What is in this leaflet
This leaflet answers some common questions about ITRACAP Itraconazole capsules.
It does not contain all the available information. It does not take the place of talking to your doctor or pharmacist.
All medicines have benefits and risks. Your doctor has weighed the risks of you taking ITRACAP against the benefits expected for you.
If you have any concerns about taking this medicine, talk to your doctor or pharmacist.
Keep this leaflet with your medicine. You may need to read it again.
What ITRACAP is used for
ITRACAP capsules are used to treat certain fungal infections which include the following:
- persistent infections of the nails, skin, hands, feet or groin;
- persistent candida (yeast) infections of vagina;
- eye infections which have not responded to other treatment or which may be affecting vision;
- candida (yeast) infections of the mouth or throat in patients with lower resistance to disease;
- generalised infections.
ITRACAP works by killing or stopping the growth of fungus that causes the infection.
Ask your doctor if you have any questions about why this medicine has been prescribed for you. Your doctor may have prescribed it for another reason.
Before you take ITRACAP
When you must not take it
Do not take ITRACAP if you have an allergy to:
- any medicine containing itraconazole
- any of the ingredients listed at the end of this leaflet. See Product Description at the end of this leaflet.
- you are pregnant or may become pregnant.
- If there is any chance of you becoming pregnant, talk to your doctor about the need for highly effective contraception. Once you have finished taking this medicine, you should continue using highly effective contraception until you have had your next period. Tell your doctor immediately if you do become pregnant while taking this medicine
- you have a condition called heart failure (also called congestive heart failure or CHF), this medicine could make it worse. If your doctor decides that you need to take this medicine even if you have this condition, be sure to get immediate medical help if you have shortness of breath, unexpected weight gain, swelling of the legs, unusual fatigue, or begin to wake up at night.
Some of the symptoms of an allergic reaction may include
- shortness of breath
- wheezing or difficulty breathing
- swelling of the face, lips, tongue or other parts of the body
- rash, itching or hives on the skin
- add any other specific reactions listed in the PI.
- Tell your doctor immediately if you do become pregnant while taking ITRACAP.
Do not take this medicine if you are pregnant or may become pregnant. It may affect your developing baby if you take it during pregnancy.
If there is any chance of you becoming pregnant, talk to your doctor about the need for highly effective contraception. Once you have finished taking itraconazole, you should continue using highly effective contraception until you have had your next period.
Tell your doctor immediately if you do become pregnant while taking ITRACAP.
Do not take this medicine if you have heart failure (also called congestive heart failure or CHF). ITRACAP could make it worse. If your doctor decides that you need to take ITRACAP even if you have this condition, be sure to get immediate medical help if you have shortness of breath, unexpected weight gain, swelling of the legs, unusual fatigue, or begin to wake up at night.
Do not take ITRACAP with any of the following medicines:
- terfenadine, astemizole or mizolastine (used for allergy or hay fever);
- bepridril felodipine, lercanidipine, ivabradine, ranolazine, eplerenone and nisoldipine (used to treat angina (crushing chest pain) and high blood pressure;
- domperidone (used to treat nausea and vomiting);
- ticagrelor (used for the prevention of heart attack or stroke);
- cisapride (used for certain digestive problems);
- certain medicines used to produce calmness or to help you sleep (midazolam (oral) or traizolam);
- simvastatin, lomitapide or lovastatin (used to lower your cholesterol);
- lurasidone, pimozide or sertindole (used to treat mental disorders);
- disopyramide, dronedarone, quinidine or dofetilide (used to treat irregular heartbeats);
- levacetylmethadol, methadone (used to treat severe pain or to manage opioid-dependency);
- dihydroergotamine and ergotamine (used to treat migraine);
- ergometrine or methylergometrine (used to control bleeding and maintain uterine contraction after child birth).
- halofantrine (used to treat malaria);
- irinotecan, an anti-cancer medicine;
- isavuconazole (used to treat fungal infections);
- naloxegol (used to treat constipation caused by taking opioid painkillers);
- avanafil (used to treat erectile dysfunction);
- dapoxetine (used to treat premature ejaculation);
- eliglustat (if you know you do not break down drugs that are broken down by the enzyme known as CYP2D6, you should check with your doctor if you can take this medicine).
- finerenone (used to treat kidney problems in patients with type 2 diabetes);
- voclosporin (used to treat lupusrelated kidney problems).
- If you have kidney or liver problems, do not take ITRACAP capsules with any of the following:
- colchicine (used to treat gout);
- fesoterodine or solifenacin (used to control irritated urinary bladder);
- telithromycin (an antibiotic).
If you have chronic lymphocytic leukemia/small lymphocytic lymphoma and you want to newly start this medicine or are making dose adjustments:
- venetoclax (used to treat certain cancers).
Wait at least 2 weeks after stopping ITRACAP capsules before taking any of these medicines.
Do not take this medicine after the expiry date printed on the pack or if the packaging is torn or shows signs of tampering. If it has expired or is damaged, return it to your pharmacist for disposal.
If you are not sure whether you should start taking this medicine, talk to your doctor.
Before you start to take it
Tell your doctor if you have allergies to any other medicines, foods, preservatives or dyes.
Tell your doctor if you:
- you are breastfeeding or wish to breastfeed;
- you have had allergic reactions to other medicines used to treat fungal infections;
- any liver problems;
- any kidney problems;
- heart problems;
- neutropenia or AIDS
- organ transplant patient
- cystic fibrosis
Tell your doctor if you are pregnant or plan to become pregnant or are breastfeeding.
If you have not told your doctor or pharmacist about any of the above, tell him/her before you start taking ITRACAP capsules.
Your doctor will advise whether or not to take ITRACAP or if you need to adjust the dose or adapt your treatment.
Taking other medicines
Tell your doctor or pharmacist if you are taking any other medicines, including any that you get without a prescription from a pharmacy, supermarket or health food shop.
In particular, ITRACAP capsules must not be taken with some medicines. Examples are:
- terfenadine, astemizole or mizolastine (used for allergy or hay fever);
- bepridil, felodipine, nisoldipine, lercanidipine, ivabradine, ranolazine, eplerenone (used to treat angina (crushing chest pain or high blood pressure);
- cisapride (used for certain digestive problems);
- certain medicines used to produce calmness or to help you sleep (midazolam (oral) or traizolam);
- simvastatin, lomitapide or lovastatin (used to lower your cholesterol);
- lurasidone, pimozide or sertindole (used to treat mental disorders);
- disopyramide, dronedarone, quinidine or dofetilide (used to treat irregular heartbeats);
- levacetylmethadol, methadone (used to treat severe pain and to manage opioid-dependency);
- ticagrelor (used for the prevention of heart attack or stroke);
- dihydroergotamine and ergotamine (used to treat migraine);
- ergometrine or methylergometrine (used to control bleeding and maintain uterine contraction after child birth).
- Halofantrine (used to treat malaria);
- irinotecan, an anti-cancer medicine;
- domperidone (used to treat nausea and vomiting);
- isavuconazole (used to treat fungal infections);
- naloxegol (used to treat constipation caused by taking opioid painkillers);
- avanafil (used to treat erectile dysfunction);
- dapoxetine (used to treat premature ejaculation;
- eliglustat (if you know you do not break down drugs that are broken down by the enzyme known as CYP2D6, you should check with your doctor if you can take this medicine).
Certain medicines are not recommended because they may be affected by ITRACAP capsules or may affect how well ITRACAP capsules work.
Your doctor may need to adjust the dose or adapt your treatment.
Examples of these medicines are:
- phenytoin, phenobarbital or carbamazepine (used to treat fits);
- bedaquiline, delamanid, rifampicin, rifabutin or isoniazid (used to treat tuberculosis);
- certain medicines used to treat HIV/AIDS, such as cobicistat, boosted elvitegravir, efavirenz, indinavir, maraviroc, nevirapine, saquinavir and ritonavir, ritonavir-boosted darunavir, ritonavir-boosted fosamprenavir, tenofovir disoproxil fumerate (TDF);
- boosted asunaprevir, bocoeprevir, daclatasvir, telaprevir, vaniprevir as HCV protease inhibitors (used to treat hepatitis C);
- glecaprevir/ pibrentasvir, elbasvir/grazoprevir; ombitasvir/paritaprevir/ritonavir (with or without dasabuvir) combinations, to treat Hepatitis C
- certain antineoplastics such as axitinib, bosutinib, bortezomib, brentuximab vedotin, busulphan, carbazitaxel, cabozanitinib, ceritinib, cobimetinib, crizotinib, dabrafenib, dasatinib, docetaxel, erlotinib, gefitinib, glasdegib, ibrutinib, idelalisib, imatinib, ixabepilone, lapatinib, nilotinib, nintedanib, Olaparib, panobinstat, pazopanib, ponatinib, regorafenib, ruxolitinib, sunitinib, sonidegib, talazoparib, trabectedin, trastuzumab emtansine, tretinoin (oral), vandetanib, vinca alkaloids (used to treat certain cancers); or docetaxel)
- sunitinib, used to treat certain types of bowel, stomach, or oesophagus tumours and kidney or pancreatic cancer
- gefitinib, used to treat breast, lung and other cancers
- imatinib, used to treat lung cancer
- conivaptan, tolvaptan or mozavaptan, used to treat low blood sodium levels
- aliskiren, diltiazem (to treat hypertension)
- bosentan, digoxin, nadolol, riociguat, and certain calcium channel blockers including dihydropyridines (e.g. amlodipine, nifedipine) and verapamil (used to treat heart or blood pressure problems);
- varopaxar (used to treat heart attacks or strokes);
- atorvastatin (used to lower cholesterol);
- anticoagulant medicines such as apixaban coumarins & coumarin-like medicines (e.g. warfarin), cilostazol, dabigatran, rivaroxaban (used to slow blood clotting);
- simeprevir and telaprevir as HCV protease inhibitors (used to treat hepatitis C);
- alfuzosin, dutasteride, soldosin (used to treat Benign Prostatic enlargement);
- sildenafil (used to treat erectile dysfunction or pulmonary hypertension);
- tadalafil, udenafil, vardenafil (used to treat erectile dysfunction);
- tolvaptan (used to treat low blood sodium levels);
- conivaptan, colchicine (used to treat gout);
- mozavaptan; to treat low blood sodium;
- fentanyl, a strong medicine for pain;
- alfentanil, buprenorphine, oxycodone, sufentanil (used in surgery for pain relief and to help anaesthesia);
- meloxicam, to treat join inflammation and pain;
- salmeterol (to improve breathing)
- darifenacin, fesoterodine, imidafenacin, oxybutynin, tolterodine (used to treat urinary incontinence);
- tamsulosin (used to treat male urinary incontinence)
- ciprofloxacin, clarithromycin, erythromycin, telithromycin (antibiotics);
- methylprednisolone, budesonide, ciclesondiate, fluticasone and dexamethasone (often used for conditions such as inflammations, asthma and allergies);
- bilastine, ebastine, rupatadine (used to treat allergies);
- everolimus (given after an organ transplant)
- ciclosporin, rapamycin (also known as sirolimus), tacrolimus, temsirolimus (used to help prevent organ transplant rejection or to treat certain problems with the immune system);
- trimetrexate (used to treat certain type of pneumonia);
- buspirone, perospirone, ramelteon, midazolam IV, alprazolam, brotizolam (used to treat anxiety or help you sleep);
- aripiprazole, cariprazine, haloperidol, quetiapine, risperidone; to treat psychosis;
- medicines taken for diabetes (in particular repaglinide and saxagliptin);
- aprepitant, netupitant (used for nausea and vomiting during cancer treatment)
- praziquantel, (used to treat fluke and tapeworms);
- some contraceptive pills (birth control pills); such as dienogest, ulipristal
- reboxetine, venlafaxine (used to treat depression and anxiety);
- cinacalcet, to treat an over active parathyroid;
- alitretinoin (oral formulation), to treat eczema;
- eletriptan (used to treat migraine);
- medicines which neutralize stomach acid or suppress the production of stomach acid (such as antacids, cimetidine, ranitidine, omeprazole);
- Saccharolmyces boulardii, loperamide (used to treat diarrhea);
- lumacaftor/ ivacaftor (used to treat Cystic Fibrosis);
- guanfacine (used to treat Attention Deficit Hyperactivity Disorder);
- suvorexant, zopiclone (used to treat insomnia);
- cabergoline (used to treat Parkinsons Disease;
- cannabinoids (used to treat nausea and vomiting, weight loss for patients with immune system problems and muscle spasms in patients with Multiple Sclerosis);
- artemether-lumefantrine, quinine (used to treat malaria);
- galantamine (used to treat Alzheimer's disease)
If you know you break down drugs that are handled/broken down by the enzyme CYP2D6 very quickly, you should check with your doctor if you can take this medicine as it may require a dose change:
- eliglustat
Medicines not recommended while you are on ITRACAP capsules, when you are on a stable dose of this medicine:
- venetoclax
Wait at least 2 weeks after stopping ITRACAP capsules before starting this medicine unless your doctor feels it is necessary. Taking ITRACAP capsules.
Your doctor and pharmacist have more information on medicines to be careful with or avoid while taking this medicine.
How to take ITRACAP
Follow all directions given to you by your doctor and pharmacist carefully. They may differ from the information contained in this leaflet.
If you do not understand the instructions on the box, ask your doctor or pharmacist for help.
How much to take
Adults
The usual doses are shown below, but your doctor may decide to adjust them for your individual needs.
Tinea of body and groin
1 capsule (100 mg) daily for 2 weeks.
Tinea of hands and feet
1 capsule (100 mg) daily for 4 weeks.
Other skin infections
2 capsules (200 mg) daily for 1 week.
Eye infections
2 capsules (200 mg) daily for 3 weeks.
Vaginal infections
2 capsules (200 mg) morning and evening for 1 day, or 2 capsules (200 mg) daily for 3 days.
Mouth infections
1 to 2 capsules (100 mg - 200 mg) daily for 4 weeks.
Systemic infections
1 to 2 capsules (100 mg to 200 mg) once or twice daily for 3 weeks to 8 months, depending on the condition.
Nail infections
Continuous nail therapy
2 capsules (200 mg) once daily for 3 months.
Cyclic (pulse) nail therapy
2 capsules (200 mg) twice daily for 1 week. After that, stop taking ITRACAP for 3 weeks. Then the cycle is repeated, once for fingernails and twice for toenail infections (with or without fingernail infections). (See below).
Fingernails only
Week 1: Take 2 capsules twice daily.
Week 2, 3, 4: No ITRACAP.
Week 5: Take 2 capsules twice daily.
Week 6: Stop.
Toenails with or without fingernails
Week 1: Take 2 capsules twice daily.
Week 2, 3, 4: No ITRACAP.
Week 5: Take 2 capsules twice daily.
Week 6, 7, 8: No ITRACAP.
Week 9: Take 2 capsules twice daily.
Week 10: Stop.
Children and Elderly
ITRACAP capsules are not recommended for use in children and in the elderly.
How to take it
Always take ITRACAP after a meal.
The capsules must be swallowed whole.
Do not take medicines that neutralise stomach acid within 2 hours of taking ITRACAP capsules. This is because sufficient stomach acid is required to ensure that ITRACAP capsule is properly absorbed by the body. If you take medicine that suppress the production of stomach acid, you should take your ITRACAP capsules with an acidic drink, such as a cola beverage.
If you forget to take it
Take the dose you missed as soon as you remember, and then continue taking your medicine as you would normally.
If it is almost time for your next dose, skip the dose you missed and take your next dose when you are meant to.
Do not take a double dose to make up for the dose you missed.
If you have missed more than one dose, or you are not sure what to do, ask your doctor or pharmacist.
If you have trouble remembering to take your medicine, ask your pharmacist for some hints.
If you take too much (overdose)
Immediately telephone your doctor or the Poisons Information Centre (telephone 13 11 26) for advice, or go to Accident and Emergency at the nearest hospital, if you think that you or anyone else may have taken too much ITRACAP. Do this even if there are no signs of discomfort or poisoning. You may need urgent medical attention.
While you are taking ITRACAP
Things you must do
Always follow your doctor's instructions carefully.
If you have to take ITRACAP capsules continuously for more than 1 month, your doctor may ask you to have your blood checked regularly to make sure that your liver is not affected.
If you become pregnant while taking this medicine, tell your doctor immediately.
If there is any chance of you becoming pregnant, talk to your doctor about the need for highly effective contraception. Once you have finished taking ITRACAP, you should continue using adequate contraception until you have had your next period.
If you are about to start taking a new medicine, tell your doctor and pharmacist that you are taking ITRACAP.
Tell any other doctors, dentists and pharmacists who treat you that you are taking this medicine.
Ask your doctor or pharmacist if you're not sure whether the treatment is working.
Always complete the treatment as directed by your doctor, even if the signs of infection have gone.
Things you must not do
Do not take ITRACAP capsules to treat any other complaints unless your doctor tells you to.
Do not give this medicine to anyone else, even if his or her symptoms seem similar to yours.
Do not stop taking your medicine or change the dosage without checking with your doctor.
Things to be careful of
You may feel dizzy while taking ITRACAP capsules. If you experience this or similar effects, you should avoid driving and using machines.
Make sure you know how you react to ITRACAP capsules before you drive a car, operate machinery or do anything else that could be dangerous if you are dizzy or lightheaded.
Side effects
Tell your doctor or pharmacist as soon as possible if you do not feel well while you are taking ITRACAP.
All medicines can have side effects. Sometimes they are serious, most of the time they are not. You may need medical attention if you get some of the side effects.
Do not be alarmed by the following list of side effects. You may not experience any of them.
Ask your doctor or pharmacist to answer any questions you may have.
Tell your doctor or pharmacist if you experience any of the following:
- upset stomach, stomach pain or discomfort, nausea, vomiting, diarrhoea, constipation, an unpleasant taste in your mouth.
- shortness of breath, headache, dizziness, fever.
- confusion
- cough, chills, cold or flu-like symptoms
- a change in menstrual pattern.
- unusual hair loss or thinning.
- erectile dysfunction.
- muscle weakness or pain, painful joints, tremors.
- High or low blood pressure
- Sleepiness
- Excessive sweating
- inflammation of the pancreas.
Tell your doctor as soon as possible if you notice any of the following as you may need urgent medical care:
- tingling, numbness or weakness in the hands or feet.
- swelling of hands ankles, feet, legs or abdomen.
- Increased heart rate
- Chest pain
- shortness of breath, unexpected weight gain, unusual fatigue, or begin to wake up at night.
- oversensitivity to sunlight.
- blurry or double vision, ringing in the ears.
- lose the ability to control your bladder or urinate much more than usual.
If any of the following happen, STOP taking ITRACAP and tell your doctor immediately or go to Accident and Emergency at your nearest hospital:
- abnormal tiredness, loss of appetite, nausea, vomiting, abdominal pain, dark urine, pale stools, yellowing of the skin or eyes (liver disorder).
- sudden signs of allergy such as rash, itching or hives on the skin, swelling of the face, lips, tongue or other parts of the body, shortness of breath or difficulty breathing, wheezing or trouble breathing.
- a severe skin disorder (widespread rashes with peeling skin and blisters in the mouth, eyes and genitals, or rashes with small pustules or blisters).
- you experience any hearing loss symptoms. In very rare cases, patients taking itraconazole have reported temporary or permanent hearing loss.
Other side effects not listed above may also occur in some people.
Tell your doctor if you notice are other effects.
After taking ITRACAP
Storage
Keep your capsules in the pack until it is time to take them. If you take the capsules out of the pack they may not keep well.
Keep your capsules in a cool dry place where the temperature stays below 25°C.
Do not store ITRACAP or any other medicine in the bathroom or near a sink. Do not leave it on a window sill or in the car. Heat and dampness can destroy some medicines.
Keep it where children cannot reach it. A locked cupboard at least one-and-a-half metres above the ground is a good place to store medicines.
Disposal
If your doctor tells you to stop taking this medicine or the expiry date has passed, ask your pharmacist what to do with any medicine that is left over.
Product description
What it looks like
ITRACAP capsules are a size "0el" hard gelatin white opaque capsules filled with off-white to cream coloured pellets and imprinting with 'ITR' on cap and '100' on body
They are supplied in a PVC/PE/PVDC/Al blister pack of 4, 6, 15, 28 and 60 capsules.
Not all pack sizes are available.
Ingredients
ITRACAP capsules contains 100 mg of itraconazole as the active ingredient.
It also contains the following inactive ingredients:
- hypromellose
- macrogol 20,000
- sucrose
- maize starch
- gelatin
- TekPrint SW-9008 Black Ink
This medicine does not contain lactose, gluten, tartrazine or any other azo dyes.
ITRACAP capsule contains sugars and sulfites. This medicine does not contain lactose, gluten, tartrazine or any other azo dyes.
Sponsor
Arrotex Pharmaceutical Pty Ltd
15 - 17 Chapel Street
Cremorne, VIC 3121
www.arrotex.com.au
Distributor
ITRACAP is distributed in Australia by:
Alphapharm Pty Ltd trading as Viatris
Level 1, 30 The Bond
30-34 Hickson Road
Millers Point NSW 2000
www.viatris.com.au
Phone 1800 274 276
Australian registration numbers:
ITRACAP itraconazole capsule blister pack 100 mg: AUST R 244472
This leaflet was prepared in September 2023.
ITRACAP® is a Viatris company trade mark
Published by MIMS November 2023

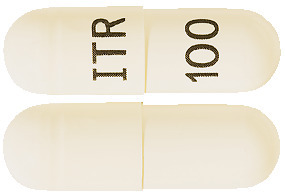






 Table 5 is a list of additional adverse effects associated with itraconazole that have been reported in clinical trials of itraconazole oral solution and/or itraconazole IV. The adverse effects are related to the active substance and are not specifically formulation dependent.
Table 5 is a list of additional adverse effects associated with itraconazole that have been reported in clinical trials of itraconazole oral solution and/or itraconazole IV. The adverse effects are related to the active substance and are not specifically formulation dependent.

 Chemical name: (+)-cis-4-[4-[4-[4-[[2-(2,4-dichlorophenyl)-2-(1H-1,2,4-triazol-1-ylmethyl)-1,3-dioxolan-4-yl] methoxy]phenyl]-1-piperazinyl]phenyl]-2,4-dihydro-2-(1-methylpropyl)-3H-1,2,4-triazol-3-one.
Chemical name: (+)-cis-4-[4-[4-[4-[[2-(2,4-dichlorophenyl)-2-(1H-1,2,4-triazol-1-ylmethyl)-1,3-dioxolan-4-yl] methoxy]phenyl]-1-piperazinyl]phenyl]-2,4-dihydro-2-(1-methylpropyl)-3H-1,2,4-triazol-3-one.