SUMMARY CMI
KEFLEX capsules/suspension
Consumer Medicine Information (CMI) summary
The full CMI on the next page has more details. If you are worried about using this medicine, speak to your doctor or pharmacist.
1. Why am I using KEFLEX?
KEFLEX contains the active ingredient cefalexin monohydrate. KEFLEX is used to treat infections caused by bacteria in different parts of the body, including infections of the respiratory tract (throat, tonsils, chest and lungs), nose (sinusitis), ears (otitis media), skin and soft tissue, kidneys and bladder (genitourinary tract).
For more information, see Section 1. Why am I using KEFLEX? in the full CMI.
2. What should I know before I use KEFLEX?
Do not use if you have ever had an allergic reaction to cefalexin monohydrate, penicillin, other cephalosporins or any of the ingredients listed at the end of the CMI.
Talk to your doctor if you have any other medical conditions, take any other medicines, or are pregnant or plan to become pregnant or are breastfeeding.
For more information, see Section 2. What should I know before I use KEFLEX? in the full CMI.
3. What if I am taking other medicines?
Some medicines may interfere with KEFLEX and affect how it works.
A list of these medicines is in Section 3. What if I am taking other medicines? in the full CMI.
4. How do I use KEFLEX?
- Follow all directions given to you by your doctor or pharmacist.
- You doctor will tell you how much and how often you should take KEFLEX.
More instructions can be found in Section 4. How do I use KEFLEX? in the full CMI.
5. What should I know while using KEFLEX?
| Things you should do |
|
| Things you should not do |
|
| Driving or using machines |
|
| Looking after your medicine |
|
For more information, see Section 5. What should I know while using KEFLEX? in the full CMI.
6. Are there any side effects?
For more information, including what to do if you have any side effects, see Section 6. Are there any side effects? in the full CMI.
FULL CMI
KEFLEX capsules/suspension
Active ingredient: cefalexin monohydrate
Consumer Medicine Information (CMI)
This leaflet provides important information about using KEFLEX. You should also speak to your doctor or pharmacist if you would like further information or if you have any concerns or questions about using KEFLEX.
Where to find information in this leaflet:
1. Why am I using KEFLEX?
2. What should I know before I use KEFLEX?
3. What if I am taking other medicines?
4. How do I use KEFLEX?
5. What should I know while using KEFLEX?
6. Are there any side effects?
7. Product details
1. Why am I using KEFLEX?
KEFLEX contains the active ingredient cefalexin monohydrate. This medicine belongs to a group of medicines called cephalosporins. These antibiotics work by killing the bacteria that are causing your infection.
KEFLEX is used to treat infections caused by bacteria in different parts of the body, including infections of the:
- respiratory tract (throat, tonsils, chest and lungs)
- nose (sinusitis)
- ears (otitis media)
- skin and soft tissue
- kidneys and bladder (genitourinary tract).
Ask your doctor or pharmacist if you have any questions about why this medicine has been prescribed for you.
Your doctor may have prescribed it for another reason.
There is no evidence that it is addictive.
2. What should I know before I use KEFLEX?
Warnings
Do not use KEFLEX if:
- you are allergic to cefalexin monohydrate, penicillin, other cephalosporins, or any of the ingredients listed at the end of this leaflet.
Some of the symptoms of an allergic reaction may include:
- shortness of breath, wheezing or difficulty breathing
- swelling of the face, lips, tongue or other parts of the body
- rash, itching or hives on the skin.
Always check the ingredients to make sure you can use this medicine. - the expiry date (EXP) on the pack has passed.
- the packaging is torn or shows signs of tampering.
Do not take KEFLEX suspension if it has been in your refrigerator for longer than two weeks.
If you are not sure whether you should start taking this medicine, talk to your doctor.
Check with your doctor if you:
- are allergic to any other medicines or any foods, preservatives or dyes.
- have any other medical conditions including
- liver disease
- kidney disease
- bowel disease.
If you have not told your doctor about any of the above, tell them before you start taking KEFLEX.
During treatment, you may be at risk of developing certain side effects. It is important you understand these risks and how to monitor for them. See additional information under Section 6. Are there any side effects?
Pregnancy and breastfeeding
Talk to your doctor if you are pregnant or intend to become pregnant or are breastfeeding.
Your doctor can discuss with you the risks and benefits involved.
3. What if I am taking other medicines?
Tell your doctor or pharmacist if you are taking any other medicines, including any medicines, vitamins or supplements that you buy without a prescription from your pharmacy, supermarket or health food shop.
Some medicines may interfere with KEFLEX and affect how it works.
These include:
- probenecid (e.g. Pro-Cid), a medicine commonly used to treat gout
- metformin, a medicine used in the treatment of diabetes.
These medicines may be affected by KEFLEX or may affect how well it works. You may need different amounts of your medicines or you may need to take different medicines.
Check with your doctor or pharmacist if you are not sure about what medicines, vitamins or supplements you are taking and if these affect KEFLEX.
4. How do I use KEFLEX?
Follow all directions given to you by your doctor or pharmacist.
They may differ from the information contained in this leaflet.
If you do not understand the instructions on the carton or bottle, ask your doctor or pharmacist for help.
How much to take
- Your doctor will tell you how much and how often you should take KEFLEX.
- This will depend on the type of infection. The dose varies from patient to patient.
When to take KEFLEX
- It does not matter if you take this medicine with or without food.
How to take KEFLEX
KEFLEX capsules:
- Swallow the capsules whole with a full glass of water.
KEFLEX suspension:
- Shake the bottle well and accurately measure the dose with a medicine measure.
Shaking the bottle and using a medicine measure will make sure that you get the correct dose. You can buy a medicine measure from your pharmacist.
How long to take KEFLEX
- Continue taking KEFLEX for as long as your doctor tells you.
It is important to complete the full course prescribed by your doctor, even if you begin to feel better after a few days. If you do not, the bacteria causing your infection may not clear completely or your symptoms may return.
If you forget to use KEFLEX
If it is almost time for your next dose, skip the dose you missed and take your next dose when you are meant to.
Otherwise, take it as soon as you remember, and then go back to taking your medicine as you would normally.
Do not take a double dose to make up for the dose you missed.
If you are not sure what to do, ask your doctor or pharmacist.
If you have trouble remembering to take your medicine, ask your pharmacist for some hints.
If you use too much KEFLEX
If you think that you have used too much KEFLEX, you may need urgent medical attention.
You should immediately:
- phone the Poisons Information Centre
(by calling 13 11 26), or - contact your doctor, or
- go to the Emergency Department at your nearest hospital.
You should do this even if there are no signs of discomfort or poisoning.
Symptoms of an overdose may include feeling sick in the stomach, diarrhoea, blood in the urine, unusually increased reflexes, convulsions or hallucinations.
5. What should I know while using KEFLEX?
Things you should do
- Tell your doctor if the symptoms of your infection do not improve within a few days or if they become worse.
- Tell any other doctors, dentists and pharmacists who are treating you that you are taking KEFLEX, especially if you are about to be started on any new medicines.
- Tell your doctor if you become pregnant while taking this medicine.
- If you are about to have any blood tests, tell your doctor that you are taking KEFLEX.
It may interfere with the results of some tests. - If you are diabetic, check with your doctor or pharmacist before using urine sugar tests.
KEFLEX may affect the results of some of these tests. - Keep all of your doctor's appointments so that your progress can be checked.
Your doctor may do some tests from time to time to make sure the medicine is working and to prevent unwanted side effects.
Things you should not do
- Do not stop using this medicine suddenly or change the dosage without first checking with your doctor.
If you stop taking it, your condition may worsen. - Do not take KEFLEX to treat any other complaints unless your doctor tells you to.
- Do not give your medicine to anyone else, even if they have the same condition as you.
Driving or using machines
Be careful before you drive or use any machines or tools until you know how KEFLEX affects you.
It may cause dizziness or drowsiness in some people.
Children should be careful when riding bicycles or climbing trees.
Looking after your medicine
KEFLEX capsules:
- Keep the capsules in the blister pack until it is time to take them.
- Keep it in a cool dry place where the temperature stays below 25°C. Do not store it in the bathroom or near a sink, in the car or on window sills.
KEFLEX suspension:
- Keep the suspension in the refrigerator between 2 and 8°C. Do not freeze.
- Keep the bottle tightly closed.
- The suspension should be shaken well before use and discarded after 14 days.
Keep it where young children cannot reach it.
Getting rid of any unwanted medicine
If you no longer need to use this medicine or it is out of date, take it to any pharmacy for safe disposal.
Do not use this medicine after the expiry date.
6. Are there any side effects?
Tell your doctor or pharmacist as soon as possible if you do not feel well while you are taking KEFLEX.
All medicines can have side effects. If you do experience any side effects, most of them are minor and temporary. However, some side effects may need medical attention.
See the information below and, if you need to, ask your doctor or pharmacist if you have any further questions about side effects.
Common side effects
| Common side effects | What to do |
| Speak to your doctor if you have any of these common side effects and they worry you. |
Serious side effects
| Serious side effects | What to do |
| Call your doctor straight away, or go straight to the Emergency Department at your nearest hospital if you notice any of these serious side effects. |
Tell your doctor immediately if you notice any of the following, particularly if they occur several weeks after stopping treatment with Keflex:
- severe stomach cramps or pain
- severe, watery or bloody diarrhoea
- fever, in combination with one of the above.
Do not take any diarrhoea medicine without first checking with your doctor.
You may have a serious condition affecting your bowel requiring urgent medical attention.
Tell your doctor or pharmacist if you notice anything else that may be making you feel unwell.
Other side effects not listed here may occur in some people. Do not be alarmed by this list of possible side effects. You may not experience any of them.
Reporting side effects
After you have received medical advice for any side effects you experience, you can report side effects to the Therapeutic Goods Administration online at www.tga.gov.au/reporting-problems. By reporting side effects, you can help provide more information on the safety of this medicine.
Always make sure you speak to your doctor or pharmacist before you decide to stop taking any of your medicines.
7. Product details
This medicine is only available with a doctor's prescription.
What KEFLEX contains
KEFLEX capsules:
| Active ingredient (main ingredient) | cefalexin monohydrate (equivalent to 250 mg or 500 mg of cefalexin) |
| Other ingredients (inactive ingredients) |
|
KEFLEX capsules do not contain lactose, sucrose, gluten, tartrazine or any other azo dyes.
KEFLEX suspension:
| Active ingredient (main ingredient) | cefalexin monohydrate (125 mg/5 mL or 250 mg/5 mL) |
| Other ingredients (inactive ingredients) |
|
KEFLEX suspensions do not contain lactose, gluten or tartrazine.
Do not take this medicine if you are allergic to any of these ingredients.
What KEFLEX looks like
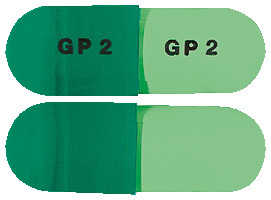
KEFLEX capsules:
KEFLEX 250 mg capsules are opaque dark green and white, marked with “GP1”on the cap and body. They are available in packs of 20 (AUST R 73522).
KEFLEX 500 mg capsules are opaque dark green and light green, marked with “GP2” on the cap and body. They are available in packs of 20 (AUST R 73523).
KEFLEX suspension:
Your pharmacist will make up the medicine in the bottle before dispensing it to you. The resulting suspension is pink.
It is available in two different strengths:
- 125 mg/5 mL (AUST R 92970)
- 250 mg/5 mL (AUST R 92971).
Who distributes KEFLEX
Aspen Pharmacare Australia Pty Ltd
34-36 Chandos Street
St Leonards NSW 2065
Australia
www.aspenpharmacare.com.au
This leaflet was revised in January 2024.
Published by MIMS March 2024


 In severe infections, the dosage may be doubled.
In severe infections, the dosage may be doubled.

