What is in this leaflet
This leaflet answers some common questions about IMURAN Injection. It does not contain all of the available information.
It does not take the place of talking to your doctor or pharmacist.
All medicines have risks and benefits. Your doctor has weighed the risks of giving you IMURAN Injection against the benefits they expect it will have for you.
If you have any concerns about being given this medicine, ask your doctor or pharmacist.
Keep this leaflet with the medicine.
You may need to read it again.
What IMURAN Injection is used for
IMURAN Injection contains azathioprine as the active ingredient. Azathioprine belongs to a group of medicines called immunosuppressants.
IMURAN Injection is used to help prevent the rejection of a transplanted organ such as a kidney, liver or heart. It works by suppressing the body's immune defence system.
IMURAN Injection can also be used to treat other diseases called autoimmune diseases where your immune system is reacting against your own body. These may include:
- severe rheumatoid arthritis
- systemic lupus erythematosus
- chronic active hepatitis
- certain skin, muscle, and blood diseases.
IMURAN Injection is usually given in combination with other medicines such as corticosteroids or other immunosuppressive drugs.
Ask your doctor if you have any questions about why IMURAN Injection has been prescribed for you.
Your doctor may have prescribed it for another purpose.
This medicine is only available with a doctor's prescription.
There is no evidence that it is addictive.
Before you are given it
When you must not be given it
You must not be given IMURAN Injection if you have ever had an allergic reaction to:
- azathioprine
- 6-mercaptopurine (Puri-Nethol), a medicine which is similar to IMURAN Injection
- any of the ingredients listed at the end of this leaflet.
Symptoms of an allergic reaction may include shortness of breath, wheezing or difficulty in breathing; swelling of the face, lips, tongue or any other parts of the body; rash, itching or hives on the skin.
You must not be given IMURAN Injection if you are pregnant, may be pregnant, plan to become pregnant or intending to father a child.
This medicine may cause birth defects if either the male or female is taking it at the time of conception.
You must not be given IMURAN Injection if you are breastfeeding unless you and your doctor have discussed the risks and benefits involved.
It is not recommended for use while breastfeeding as it may cause serious side effects to your baby.
You must not be given IMURAN Injection if you have rheumatoid arthritis that has previously been treated with some other medicines, such as chlorambucil, melphalan or cyclophosphamide.
You must not be given IMURAN Injection after the expiry date printed on the pack.
If you are given this medicine after the expiry date has passed, it may not work as well.
You must not be given IMURAN Injection if the packaging is torn or shows signs of tampering.
If you are not sure whether you should be given this medicine, talk to your doctor.
Before you are given it
Tell your doctor if you are allergic to any other medicines or any foods, dyes or preservative.
Tell your doctor if you have or have had any of the following medical conditions:
- liver or kidney disease
- a condition where your body produces too little of a natural chemical called thiopurine methyltransferase (TPMT)
- Lesch-Nyhan Syndrome
- chickenpox or shingles
- hepatitis B.
Tell your doctor if you have recently been vaccinated or immunised or plan to do so.
IMURAN Injection may affect the way the vaccine works or your reaction to the vaccine.
Tell your doctor if you are pregnant, may be pregnant, plan to become pregnant or intending to father a child.
You or your partner should take adequate contraceptive precautions while you are taking IMURAN Injection.
Tell your doctor if you are breastfeeding or planning to breastfeed.
IMURAN Injection is not recommended for use while breastfeeding as it may cause serious side effects to your baby.
Tell your dentist that you are being given IMURAN Injection.
Dental work, whenever possible, should be completed before you start to be given IMURAN Injection or delayed until your blood cell counts are normal.
Taking other medicines
Tell your doctor if you are taking any other medicines, including any that you get without a prescription from a pharmacy, supermarket or health food shop.
Some medicines may interfere with IMURAN Injection. These include:
- penicillamine, used mainly in the treatment of rheumatoid arthritis
- captopril, used mainly to treat high blood pressure and heart failure
- cimetidine, used to treat stomach ulcers and indigestion
- indomethacin, used as a painkiller and anti-inflammatory
- co-trimoxazole, used to treat infections
- allopurinol, oxipurinol or thiopurinol, used mainly to treat gout
- tubocurarine, succinylcholine, used during anaesthesia
- frusemide, may be used to reduce swelling caused by excess fluid
- warfarin, used to prevent blood clots
- mesalazine, olsalazine or sulphasalazine, used mainly to treat ulcerative colitis
- phenytoin, phenobarbital, rifampicin, ketoconazole, erythromycin
- methotrexate, used in the treatment of cancer
- ribavirin, used to treat a type of respiratory infection.
These medicines may be affected by IMURAN Injection or may affect how well it works. You may need to take different amounts of your medicine or you may need to take different medicines. Your doctor or pharmacist has a more complete list of medicines to avoid while being given IMURAN Injection.
How it is given
How much is given
Your doctor will decide what dose you will receive. The dose will depend on the condition being treated, your bodyweight and how you respond to the treatment.
From time to time, while you are being given IMURAN Injection, your doctor will want you to have a blood test. This is to check your blood cell count and to change your dose if necessary.
How it is given
IMURAN Injection will be given to you under the supervision of a doctor.
It is a sterile powder which is dissolved and then diluted with suitable fluids before intravenous injection or infusion into a vein.
How long to have it for
Patients with a transplant will need to be given IMURAN continuously to reduce the risk of organ rejection.
For other conditions, your doctor will discuss with you how long you need to be given this medicine. It could take some weeks or months for it to take full effect.
If you are given too much (overdose)
As this medicine is given to you under the supervision of your doctor, it is extremely unlikely that you will be given too much.
However, if you experience any side effects after being given IMURAN Injection, tell your doctor or nurse immediately.
You may need urgent medical attention.
While you are having it
Things you must do
Visit your doctor regularly, so they can make sure that IMURAN Injection is working properly and to check for any unwanted side-effects.
Your doctor may order regular blood tests while you are having this medicine to check how it affects you. The frequency of your blood tests will usually decrease the longer you continue to take IMURAN Injection.
Tell any other doctor, dentist or pharmacist who is treating you that you are being given IMURAN Injection, especially if you are about to be started on any new medicines.
Tell your doctor if you have recently been vaccinated or immunised or plan to do so.
IMURAN Injection may affect the way some vaccines work or your reaction to the vaccine.
Tell your doctor if you become pregnant, are trying to become pregnant or planning to father a child.
If you have to have an operation, tell your surgeon and anaesthetist that you are being given IMURAN Injection.
Tell your doctor immediately if you notice new moles, changes in existing moles, any lumps on your body or you feel unwell.
Immunosuppressant drugs, like IMURAN Injection, lower the body's immune defence system. There may be an increased risk of developing infections or tumours, including skin cancer, whilst being given this medicine.
Protect yourself from the sun while you are being given IMURAN Injection.
If you go out in the sun, wear a hat, protective clothing and use sunscreen.
Avoid contact with anyone suffering from chickenpox or shingles.
Infection with chickenpox or shingles can become severe in patients having drugs such as IMURAN Injection.
Things to be careful of
Be careful driving or operating machinery until you know how IMURAN Injection affects you.
Side effects
Tell your doctor as soon as possible if you do not feel well while you are being given IMURAN Injection.
All medicines can have side effects. Sometimes they are serious, most of the time they are not. You may need medical treatment if you get some of the side effects.
Ask your doctor or pharmacist to answer any questions you may have.
Tell your doctor immediately if you notice any of the following:
- any infection or fever
- unexpected bruising or bleeding, black tarry stools or blood in the urine or stools
- new marks on skin or any change to marks that may have been there previously
- headache, stiff neck and extreme sensitivity to bright light
- nausea and vomiting
- tiredness, dizziness or generally unwell
- irregular heart beat
- you come into contact with anyone who is suffering from chickenpox or shingles
- sores in the mouth and on the lips
- feeling of ants creeping in or under the skin
- change in sense of smell or taste.
IMURAN could cause your hepatitisB to become active again.
Tell your doctor immediately, or go to Accident and Emergency at your nearest hospital if you notice any of the following symptoms:
- allergic type reactions e.g. skin rash, itching and difficulty breathing, wheezing or coughing
- muscle weakness, with or without a skin rash
- muscle pain or stiffness
- severe joint pain
- kidney problems
- feeling faint especially when standing up
- severe abdominal pain
- diarrhoea
- jaundice, a yellow discoloration of the skin/eyes
- serious skin reactions such as blistering or peeling.
Side-effects reported particularly in organ transplant patients are:
- viral, fungal and bacterial infections
- hair loss (particularly following a kidney transplant)
- diarrhoea, usually with blood and mucus
- stomach pain with fever and vomiting.
Tell your doctor if you notice anything else that is making you feel unwell, even if you think the problems are not connected with this medicine and are not referred to in this leaflet.
Other side effects not listed above may also occur in some people.
Do not be alarmed by this list of possible side-effects.
You may not experience any of them.
After using it
Storage
Normally your doctor will get IMURAN Injection from the hospital pharmacy or their consulting rooms. If you take your IMURAN Injection from the pharmacy to your doctor, it is important to store it in a safe place, away from heat and light, where the temperature stays below 25°C.
Keep this medicine where young children cannot reach it.
If for any reason you take your IMURAN Injection home, always ensure that it is stored in a safe place such as a locked cupboard, where children cannot reach it.
Product description
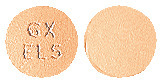
What it looks like
IMURAN Injection is supplied as a yellow to amber sterile powder in a glass vial. The powder is dissolved with sterile water and then further diluted with suitable fluids before it is used. Available in packs of 1 vial.
Ingredients
Active ingredient:
Each vial contains 50 mg of azathioprine.
Inactive ingredients:
- sodium hydroxide
- water for injections.
IMURAN Injection does not contain lactose, gluten, sucrose, tartrazine or any other azo dyes.
Sponsor
Aspen Pharmacare Australia Pty Ltd
34-36 Chandos St
St Leonards NSW 2065
Australia
Australian Registration Number:
AUST R 11102
This leaflet was revised in February 2012.

 C9H7N7O2S, molecular weight is 277.3.
C9H7N7O2S, molecular weight is 277.3.