SUMMARY CMI
LATUDA®
Consumer Medicine Information (CMI) summary
The full CMI on the next page has more details. If you are worried about using this medicine, speak to your doctor or pharmacist.
1. Why am I using LATUDA?
LATUDA contains the active ingredient lurasidone hydrochloride. LATUDA is used to treat adults and adolescents (aged 13 years and over) with schizophrenia. It is only available with a doctor's prescription. For more information, see Section 1. Why am I using LATUDA? in the full CMI.
2. What should I know before I use LATUDA?
Do not use if you have ever had an allergic reaction to LATUDA or any of the ingredients listed at the end of the CMI.
Talk to your doctor if you have any other medical conditions, take any other medicines, or are pregnant or plan to become pregnant or are breastfeeding. LATUDA is not approved for treatment of elderly patients with dementia-related psychosis or behavioural disorders. For more information, see Section 2. What should I know before I use LATUDA? in the full CMI.
3. What if I am taking other medicines?
Some medicines may interfere with LATUDA and affect how it works.
A list of these medicines is in Section 3. What if I am taking other medicines? in the full CMI.
4. How do I use LATUDA?
Your doctor or pharmacist will tell you how many tablets you will need to take each day. This depends on your condition and whether or not you are taking any other medicines. Unless your doctor gives you other directions, you should take LATUDA only once a day. Take LATUDA during or immediately after food, consider evening meal. More instructions can be found in Section 4. How do I use LATUDA? in the full CMI. Continue taking the tablets for as long as your doctor tells you.
5. What should I know while using LATUDA?
| Things you should do |
|
| Things you should not do |
|
| Driving or using machines |
|
| Drinking alcohol |
|
| Looking after your medicine |
|
For more information, see Section 5. What should I know while using LATUDA? in the full CMI.
6. Are there any side effects?
All medicines can have side effects. If you do experience any side effects, most of them are minor and temporary. However, some side effects may need medical attention. Severe allergic reactions and other severe reactions such as nervous system or musculoskeletal related disorders have rarely been reported. Medical attention or hospitalisation may then be required and should be sought urgently from a doctor or Accident and Emergency at the nearest hospital. For more information, including what to do if you have any side effects, see Section 6. Are there any side effects? in the full CMI.
FULL CMI
LATUDA®
Active ingredient(s): Lurasidone Hydrochloride (pronounced lu-ra-si-done hy-dro-chl-ride)
Consumer Medicine Information (CMI)
This leaflet provides important information about using LATUDA. You should also speak to your doctor or pharmacist if you would like further information or if you have any concerns or questions about using LATUDA.
Where to find information in this leaflet:
1. Why am I using LATUDA?
2. What should I know before I use LATUDA?
3. What if I am taking other medicines?
4. How do I use LATUDA?
5. What should I know while using LATUDA?
6. Are there any side effects?
7. Product details
1. Why am I using LATUDA?
- LATUDA contains the active ingredient lurasidone hydrochloride.
LATUDA belongs to a group of medicines called atypical antipsychotics. It helps to correct chemical imbalances in the brain, which may cause mental illness.
- LATUDA is used to treat adults and adolescents (aged 13 years over with schizophrenia).
Schizophrenia is a mental illness with disturbances in thinking, feelings and behaviour.
Your doctor may have prescribed LATUDA for another reason.
Ask your doctor if you have any questions about why LATUDA has been prescribed for you.
LATUDA is not addictive or habit forming.
LATUDA is available only with a doctor's prescription.
LATUDA is not recommended for use in children or adolescents under 13 years of age, as safety and effectiveness have not been established in this age group.
LATUDA is not approved for the treatment of elderly patients with dementia-related psychosis or behavioural disorders. Medicines like LATUDA can increase the risk of death in elderly people who have memory loss (dementia).
2. What should I know before I use LATUDA?
There are some people who shouldn't take LATUDA. Please read the list below. If you think any of these situations apply to you or you have any questions, please see your doctor.
Warnings
Do not use LATUDA if:
- you are allergic to lurasidone hydrochloride, or any of the ingredients listed at the end of this leaflet.
- always check the ingredients to make sure you can use this medicine.
- you are taking medicines that can affect how your body processes LATUDA such as:
- ketoconazole or voriconazole, used to treat certain fungal infections
- ritonavir, used to treat HIV infection
- carbamazepine, used to treat convulsions (fits)
- phenytoin, used to treat convulsions (fits) and some heart conditions
- rifampicin or clarithromycin, used to treat bacterial infections
- herbal medicines derived from St. John's wort, used to treat depression - the packaging is torn or shows signs of tampering
- the expiry date (EXP) printed in the pack has passed
- If you are not sure whether you should start taking LATUDA, talk to your doctor or pharmacist.
Before you start to take it
Tell your doctor if you have allergies to:
- Any other medicines
- Any other substances, such as foods, preservatives or dyes
Talk to your doctor about how much alcohol you drink. People who drink excessive quantities of alcohol should not take LATUDA.
- If you have any doubts or questions about taking LATUDA consult your doctor.
Check with your doctor if you have or have had:
- dementia-related psychosis (particularly in the elderly)
- neuroleptic malignant syndrome, a reaction to some medicines with a sudden increase in body temperature, extremely high blood pressure and severe convulsions (fits)
- tardive dyskinesia, a reaction to some medicines with worm-like movements of the tongue, or other uncontrolled movements of the mouth, tongue, cheeks or jaws which may progress to the arms and legs
- diseases of the blood with a reduced number of white blood cells (e.g. leukopenia or neutropenia) which may result in fever or other signs of infection.
- diabetes, increased blood sugar (also known as hyperglycaemia), or have a family history of diabetes or high blood sugar.
- seizures
- suicidal thoughts or behaviour
- cardiovascular disease (e.g. heart failure, history of heart attack, ischemia, conduction abnormalities, or have a condition known as QT prolongation)
- changed levels of lipids such as cholesterol, triglycerides etc. in the blood (also known as dyslipidemia)
- high blood pressure (also known as hypertension) or low blood pressure (also known as hypotension) or fainting
- venous thromboembolism (e.g. blockage of a blood vessel by a blood clot formed elsewhere in the body)
- cerebrovascular disease (e.g. stroke, dehydration, low blood pressure), particularly in the elderly
- liver or kidney problems
- breast cancer, pituitary tumours (e.g. tumours at the base of the brain)
- high prolactin levels (which may present as breast swelling, unusual secretions of breast milk, missed or irregular menstrual periods, breast enlargement in men or impotence)
- difficulty swallowing
- weight gain
- sleep apnoea (temporarily stopping breathing while sleeping)
Tell your doctor if you are participating in activities that may contribute to an elevation in core body temperature (e.g. exercising strenuously, exposure to extreme heat) or subject you to dehydration.
During treatment, you may be at risk of developing certain side effects. It is important you understand these risks and how to monitor for them. See additional information under Section 6. Are there any side effects?
Pregnancy and breastfeeding
- Tell your doctor if you are pregnant or intend to become pregnant.
Like most atypical antipsychotic medicines, LATUDA is not recommended for use during pregnancy. However, if you need to take LATUDA during your pregnancy, your doctor will discuss with you the benefits and risks of taking it.
Newborn babies exposed to antipsychotic medicines (including LATUDA) during the third trimester of pregnancy are at risk of experiencing unusual movements of trembling and/or withdrawal symptoms following delivery including breathing problems, difficulty in feeding, spasms, restlessness, drowsiness.
Talk to your doctor if you are breastfeeding or intend to breastfeed.
It is recommended that you do not breast-feed while taking LATUDA, as it may pass into breast milk and therefore there is a possibility that the breast-fed baby may be affected. Be sure you have discussed with your doctor the risks and benefits of using this medicine while breast-feeding.
- If you have not told your doctor or pharmacist about any of the above, tell them before you start taking LATUDA.
3. What if I am taking other medicines?
Tell your doctor or pharmacist if you are taking any other medicines, including any medicines, vitamins or supplements that you buy without a prescription from your pharmacy, supermarket or health food shop.
- Some medicines may interfere with LATUDA and affect how it works. Medicines that can affect how your body processes LATUDA include:
- ketoconazole or voriconazole, used to treat certain fungal infections
- ritonavir, used to treat HIV infection
- carbamazepine, used to treat convulsions (fits)
- phenytoin, used to treat convulsions (fits) and some heart conditions
- rifampicin or clarithromycin, used to treat bacterial infections
- herbal medicines derived from St. John's wort, used to treat depression
These medicines may be affected by LATUDA or may affect how well it works. You may need different amounts of your medicine, or you may need to take different medicines. Your doctor will advise you.
- Check with your doctor or pharmacist if you are not sure about what medicines, vitamins or supplements you are taking and if these affect LATUDA.
4. How do I use LATUDA?
How much to take
- Follow all directions given to you by your doctor or pharmacist carefully.
They may differ from the information contained in this leaflet.
Your doctor or pharmacist will tell you how many tablets you will need to take each day. This depends on your condition and whether or not you are taking any other medicines.
- If you do not understand the instructions on the box, ask your doctor or pharmacist for help.
- Do not change your dose without the advice of your doctor even if you feel better.
Follow the instructions provided and take LATUDA until your doctor tells you to stop.
When to take LATUDA
- Swallow LATUDA whole with a glass of water. Do not chew the tablets.
- LATUDA should be taken during or immediately after food, consider evening meal.
- Unless your doctor gives you other directions, you should take LATUDA only once a day.
How to take LATUDA
- Continue taking the tablets for as long as your doctor tells you.
LATUDA helps control your condition but does not cure it. Therefore you must take LATUDA every day.
- Do not stop taking it unless your doctor tells you to – even if you feel better.
If you forget to take LATUDA
LATUDA should be used regularly at the same time each day. If you miss your dose at the usual time, take it as soon as you remember, and then go back to taking your medicine as you would normally.
- If it is almost time for your next dose, skip the dose you missed and take your next dose when you are meant to.
- Do not take a double dose to make up for the dose you missed.
This may increase the chance of you getting an unwanted side effect.
- If you are not sure what to do, ask your doctor or pharmacist.
- If you have trouble remembering to take your medicine, ask your pharmacist for some hints.
If you take too much LATUDA
- It is important that you do not take more LATUDA tablets than your doctor has prescribed.
If you think that you have used too much LATUDA, you may need urgent medical attention.
If you take too much, you may experience:
- fast, slow or irregular heartbeat
- low blood pressure (i.e. dizziness, light-headedness)
- reduced alertness
- seizures (i.e. fits)
- uncontrolled muscle spasms affecting the head and neck
You should immediately:
- phone the Poisons Information Centre
(by calling 13 11 26), or - contact your doctor, or
- go to the Emergency Department at your nearest hospital.
If anyone accidentally swallows any of your LATUDA tablets, call your nearest Poisons Information Centre for advice (Australian telephone: 13 11 26), or go to Accident and Emergency at your nearest hospital. Keep the telephone number for those places handy whilst taking any medications.
You should do this even if there are no signs of discomfort or poisoning.
5. What should I know while using LATUDA?
Things you should do
Tell any other doctors, dentists and pharmacists who are treating you that you are taking LATUDA if:
- you are about to be started on any new medicines
- you plan to have surgery that needs a general anaesthetic
- you become pregnant while taking LATUDA
- you need to have any medical tests while you are taking LATUDA
- you have signs of frequent infections such as fever, chills, sore throat or mouth ulcers
- you have hyperglycaemia (high blood sugar)
- you have a sudden increase in body temperature, sweating, fast heartbeat, muscle stiffness, high blood pressure and convulsions (these symptoms may be associated with a condition called ‘neuroleptic malignant syndrome’)
- dizziness on standing up, especially when getting up from a sitting or lying position (orthostatic hypotension) or fainting
- high blood prolactin levels (which may present as breast swelling, unusual secretion of breast milk, missed or irregular menstrual periods, breast enlargement in men or impotence)
LATUDA may affect the results of some tests.
Do not take any other medications, whether they require a prescription or not, without first telling your doctor that you are taking LATUDA as sometimes the action of one medicine may interfere with another.
- Tell your doctor if, for any reason, you have not taken your medicine exactly as prescribed. Otherwise your doctor may think that it was not effective and change your treatment unnecessarily.
Tell your doctor if you feel the tablets are not helping your condition.
Avoid eating grapefruit or drinking grapefruit juice during treatment with LATUDA. Grapefruit and grapefruit juice may affect the amount of LATUDA in your blood.
- Keep all your doctor's appointments so that your progress can be checked.
Call your doctor straight away if you:
- If you have any thoughts about suicide or doing harm to yourself, call your doctor immediately and also contact someone you trust.
All thoughts or talk about suicide or violence towards others or yourself are serious.
If you or someone you know is showing any of the following common warning signs, either contact your doctor or healthcare professional or go to the nearest hospital for treatment:
- worsening symptoms of depression or anxiety
- thoughts or talk about death or suicide
- thoughts or talk about self-harm or doing harm to others
- any recent attempts of self-harm
- an increase in aggressive behaviour, irritability or agitation
If someone you know shows any of these symptoms, suggest they urgently contact a healthcare professional.
In addition to talking to your doctor, confidential support and counselling services are available (in Australia) from LifeLine by calling 13 11 14.
Remind any doctor, dentist or pharmacist you visit that you are using LATUDA.
Things you should not do
- Do not stop taking LATUDA, or lower the dosage, even if you are feeling better, without checking with your doctor.
If you stop taking LATUDA suddenly, your condition may worsen or your chance of getting an unwanted side effect may increase.
To prevent this, your doctor may gradually reduce the amount of LATUDA you take each day before stopping completely.
- Do not take LATUDA to treat any other complaints unless your doctor tells you to.
- Do not take any medicines that cause drowsiness while you are taking LATUDA, unless recommended by your doctor.
- You should not take LATUDA together with certain medications (see also under “Do not use LATUDA if”) as they can affect how your body processes LATUDA.
Do not give LATUDA to anyone else, even if their symptoms seem similar or they have the same condition as you.
Things to be careful of
- Grapefruit and grapefruit juice should be avoided while taking LATUDA.
Grapefruit juice contains one or more components that alter the metabolism of some medicines including LATUDA. This may lead to higher and unpredictable levels of LATUDA in the blood.
Do not become too hot or dehydrated while taking LATUDA as your body's ability to reduce core body temperature may be affected.
Driving or using machines
- Be careful before you drive or use any machines or tools until you know how LATUDA affects you. Speak with your doctor about when you can resume these activities.
As with other antipsychotic medicines, LATUDA has the potential to impair judgement, thinking or motor skills in some people. Make sure you know how you react to LATUDA before you drive a car, operate machinery, or do anything else that could be dangerous if you are affected by LATUDA.
Drinking alcohol
- Tell your doctor if you drink alcohol. Talk to you doctor about how much alcohol you drink.
People who drink excessive quantities of alcohol should not take LATUDA.
Looking after your medicine
Follow the instructions in the carton on how to take care of your medicine properly.
Store it in a cool dry place away from moisture, heat or sunlight; for example, do not store it:
- in the bathroom or near a sink, or
- in the car or on window sills.
- Keep it where young children cannot reach it.
When to discard your medicine (as relevant)
Discard the medicine when the expiry date (EXP) printed on the pack has passed.
Getting rid of any unwanted medicine
If you no longer need to use this medicine or it is out of date, take it to any pharmacy for safe disposal.
Do not use this medicine after the expiry date.
6. Are there any side effects?
All medicines can have side effects. If you do experience any side effects, most of them are minor and temporary. However, some side effects may need medical attention.
See the information below and, if you need to, ask your doctor or pharmacist if you have any further questions about side effects.
Serious side effects
|
|
Severe allergic reaction exists with any medication. The following are general signs and symptoms of an allergic reaction:
|
|
Less serious side effects
|
|
Psychiatric disorders:
|
|
Tell your doctor or pharmacist if you notice anything else that may be making you feel unwell.
Other side effects not listed here may occur in some people.
Reporting side effects
After you have received medical advice for any side effects you experience, you can report side effects to the Therapeutic Goods Administration online at www.tga.gov.au/reporting-problems. By reporting side effects, you can help provide more information on the safety of this medicine.
Always make sure you speak to your doctor or pharmacist before you decide to stop taking any of your medicines.
7. Product details
This medicine is only available with a doctor's prescription.
What LATUDA contains
| Active ingredient (main ingredient) | lurasidone hydrochloride |
| Other ingredients (inactive ingredients) | carnauba wax, croscarmellose sodium, hypromellose, magnesium stearate, mannitol, Opadry complete film coating system 03F48969 white, pregelatinised maize starch, colourings: indigo carmine and iron oxide yellow (80 mg tablet only) |
| Potential allergens | LATUDA does not contain lactose, sucrose, gluten, tartrazine or any other azo dyes |
Do not take this medicine if you are allergic to any of these ingredients.
What LATUDA looks like
LATUDA is registered on the Australian register of Therapeutic Goods and has the Australia Register numbers:
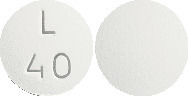
- AUST R 206650 – 40 mg tablets
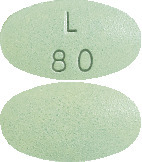
- AUST R 206651 – 80 mg tablets
LATUDA 40 mg tablets are round, white to off-white and debossed on one side with “L40”.
LATUDA 80 mg tablets are oval-shaped, pale green and debossed on one side with “L80”.
LATUDA tablets come in a blister strip. Each box contains 30 tablets.
Who distributes LATUDA
LATUDA is supplied in Australia by:
Servier Laboratories (Aust.) Pty. Ltd.
Level 4, Building 9,
588A Swan Street
Burnley, 3121, Victoria
Telephone: 1800 153 590
Internet: www.servier.com.au
This leaflet was prepared in August 2023.
Published by MIMS September 2023

 In long-term controlled studies, for patients who had normal BMI status at baseline (18.5 to < 25.0), the rate of clinically significant weight gain (≥ 7% increase in BMI) at month 12 was 12.4%, 34.5% and 5.6% and to study endpoint (LOCF) was 9.6%, 17.7% and 8.3% of the Latuda, risperidone and quetiapine XR groups, respectively. For those who were overweight at baseline (BMI 25.0 to < 30.0), the rate of clinically significant weight gain at study endpoint was 6.3%, 14.1% and 9.5%, in patients given Latuda, risperidone and quetiapine XR, respectively.
In long-term controlled studies, for patients who had normal BMI status at baseline (18.5 to < 25.0), the rate of clinically significant weight gain (≥ 7% increase in BMI) at month 12 was 12.4%, 34.5% and 5.6% and to study endpoint (LOCF) was 9.6%, 17.7% and 8.3% of the Latuda, risperidone and quetiapine XR groups, respectively. For those who were overweight at baseline (BMI 25.0 to < 30.0), the rate of clinically significant weight gain at study endpoint was 6.3%, 14.1% and 9.5%, in patients given Latuda, risperidone and quetiapine XR, respectively. The proportion of patients with prolactin elevations ≥ 5 x upper limit of normal (ULN) was 2.8% for Latuda treated patients versus 1.0% for placebo treated patients. The proportion of female patients with prolactin elevations ≥ 5 x ULN was 5.7% for Latuda treated patients versus 2.0% for placebo treated female patients. The proportion of male patients with prolactin elevations ≥ 5 x ULN was 1.6% versus 0.6% for placebo treated male patients.
The proportion of patients with prolactin elevations ≥ 5 x upper limit of normal (ULN) was 2.8% for Latuda treated patients versus 1.0% for placebo treated patients. The proportion of female patients with prolactin elevations ≥ 5 x ULN was 5.7% for Latuda treated patients versus 2.0% for placebo treated female patients. The proportion of male patients with prolactin elevations ≥ 5 x ULN was 1.6% versus 0.6% for placebo treated male patients.
 In long-term controlled studies the rate of markedly abnormal metabolic parameters was similar between Latuda, risperidone and quetiapine XR. For patients given any dose of Latuda the rate of shift from normal to high total cholesterol was 2.2% and triglycerides was 6.2%.
In long-term controlled studies the rate of markedly abnormal metabolic parameters was similar between Latuda, risperidone and quetiapine XR. For patients given any dose of Latuda the rate of shift from normal to high total cholesterol was 2.2% and triglycerides was 6.2%.





 Examination of population subgroups based on age (there were few patients over 65), gender and race did not reveal any clear evidence of differential responsiveness.
Examination of population subgroups based on age (there were few patients over 65), gender and race did not reveal any clear evidence of differential responsiveness.

