken as 400 mg twice a day, in the morning and in the evening.
Your doctor may direct you to take a higher or lower dose, or stop treatment if needed depending on your response to ARX-IMATINIB.
When to take/use ARX-IMATINIB
ARX-IMATINIB is usually taken as a single dose each day. However, your doctor may want you to take them in two doses, one in the morning and one in the evening.
Continue taking ARX-IMATINIB every day for as long as your doctor prescribes. Your doctor will keep a close check on you to make sure you are still benefiting from treatment.
How to take ARX-IMATINIB
Take the medicine with a large glass of water and food. This will help to avoid irritating the lining of your oesophagus (food pipe) and stomach.
Swallow the capsules whole with a large glass of water. Do not open or crush the capsules unless you have difficulty in swallowing (e.g. in children).
- If you are unable to swallow the capsules, you can open them up and pour the powder into a glass of still water or apple juice.
- If you are a woman who is pregnant or might get pregnant and are trying to open the capsules, you should handle the contents with caution in order to avoid skin‐eye contact or inhalation.
You should wash your hands immediately after opening the capsules.
For the best effect, take the medicine at about the same time each day. Taking them at the same time each day will help you to remember to take them.
If you forget to use ARX-IMATINIB
ARX-IMATINIB should be used regularly at the same time each day. If you miss your dose at the usual time, take the missed dose as soon as you remember, then continue with your normal schedule.
Do not take a double dose to make up for the one that you missed. This may increase the chance of you getting an unwanted side effect.
If you are not sure what to do, ask your doctor or pharmacist.
If you have trouble remembering when to take your medicine, ask your pharmacist for some hints.
If you use too much ARX-IMATINIB
If you think that you have used too much ARX-IMATINIB, you may need urgent medical attention.
You should immediately:
- phone the Poisons Information Centre (by calling 13 11 26), or
- contact your doctor, or
- go to the Emergency Department at your nearest hospital.
You should do this even if there are no signs of discomfort or poisoning.
Keep the phone numbers for these places handy.
5. What should I know while using ARX-IMATINIB?
Things you must do
Make sure you follow your doctor's instructions carefully and keep all appointments. You will need regular follow‐up to make sure the treatment is working. Regular blood tests, weight checks and urine tests can also find side effects before they become serious.
Some children and adolescents taking ARX-IMATINIB may have slower than normal growth. Growth will be monitored at regular visits by your doctor.
Make sure you use a method of contraception to prevent pregnancy during treatment with ARX-IMATINIB and for 15 days after ending treatment.
If you are about to be started on any new medicine, remind your doctor and pharmacist that you are taking ARX-IMATINIB.
Call your doctor straight away if you:
- if you become pregnant while you are taking this medicine.
Remind any doctor, dentist or pharmacist you visit that you are using ARX-IMATINIB.
Things you should not do
Avoid drinking grapefruit juice while you are being treated with ARX-IMATINIB. Grapefruit juice may interact with ARX-IMATINIB and affect how your body uses this medicine.
Do not give this medicine to anyone else even if their condition seems to be the same as yours.
Do not use it to treat any other complaints unless your doctor tells you to.
Things to be careful of
If you need to take something to treat a headache, cold or other minor aches and pains, try to avoid taking medicines containing paracetamol (e.g. Panadol®, Panadeine®, Codral®, Tylenol®). Ask your pharmacist to suggest an alternative medicine.
When you are outdoors, wear protective clothing and use at least a 15+ sunscreen. Do not use sunlamps or tanning beds. This medicine may cause your skin to be much more sensitive to sunlight than it normally is. Exposure to sunlight may cause a skin rash, itching, redness or severe sunburn. If your skin does appear to be burning, tell your doctor.
Driving or using machines
This medicine may cause dizziness, light‐headedness or drowsiness in some people. Make sure you know how you react to it before you drive a car, operate machinery or do anything that could be dangerous.
Drinking alcohol
Tell your doctor if you drink alcohol.
Looking after your medicine
Keep your medicine in its original packaging until it is time to take it. The medicine will not keep as well if taken out of the packaging.
Keep this medicine in a cool dry place where the temperature stays below 25°C.
Store it in a cool dry place away from moisture, heat or sunlight; for example, do not store it:
- in the bathroom or near a sink, or
- in the car or on windowsills.
Keep it where young children cannot reach it.
Getting rid of any unwanted medicine
If your doctor tells you to stop taking this medicine or it is out of date, take it to any pharmacy for safe disposal.
Do not use this medicine after the expiry date.
6. Are there any side effects?
Tell your doctor, nurse or pharmacist as soon as possible if you do not feel well while you are being treated with this medicine.
All medicines have some unwanted side effects. Sometimes they are serious, but most of the time they are not. You may need medical treatment if you get some of the side effects
Do not be alarmed by these lists of possible side effects. You may not experience any of them. Ask your doctor or pharmacist to answer any questions you may have.
Less serious side effects
| Less serious side effects | What to do |
| Speak to your doctor if you have any of these less serious side effects and they worry you. |
Serious side effects
| Serious side effects | What to do |
| Call your doctor straight away, or go straight to the Emergency Department at your nearest hospital if you notice any of these serious side effects. |
Tell your doctor or pharmacist if you notice anything else that may be making you feel unwell.
Other side effects not listed here may occur in some people. Other side effects not listed here or not yet known may happen in some people. Some of these side effects can only be found by laboratory testing.
Reporting side effects
After you have received medical advice for any side effects you experience, you can report side effects to the Therapeutic Goods Administration online at www.tga.gov.au/reporting-problems. By reporting side effects, you can help provide more information on the safety of this medicine.
Always make sure you speak to your doctor or pharmacist before you decide to stop taking any of your medicines.
7. Product details
This medicine is only available with a doctor's prescription.
What ARX-IMATINIB contains
| Active ingredient (main ingredient) | Imatinib mesilate |
| Other ingredients (inactive ingredients) |
|
Do not take this medicine if you are allergic to any of these ingredients.
This medicine is gluten‐free, lactose‐free, sucrose‐free, tartrazine‐free and free of other azo dyes.
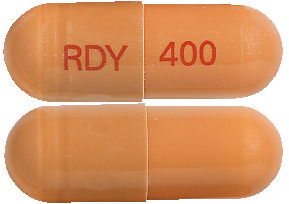
What ARX-IMATINIB looks like
ARX-IMATINIB 50 mg capsules (AUST R 261059) are off‐white to brownish yellow colour granular powder filled in light yellow to orange yellow opaque Size ‘4’ Hard Gelatin capsule imprinted with ‘RDY’ on cap and ‘50’ on body with red ink. Available in blister packs of 30 capsules.
ARX-IMATINIB 100 mg capsule (AUST R 261054) is an off‐white to brownish yellow colour granular powder filled in an orange to greyish‐orange opaque size ‘1’ hard gelatin capsule imprinted with ‘RDY’ on cap and ‘100’ on body with red ink. Available in blister packs of 60 capsules.
ARX-IMATINIB 400 mg capsule (AUST R 261060) is an off‐white to brownish yellow colour granular powder filled in a very dark yellow to brownish‐orange opaque size ‘00’ hard gelatin capsule imprinted with ‘RDY’ on cap and ‘400’ on body with red ink. Available in blister packs of 30 capsules.
Who is the Sponsor of ARX-IMATINIB
Dr. Reddy's Laboratories (Australia) Pty Ltd
Level 3, 390 St Kilda Road
Melbourne, VIC 3004
Australia
Who Distributes ARX-IMATINIB
Arrotex Pharmaceuticals Pty Ltd
Cremorne VIC 3121
This leaflet was prepared in March 2023
Published by MIMS January 2024







 The adjuvant trial SSG XVIII/AIO compared 1 year and 3 years imatinib treatment. Table 7 shows adverse events, regardless of relationship to study drug, that were reported in at least 5% of patients treated with imatinib.
The adjuvant trial SSG XVIII/AIO compared 1 year and 3 years imatinib treatment. Table 7 shows adverse events, regardless of relationship to study drug, that were reported in at least 5% of patients treated with imatinib. Adverse events with imatinib observed in trials in Ph+ ALL, MDS/MPD, SM, HES/CEL and DFSP were generally consistent with those seen in CML and GIST studies.
Adverse events with imatinib observed in trials in Ph+ ALL, MDS/MPD, SM, HES/CEL and DFSP were generally consistent with those seen in CML and GIST studies.


 Laboratory abnormalities with imatinib observed in trials in Ph+ ALL, MDS/MPD, SM, HES/CEL and DFSP were generally consistent with those seen in CML and GIST studies.
Laboratory abnormalities with imatinib observed in trials in Ph+ ALL, MDS/MPD, SM, HES/CEL and DFSP were generally consistent with those seen in CML and GIST studies. Rates of complete haematological response, major cytogenetic response and complete cytogenetic response on first-line treatment were estimated using the Kaplan-Meier approach, for which non-responses were censored at the date of last examination. Using this approach the estimated cumulative response rates for first-line treatment with imatinib are shown in Table 13.
Rates of complete haematological response, major cytogenetic response and complete cytogenetic response on first-line treatment were estimated using the Kaplan-Meier approach, for which non-responses were censored at the date of last examination. Using this approach the estimated cumulative response rates for first-line treatment with imatinib are shown in Table 13. For analysis of long-term outcomes patients randomised to receive imatinib were compared with patients randomised to receive IFN. Patients who crossed over prior to progression were not censored at the time of crossover, and events that occurred in these patients following crossover were attributed to the original randomised treatment.
For analysis of long-term outcomes patients randomised to receive imatinib were compared with patients randomised to receive IFN. Patients who crossed over prior to progression were not censored at the time of crossover, and events that occurred in these patients following crossover were attributed to the original randomised treatment.
 A total of 71 (12.8%) and 85 (15.4%) patients died in the imatinib and IFN+Ara-C groups, respectively. At 84 months the estimated overall survival is 86.4% (83, 90) vs. 83.3% (80, 87) in the randomised imatinib and the IFN+Ara-C groups, respectively (p=0.073, log-rank test). This time-to-event endpoint is strongly affected by the high crossover rate from IFN+Ara-C to imatinib. Additionally, a greater number of patients received bone marrow transplant (BMT) after discontinuation of study treatment in the IFN+Ara-C group (n=66, 38 after crossover to imatinib) compared with the imatinib group (n=50, 8 after crossover to IFN) at the 84 month update. When censoring the 48 deaths that occurred after BMT, the 84-months survival rates were 89.6 vs 88.1 (p=0.200, log-rank test). Only 31 deaths (before BMT) of the imatinib patients (5.6%) were attributed to CML, compared to 40 of the IFN+Ara-C patients (7.2%).
A total of 71 (12.8%) and 85 (15.4%) patients died in the imatinib and IFN+Ara-C groups, respectively. At 84 months the estimated overall survival is 86.4% (83, 90) vs. 83.3% (80, 87) in the randomised imatinib and the IFN+Ara-C groups, respectively (p=0.073, log-rank test). This time-to-event endpoint is strongly affected by the high crossover rate from IFN+Ara-C to imatinib. Additionally, a greater number of patients received bone marrow transplant (BMT) after discontinuation of study treatment in the IFN+Ara-C group (n=66, 38 after crossover to imatinib) compared with the imatinib group (n=50, 8 after crossover to IFN) at the 84 month update. When censoring the 48 deaths that occurred after BMT, the 84-months survival rates were 89.6 vs 88.1 (p=0.200, log-rank test). Only 31 deaths (before BMT) of the imatinib patients (5.6%) were attributed to CML, compared to 40 of the IFN+Ara-C patients (7.2%).
 Efficacy results were similar in men and women and in patients younger and older than age 65. Responses were seen in black patients, but there were too few black patients to allow a quantitative comparison.
Efficacy results were similar in men and women and in patients younger and older than age 65. Responses were seen in black patients, but there were too few black patients to allow a quantitative comparison. In study AJP01 imatinib (600 mg/day on days 8 - 63 of induction chemotherapy, and on days 1 - 28 of each chemotherapy cycle during consolidation and maintenance) was integrated into a chemotherapy regimen in 80 patients with de novo Ph+ ALL. Results are summarized in Table 17.
In study AJP01 imatinib (600 mg/day on days 8 - 63 of induction chemotherapy, and on days 1 - 28 of each chemotherapy cycle during consolidation and maintenance) was integrated into a chemotherapy regimen in 80 patients with de novo Ph+ ALL. Results are summarized in Table 17. Analysis of event-free survival and overall survival also indicated superiority of the imatinib-containing regimen (p < 0.0001 for both).
Analysis of event-free survival and overall survival also indicated superiority of the imatinib-containing regimen (p < 0.0001 for both).

 Imatinib has not been shown to be effective in patients with less aggressive forms of systemic mastocytosis. Imatinib is not recommended for use in patients with cutaneous mastocytosis, indolent systemic mastocytosis (smoldering SM or isolated bone marrow mastocytosis), SM with an associated clonal haematological non-mast cell lineage disease, mast cell leukaemia, mast cell sarcoma or extracutaneous mastocytoma. In vitro, cell lines and patient-derived mast cells harbouring the KIT D816V mutation were resistant to imatinib and the effectiveness of imatinib in the treatment of patients with SM who have the D816V mutation remains controversial.
Imatinib has not been shown to be effective in patients with less aggressive forms of systemic mastocytosis. Imatinib is not recommended for use in patients with cutaneous mastocytosis, indolent systemic mastocytosis (smoldering SM or isolated bone marrow mastocytosis), SM with an associated clonal haematological non-mast cell lineage disease, mast cell leukaemia, mast cell sarcoma or extracutaneous mastocytoma. In vitro, cell lines and patient-derived mast cells harbouring the KIT D816V mutation were resistant to imatinib and the effectiveness of imatinib in the treatment of patients with SM who have the D816V mutation remains controversial. Additionally, improvements in symptomatology and other organ dysfunction abnormalities were reported by the investigators in the case reports. Improvements were reported in cardiac, nervous, skin/subcutaneous tissue, respiratory/thoracic/mediastinal, musculoskeletal/connective tissue/vascular, and gastrointestinal organ systems.
Additionally, improvements in symptomatology and other organ dysfunction abnormalities were reported by the investigators in the case reports. Improvements were reported in cardiac, nervous, skin/subcutaneous tissue, respiratory/thoracic/mediastinal, musculoskeletal/connective tissue/vascular, and gastrointestinal organ systems. Median follow up for the combined studies was 37.5 months (25th - 75th percentile 19 to 46 months). There was a statistically significant improvement in PFS in the 800 mg treatment group (23.2 months [95% CI, 20.8 to 24.9]) compared to the 400 mg treatment group (18.9 months [95% CI, 17.4 to 21.2]) (p=0.03). However, there were no observed differences in overall survival between the treatment groups (p=0.98). The estimated overall PFS for all 1640 patients in these Phase III studies was 21 months [95% CI 19.4 to 22.5] and the estimated OS of 48.8 months [95% CI 46.3 to 51.6]. 5.1% of patients achieved a confirmed complete response and 47.5% achieved a partial response. Treatment at either dose level was generally well tolerated and overall 5.4% of patients withdrew due to toxicity.
Median follow up for the combined studies was 37.5 months (25th - 75th percentile 19 to 46 months). There was a statistically significant improvement in PFS in the 800 mg treatment group (23.2 months [95% CI, 20.8 to 24.9]) compared to the 400 mg treatment group (18.9 months [95% CI, 17.4 to 21.2]) (p=0.03). However, there were no observed differences in overall survival between the treatment groups (p=0.98). The estimated overall PFS for all 1640 patients in these Phase III studies was 21 months [95% CI 19.4 to 22.5] and the estimated OS of 48.8 months [95% CI 46.3 to 51.6]. 5.1% of patients achieved a confirmed complete response and 47.5% achieved a partial response. Treatment at either dose level was generally well tolerated and overall 5.4% of patients withdrew due to toxicity. A statistically significant difference in response rates between the two dose groups was not demonstrated. A significant number of patients who had stable disease at the time of the interim analysis achieved a partial response with longer treatment (median follow-up 31 months). Median time to response was 13 weeks (95% C.I. 12 to 23). Median time to treatment failure in responders was 122 weeks (95% C.I. 106 to 147), while in the overall study population it was 84 weeks (95% C.I. 71 to 109). The median overall survival has not been reached. The Kaplan-Meier estimate for survival after 36-month follow-up is 68% [Figure 3]. Additionally, there is no difference in survival between patients achieving stable disease and partial response [Figure 4].
A statistically significant difference in response rates between the two dose groups was not demonstrated. A significant number of patients who had stable disease at the time of the interim analysis achieved a partial response with longer treatment (median follow-up 31 months). Median time to response was 13 weeks (95% C.I. 12 to 23). Median time to treatment failure in responders was 122 weeks (95% C.I. 106 to 147), while in the overall study population it was 84 weeks (95% C.I. 71 to 109). The median overall survival has not been reached. The Kaplan-Meier estimate for survival after 36-month follow-up is 68% [Figure 3]. Additionally, there is no difference in survival between patients achieving stable disease and partial response [Figure 4].




 Twelve of these 18 patients either achieved a complete response (7 patients) or were made disease free by surgery after a partial response (5 patients, including one child) for a total complete response rate of 67%. A further 3 patients achieved a partial response, for an overall response rate of 83%. Of the 8 patients with metastatic disease, five responded (62%) three of them completely (37%). The median duration of therapy in study B2225 was 6.2 months, with a maximum duration of 24.3 months, while in the published literature it ranged between 4 weeks and more than 20 months.
Twelve of these 18 patients either achieved a complete response (7 patients) or were made disease free by surgery after a partial response (5 patients, including one child) for a total complete response rate of 67%. A further 3 patients achieved a partial response, for an overall response rate of 83%. Of the 8 patients with metastatic disease, five responded (62%) three of them completely (37%). The median duration of therapy in study B2225 was 6.2 months, with a maximum duration of 24.3 months, while in the published literature it ranged between 4 weeks and more than 20 months. Imatinib and its metabolites are not excreted via the kidney to a significant extent. In a study of patients with varying degrees of renal dysfunction (mild, moderate and severe - see Table 27 for renal function classification), the mean exposure to imatinib (dose normalized AUC) increased 1.5- to 2-fold compared to patients with normal renal function, which corresponded to an elevated plasma level of AGP, a protein to which imatinib binds strongly. No correlation between imatinib exposure and the severity of renal deficiency was observed. In this study, 800 mg daily was safely used in patients with mild renal dysfunction and 600 mg daily was used in moderate renal dysfunction. The 800 mg dose was not tested in patients with moderate renal dysfunction due to the limited number of patients enrolled. Similarly, only 2 patients with severe renal dysfunction were enrolled at the low (100 mg) dose, and no higher doses were tested. No patients on haemodialysis were enrolled in the study. Literature data showed that a daily dose of 400 mg was well tolerated in a patient with end-stage renal disease on haemodialysis. The PK plasma exposure in this patient fell within the range of values of imatinib and its metabolite CGP74588 observed in patients with normal renal function. Dialysis was not found to intervene with the plasma kinetics of imatinib. Since renal excretion represents a minor elimination pathway for imatinib, patients with severe renal insufficiency and on dialysis could receive treatment at the 400 mg starting dose. However, in these patients caution is recommended. The dose can be reduced if not tolerated, or increased for lack of efficacy (see Section 4.4 Special Warnings and Precautions for Use; Section 4.2 Dose and Method of Administration).
Imatinib and its metabolites are not excreted via the kidney to a significant extent. In a study of patients with varying degrees of renal dysfunction (mild, moderate and severe - see Table 27 for renal function classification), the mean exposure to imatinib (dose normalized AUC) increased 1.5- to 2-fold compared to patients with normal renal function, which corresponded to an elevated plasma level of AGP, a protein to which imatinib binds strongly. No correlation between imatinib exposure and the severity of renal deficiency was observed. In this study, 800 mg daily was safely used in patients with mild renal dysfunction and 600 mg daily was used in moderate renal dysfunction. The 800 mg dose was not tested in patients with moderate renal dysfunction due to the limited number of patients enrolled. Similarly, only 2 patients with severe renal dysfunction were enrolled at the low (100 mg) dose, and no higher doses were tested. No patients on haemodialysis were enrolled in the study. Literature data showed that a daily dose of 400 mg was well tolerated in a patient with end-stage renal disease on haemodialysis. The PK plasma exposure in this patient fell within the range of values of imatinib and its metabolite CGP74588 observed in patients with normal renal function. Dialysis was not found to intervene with the plasma kinetics of imatinib. Since renal excretion represents a minor elimination pathway for imatinib, patients with severe renal insufficiency and on dialysis could receive treatment at the 400 mg starting dose. However, in these patients caution is recommended. The dose can be reduced if not tolerated, or increased for lack of efficacy (see Section 4.4 Special Warnings and Precautions for Use; Section 4.2 Dose and Method of Administration).
 Chemical Formula: 4-[(4-Methyl-1-piperazinyl) methyl]-N-[4-methyl-3-[[4-(3-pyridinyl)-2-pyrimidinyl] amino]-phenyl] benzamide methanesulfonate.
Chemical Formula: 4-[(4-Methyl-1-piperazinyl) methyl]-N-[4-methyl-3-[[4-(3-pyridinyl)-2-pyrimidinyl] amino]-phenyl] benzamide methanesulfonate.