What is in this leaflet
This leaflet answers some common questions about INLYTA.
It does not contain all the available information. It does not take the place of talking to your doctor or pharmacist.
All medicines have risks and benefits. Your doctor has weighed the risks of you taking INLYTA against the benefits it is expected to have for you.
If you have any concerns about taking this medicine, ask your doctor or pharmacist.
Keep this leaflet with the medicine. You may need to read it again.
What INLYTA is used for
What INLYTA does
INLYTA is used to treat a certain type of kidney cancer called renal cell carcinoma (RCC).
It belongs to a group of medicines called tyrosine kinase inhibitors.
How INLYTA works
INLYTA contains the active substance axitinib. It works by reducing the blood supply to the tumour and slowing down the growth of cancer.
Ask your doctor if you have any questions about why INLYTA has been prescribed for you. Your doctor may have prescribed it for another reason.
INLYTA is only available with a doctor's prescription. It is not addictive.
Use in Children
The safety and efficacy of INLYTA have not been established in children.
Before you take INLYTA
When you must not take it
Do not take INLYTA if you have an allergy to:
- any medicine containing axitinib
- any of the ingredients listed at the end of this leaflet
Some of the symptoms of an allergic reaction may include:
- shortness of breath
- wheezing or difficulty breathing
- swelling of the face, lips, tongue or other parts of the body
- rash, itching or hives on the skin.
Do not take this medicine after the expiry date printed on the pack or if the packaging is torn or shows signs of tampering. If it has expired or is damaged, return it to your pharmacist for disposal.
If you are not sure whether you should start taking this medicine, talk to your doctor.
Before you start to take it
Tell your doctor if you have allergies to any other medicines, foods, preservatives or dyes.
You must tell your doctor if you have or have had any of the following medical conditions:
- high blood pressure
- thyroid gland problems
- blood clots in your veins and/or arteries (types of blood vessels) or lungs
- stroke or heart attack
- bleeding problems
- you have an unhealed wound, or if you have surgery scheduled
- liver problems
- serious kidney problems (other than the kidney cancer for which you are being treated)
- lactose intolerance.
Before you start treatment with INLYTA, your doctor will perform tests to check for and monitor:
- blood pressure
- kidney problems
- thyroid levels
- red blood cell count
- liver enzyme levels
Before taking INLYTA your blood pressure should be well-controlled.
Tell your doctor if you are pregnant or plan to become pregnant or are breast-feeding. INLYTA should not be taken during pregnancy. Your doctor will discuss the risks with you.
You should not breastfeed while taking INLYTA.
If you have not told your doctor about any of the above, tell him/her before you start taking INLYTA.
Taking other medicines
Tell your doctor or pharmacist if you are taking any other medicines, including:
- all prescription medicines
- all medicines, vitamins, herbal supplements or natural therapies you buy without a prescription from a pharmacy, supermarket, naturopath or health food shop.
Some medicines may be affected by INLYTA or may affect how well it works. You may need different amounts of your medicines, or you may need to take different medicines. Your doctor will advise you.
Tell your doctor or pharmacist if you are taking any of the following:
- dexamethasone, a steroid medicine used to treat dermatitis, asthma and some other conditions
- ketoconazole or itraconazole, medicines used to treat fungal infections
- clarithromycin or telithromycin, antibiotics used to treat bacterial infections
- atazanavir, indinavir, nelfinavir, ritonavir or saquinavir, medicines used to treat HIV infections/AIDS
- rifampin or rifabutin, medicines used to treat tuberculosis (TB)
- nefazodone, used to treat depression
- phenytoin, carbamazepine or phenobarbital, anti-epileptic medicines used to stop seizures or fits
- St John's wort (Hypericum perforatum), a herbal medicine used to treat depression and other conditions
- theophylline, used to treat asthma or other lung diseases.
Your doctor and pharmacist have more information on medicines to be careful with or avoid while taking INLYTA.
How to take INLYTA
Follow all directions given to you by your doctor or pharmacist carefully. They may differ from the information contained in this leaflet.
If you do not understand the instructions on the label, ask your doctor or pharmacist for help.
How much to take
Your doctor will tell you which tablets you need to take each day. For kidney cancer, the usual starting dose of INLYTA is one 5 mg tablet taken 2 times a day (for a total of 2 tablets each day).
You doctor may subsequently increase or decrease your dose depending on your response to INLYTA.
While taking this medicine your blood pressure should be monitored. If you experience high blood pressure, your doctor may recommend medicine to treat it or may change your dose of INLYTA.
How to take it
Swallow the INLYTA tablets whole with a glass of water.
You can take INLYTA either with or without food.
Do not drink grapefruit juice or eat grapefruit while taking INLYTA. They may change the amount of INLYTA in your body.
When to take it
Take your medicine at about the same time each day. Taking it at the same time each day will have the best effect. It will also help you remember when to take it.
How long to take it
Continue taking INLYTA for as long as your doctor tells you.
This medicine helps to control your condition, but does not cure it. It is important to keep taking your medicine even if you feel well.
Continue taking your medicine for as long as your doctor prescribes it.
If you forget to take it
Take your next dose at your regular time.
Do not take a double dose to make up for the dose that you missed.
If you are not sure what to do, ask your doctor or pharmacist.
If you have trouble remembering to take your medicine, ask your pharmacist for some hints.
If you take too much (overdose)
Immediately telephone your doctor, or Poisons Information Centre (telephone Australia 13 11 26 or New Zealand 0800 POISON or 0800 764 766) for advice, or go to Accident and Emergency at the nearest hospital, if you think that you or anyone else may have taken too much INLYTA.
Do this even if there are no signs of discomfort or poisoning. You may need urgent medical attention.
While you are taking INLYTA
Things you must do
Make sure you follow your doctor's instructions and keep all appointments.
During treatment with INLYTA, your doctor will perform regular tests to check for and monitor:
- blood pressure
- heart disease
- stomach and bowel problems
- kidney disease
- thyroid levels
- red blood cell count
- liver enzyme levels
Regular follow up and blood tests are done to make sure the medicine is working and to check for side effects.
Men and women should use contraception to prevent pregnancy during treatment with INLYTA. Talk with your doctor about effective contraception.
If you become pregnant while taking this medicine, tell your doctor immediately.
If you are about to be started on any new medicine, remind your doctor and pharmacist that you are taking INLYTA.
Tell any other doctors, dentists, and pharmacists who treat you that you are taking this medicine.
If you are going to have surgery, tell the surgeon or anaesthetist that you are taking this medicine.
You should stop taking INLYTA 24 hours before your surgery. It may affect other medicines used during surgery.
If you are about to have any blood tests, tell your doctor that you are taking this medicine. It may interfere with the results of some tests.
Things you must not do
Do not take INLYTA to treat any other complaints unless your doctor tells you to.
Do not give your medicine to anyone else, even if they have the same condition as you.
Do not stop taking your medicine or lower the dosage without checking with your doctor.
Things to be careful of
Be careful driving, operating machinery or doing jobs that require you to be alert, until you know how INLYTA affects you. INLYTA may make some people feel very tired or dizzy.
If you feel light-headed, dizzy or faint when getting out of bed or standing up, get up slowly. Standing up slowly, especially when you get up from bed or chairs, will help your body get used to the change in position and blood pressure. If this problem continues or gets worse, talk to your doctor.
Side effects
Tell your doctor or pharmacist as soon as possible if you do not feel well while you are taking INLYTA.
All medicines can have side effects. Sometimes they are serious, most of the time they are not. You may need medical attention if you get some of the side effects.
It can be difficult to tell whether side effects are the result of taking INLYTA, effects of your condition or side effects of other medicines you may be taking. For this reason it is important to tell your doctor of any change in your condition.
Do not be alarmed by the list of side effects. You may not experience any of them.
Ask your doctor or pharmacist to answer any questions you may have.
Tell your doctor if...
Tell your doctor or pharmacist if you notice any of the following:
- diarrhoea
- high blood pressure
- tiredness
- loss of appetite
- hoarseness, change in your voice
- tingling or rash on palms of hands or soles of feet
- nausea (feeling sick) or vomiting
- weight loss
- weakness
- constipation
- low thyroid hormone levels, symptoms include being more sensitive to cold, unintentional weight gain and lack of energy
- soreness or burning of the mouth, tongue or throat
- shortness of breath, cough
- stomach ache, indigestion
- headache
- pain in hands or feet
- muscle pain, joint pain
- change in sense of taste
- rash, dry skin, skin redness, scaly skin, itchy skin
- dizziness
- dehydration
- nose bleeding
- piles, or bleeding from the back passage
- hair loss
- unusual urine colour
- ringing or sound in the ears
The above list includes the more common side effects of your medicine.
Tell your doctor as soon as possible if...
Tell your doctor as soon as possible if you notice any of the following:
- high blood pressure, symptoms may include headaches, dizziness, blurred vision, nausea and vomiting
- foamy and frothy urine with swelling of abdomen, legs or eyes
- swelling of feet or legs, leg pain, cough.
The above list includes serious side effects that may require medical attention.
Go to hospital if...
Tell your doctor immediately or go to Accident and Emergency at your nearest hospital, if you notice any of the following:
- chest pain or pressure, pain in your arms, back, neck or jaw; shortness of breath
- numbness or weakness on one side of your body, loss of co-ordination
- trouble speaking or swallowing
- headache, confusion, trouble seeing, seizures or fits
- severe stomach pain with vomiting and fever
The above list includes very serious side effects. You may need urgent medical attention or hospitalisation.
Tell your doctor or pharmacist if you notice anything else that is making you feel unwell. Other side effects not listed above may also occur in some people.
Some of these side effects (for example, changes in blood pressure, thyroid levels, liver enzymes and red blood cell count) can only be found when your doctor does tests from time to time to check your progress.
After using INLYTA
Storage
Keep your tablets in the pack until it is time to take them. If you take the tablets out of the pack they may not keep well.
Keep your tablets in a cool dry place where the temperature stays below 30°C.
Do not store INLYTA or any other medicine in the bathroom or near a sink. Do not leave it on a window sill or in the car. Heat and dampness can destroy some medicines.
Keep it where children cannot reach it. A locked cupboard at least one-and-a-half metres above the ground is a good place to store medicines.
Disposal
If your doctor tells you to stop taking this medicine or the expiry date has passed, ask your pharmacist what to do with any medicine that is left over.
Product description
What it looks like
INLYTA 1 mg are red, oval, film-coated tablets debossed with "Pfizer" on one side and "1 XNB" on the other.
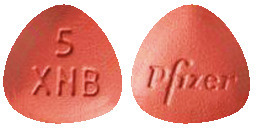
INLYTA 5 mg are red, triangular, film-coated tablets debossed with "Pfizer" on one side and "5 XNB" on the other.
INLYTA tablets are available in blister packs of 28 tablets (2 blister cards of 14 tablets each)
Ingredients
INLYTA tablets contain 1 mg or 5 mg of axitinib as the active ingredient.
The tablets also contain:
- lactose monohydrate
- cellulose - microcrystalline
- croscarmellose sodium
- magnesium stearate
- Opadry II RED 32K154441 film coating
- glycerol triacetinHPMC 2910/Hypromellose 15cP
- titanium dioxide
- iron oxide red CI77491
This medicine does not contain sucrose, gluten, tartrazine or any other azo dyes.
Supplier
INLYTA is supplied in Australia by:
Pfizer Australia Pty Ltd
ABN 50 008 422 348
Sydney NSW 2000
Toll Free number: 1800 675 229
www.pfizer.com.au
Australian registration numbers
1 mg tablets: AUST R 184856
5 mg tablets: AUST R 184859
Date of preparation
This leaflet was prepared in October 2019.
® = Registered Trademark
© Pfizer Australia Pty Ltd
Published by MIMS December 2019