SUMMARY CMI
LOZANOC®
Consumer Medicine Information (CMI) summary
The full CMI on the next page has more details. If you are worried about taking this medicine, speak to your doctor or pharmacist.
WARNING: Important safety information is provided in a boxed warning in the full CMI. Read before taking this medicine.
1. Why am I taking LOZANOC?
LOZANOC contains the active ingredient itraconazole. LOZANOC is used to treat certain fungal infections which include the following: persistent infections of the nails, skin, hands, feet or groin; persistent candida (yeast) infections of the vagina; eye infections which have not responded to other treatment or which may be affecting vision; candida (yeast) infections of the mouth or throat in patients with lower resistance to disease; generalised infections. For more information, see Section 1. Why am I taking LOZANOC? in the full CMI.
2. What should I know before I take LOZANOC?
Do not take if you have ever had an allergic reaction to LOZANOC or any of the ingredients listed at the end of the CMI.
Talk to your doctor if you have any other medical conditions, take any other medicines, or are pregnant or plan to become pregnant or are breastfeeding. For more information, see Section 2. What should I know before I take LOZANOC? in the full CMI.
3. What if I am taking other medicines?
Some medicines may interfere with LOZANOC and affect how it works. A list of these medicines is in Section 3. What if I am taking other medicines? in the full CMI.
4. How do I take LOZANOC?
Only take as many LOZANOC capsules as you have been prescribed and ask your doctor or pharmacist if you are not sure. More instructions can be found in Section 4. How do I take LOZANOC? in the full CMI.
5. What should I know while taking LOZANOC?
| Things you should do |
|
| Things you should not do |
|
| Driving or using machines |
|
| Looking after your medicine |
|
For more information, see Section 5. What should I know while taking LOZANOC? in the full CMI.
6. Are there any side effects?
Common side effects include: stomach upset/pain/discomfort, nausea, vomiting, diarrhoea, constipation, unpleasant taste in mouth, shortness of breath, headache, dizziness, fever, change in menstrual pattern, hair loss/thinning, erectile dysfunction, muscle weakness/pain, painful joints, tremors, confusion, cough, chills, high or low blood pressure. Serious side effects include: tingling/numbness/weakness in hands/feet, swelling of hands/ankles/feet/legs/abdomen, shortness of breath, weight gain, tiredness/fatigue/beginning to wake up at night, oversensitivity to sunlight, blurry/double vision, ringing in ears, loss of ability to control bladder/urinating more, loss of appetite, nausea, vomiting, dark urine, pale stools, yellowing of skin/eyes, sudden signs of allergy (rash/itching/hives on skin, swelling of the face/lips/tongue/other parts of the body, shortness of breath/trouble breathing), severe skin disorder (widespread skin rashes/peeling and blisters in mouth/eyes/genitals), any hearing loss symptoms. For more information, including what to do if you have any side effects, see Section 6. Are there any side effects? in the full CMI.
WARNING: DO NOT SUBSTITUTE LOZANOC with other brands of itraconazole, as they are not interchangeable. LOZANOC has a higher absorption than other itraconazole capsules and requires a different dose. For dosing information refer to section 4. How do I take LOZANOC?
FULL CMI
LOZANOC®
Active ingredient(s): itraconazole
Consumer Medicine Information (CMI)
This leaflet provides important information about taking LOZANOC. You should also speak to your doctor or pharmacist if you would like further information or if you have any concerns or questions about taking LOZANOC.
Where to find information in this leaflet:
1. Why am I taking LOZANOC?
2. What should I know before I take LOZANOC?
3. What if I am taking other medicines?
4. How do I take LOZANOC?
5. What should I know while taking LOZANOC?
6. Are there any side effects?
7. Product details
1. Why am I taking LOZANOC?
LOZANOC contains the active ingredient itraconazole. LOZANOC works by killing or stopping the growth of the fungus that causes the infection.
LOZANOC is used to treat certain fungal infections which include the following:
- persistent infections of the nails, skin, hands, feet or groin;
- persistent candida (yeast) infections of the vagina;
- eye infections which have not responded to other treatment or which may be affecting vision;
- candida (yeast) infections of the mouth or throat in patients with lower resistance to disease;
- generalised infections.
2. What should I know before I take LOZANOC?
Warnings
Do not take LOZANOC if:
- you are allergic to itraconazole, or any of the ingredients listed at the end of this leaflet.
Always check the ingredients to make sure you can take this medicine. - you have a condition called heart failure (also called congestive heart failure or CHF), LOZANOC could make it worse.
- you are pregnant or may become pregnant.
Do not take LOZANOC with any of the following medicines:
- certain medicines for allergy or hay fever (e.g. terfenadine, astemizole, mizolastine);
- certain medicines used to treat angina and high blood pressure (e.g. bepridil, felodipine, nisoldipine, lercanidipine, ranolazine, eplerenone) and ivabradine, a heart rate lowering agent;
- anticoagulants (used to slow blood clotting), such as apixaban, rivaroxaban, dabigatran;
- cisapride, a drug used to treat gastric reflux;
- domperidone, an antiemetic used to treat nausea, vomiting, bloating and fullness;
- levomethadyl and methadone, which are opioids;
- antipsychotic medications, such as pimozide, lurasidone and sertindole;
- ticagrelor, an anticoagulant;
- halofantrine, a medicine used to treat malaria;
- isavuconazole, an antifungal medicine;
- naloxegol, a medicine used to reduce opioid constipation;
- avanafil, a drug used for erectile dysfunction and dapoxetine, used for premature ejaculation;
- eliglustat, used to treat Gaucher disease;
- irinotecan, mobocertinib (used to treat cancer);
- venetoclax (used to treat certain cancers) in patients just starting or adjusting the dose of venetoclax;
- certain medicines used to produce calmness or to help you sleep (midazolam oral or triazolam);
- certain medicines used to lower your cholesterol, known as HMG-CoA reductase inhibitors, (e.g. simvastatin, lomitapide, lovastatin);
- dronedarone, dofetilide, quinidine or disopyramide (used to treat irregular heartbeats);
- dihydroergotamine or ergotamine (used to treat migraine);
- fesoterodine and solifenacin in patients with moderate to severe liver or kidney disease (these are medicines used to treat overactive bladder);
- colchicine in patients with severe liver or kidney disease (medicine used to treat gout and Behcet's disease);
- telithromycin in patients with severe liver or kidney disease (an antibiotic used to treat pneumonia);
- ergometrine or methylergometrine (used to control bleeding);
- finerenone (used to treat kidney problems in patients with type II diabetes);
- voclosporin (used to treat lupus-related kidney problems).
Check with your doctor if you:
- have or have had any other medical conditions, in particular:
- liver or kidney problems;
- allergic reaction to other medicines used to treat fungal infections;
- heart problems;
- neutropenia (low levels of a type of white blood cells) or AIDS or an organ transplant patient;
- hearing problems;
- weakness, numbness and pain from nerve damage, usually in the hands and feet;
- cystic fibrosis. - take any medicines for any other condition;
- you have allergies to any other medicines, foods, preservatives or dyes.
During treatment, you may be at risk of developing certain side effects. It is important you understand these risks and how to monitor for them. See additional information under Section 6. Are there any side effects?
Pregnancy and breastfeeding
Check with your doctor if you are pregnant or intend to become pregnant.
If there is a chance you may become pregnant, talk to your doctor about the need for highly effective contraception. Once you have finished LOZANOC, contraception should be continued until you have had your next period. Tell your doctor immediately, if you do become pregnant.
Talk to your doctor if you are breastfeeding or intend to breastfeed. Your doctor can discuss with you the risks and benefits involved.
3. What if I am taking other medicines?
Tell your doctor or pharmacist if you are taking any other medicines, including any medicines, vitamins or supplements that you buy without a prescription from your pharmacy, supermarket or health food shop.
In particular, LOZANOC must not be taken with some medicines. Wait at least 2 weeks after stopping LOZANOC before taking any of these medicines. Examples are provided in section 2. “Do not take LOZANOC with any of the following medicines”
Some medicines may be affected by LOZANOC or may interfere with LOZANOC and affect how it works. Your doctor may need to adjust the dose or adapt your treatment.
Examples of these medicines are:
- alfuzosin, tamsulosin, silodosin (used to treat Benign Prostatic enlargement);
- alfentanil, buprenorphine, oxycodone, sufentanil (used in surgery for pain relief and to help anaesthesia);
- fentanyl, a strong medicine for pain;
- digoxin (used to treat heart failure);
- bedaquiline, delamanid, rifampicin, rifabutin or isoniazid (used to treat tuberculosis);
- ciprofloxacin, erythromycin, clarithromycin, (antibiotics);
- trimetrexate, used to treat a certain type of pneumonia;
- anticoagulants (used to slow blood clotting), such as, edoxaban, vorapaxar, coumarins and coumarin like medicines (e.g. warfarin); phenytoin, phenobarbital or carbamazepine (used to treat fits);
- medicines taken for diabetes, such as repaglinide and saxagliptin;
- praziquantel, a worm medication;
- artemether-lumefantrine, quinine (used to treat malaria);
- bilastine, ebastine, rupatadine (used to treat allergies);
- eletriptan (used to treat migraine);
- certain antineoplastics such as axitinib, bosutinib, bortezomib, brentuximab vedotin, busulfan, cabazitaxel, cabozanitinib, ceritinib, cobimetinib, crizotinib, dabrafenib, dasatinib, docetaxel, erlotinib, entrectinib, gefitinib, glasdegib, imatinib, ibrutinib, idelalisib, ixabepilone, lapatinib, nilotinib, nintedanib, olaparib, panobinstat, pazopanib, pemigatinib, ponatinib, regorafenib, ruxolitinib, sonidegib, sunitinib, talazoparib, trabectedin, trastuzumab emtansine, tretinoin (oral), vandetanib, vinca alkaloids (used to treat certain cancers);
- alprazolam, aripiprazole, brotizolam, buspirone, cariprazine, haloperidol, midazolam i.v., perospirone, quetiapine, ramelteon, risperidone, suvorexant, zopiclone, (used to treat anxiety or help you sleep);
- certain medicines used to treat AIDS, such as cobicistat, darunavir (boosted), efavirenz, elvitegravir (boosted), fosamprenavir (ritonavirboosted), indinavir, maraviroc, nevirapine, saquinavir, tenofovir disoproxil fumarate, or ritonavir;
- boosted asunaprevir, boceprevir, daclatasvir, elbasvir/grazoprevir, glecaprevir/pibrentasvir, ombitasvir/paritaprevir/ritonavir (with or without dasabuvir), vaniprevir (used to treat hepatitis C);
- aliskiren, bosentan, nadolol or riociguat (used to treat heart or blood pressure problems or hypertension);
- sildenafil or tadalafil (used to treat erectile dysfunction or pulmonary hypertension);
- certain calcium channel blockers (used to treat heart or blood pressure problems), such as diltiazem, verapamil or other dihydropyridines;
- contraceptives such as, dienogest or ulipristal;
- aprepitant, netupitant (used for nausea and vomiting during cancer treatment);
- Saccharomyces boulardii, loperamide (used to treat diarrhoea);
- budesonide, ciclesonide, cyclosporin, dexamethasone, fluticasone, methylprednisolone, sirolimus, tacrolimus, temsirolimus or everolimus (used to help prevent organ transplant rejection or to treat certain problems with the immune system);
- atorvastatin (used to lower cholesterol);
- meloxicam (a non-steroidal anti-inflammatory drug);
- salmeterol, a respiratory drug;
- reboxetine or venlafaxine (used to treat depression);
- darifenacin, vardenafil, dutasteride, imidafenacin, oxybutynin, tolterodine or udenafil (used to treat urinary disorders);
- cinacalcet, to treat an over active parathyroid;
- alitretinoin (oral formulation), to treat eczema;
- cabergoline (used to treat Parkinson's Disease);
- cannabinoids (used to treat nausea and vomiting, weight loss for patients with immune system problems and muscle spasms in patients with Multiple Sclerosis);
- galantamine (used to treat Alzheimer's disease);
- ivacaftor, lumacaftor/ivacaftor (used to treat Cystic Fibrosis);
- guanfacine (used to treat attention deficit hyperactivity disorder and high blood pressure);
- conivaptan, tolvaptan, mozavaptan (used to treat low blood sodium levels);
- medicines used to reduce stomach acid such as antacids, H2 antagonists (e.g. ranitidine) proton pump inhibitors (e.g. omeprazole).
Check with your doctor or pharmacist if you are not sure about what medicines, vitamins or supplements you are taking and if these affect LOZANOC.
4. How do I take LOZANOC?
How much to take/How long to take LOZANOC
Adults
LOZANOC is specially designed to give higher blood levels of active ingredient than other formulations of itraconazole capsules. A 50 mg capsule of LOZANOC is therapeutically equivalent to 100 mg of other brands of itraconazole capsules but the capsules are not interchangeable.
Only take as many LOZANOC capsules as you have been prescribed and ask your doctor or pharmacist if you are not sure.
The usual doses are shown below, but your doctor may decide to adjust them for your individual needs.
Tinea of body & groin:
1 capsule daily for 2 weeks.
Tinea of hands & feet:
1 capsule daily for 4 weeks.
Other skin infections:
2 capsules daily for 1 week.
Eye infections:
2 capsules daily for 3 weeks.
Vaginal infections:
2 capsules morning & evening for 1 day, or 2 capsules daily for 3 days.
Mouth infections:
1 to 2 capsules daily for 4 weeks.
Systemic infections:
1 to 2 capsules once or twice daily for 3 weeks to 8 months, depending on the condition.
Nail infections:
Continuous nail therapy: 2 capsules once daily for 3 months.
Cyclic (pulse) nail therapy: 2 capsules twice daily for 1 week. After that, stop taking LOZANOC for 3 weeks. Then the cycle is repeated, once for fingernails and twice for toenail infections (with or without fingernail infections).
Follow the instructions provided when LOZANOC was prescribed, including the number of days it should be taken.
Don't worry if you don't see an immediate improvement after your treatment.
- With skin infections, the marks or spots (lesions) typically disappear a few weeks after you finish the course. Although the medicine kills the fungus, the marks don't disappear until after new skin has grown.
- With nail infections, marks on the nail may take 6 to 9 months to disappear, because new nail needs to grow.
Ask your doctor or pharmacist if you're not sure whether the treatment is working.
Children and Elderly
LOZANOC is not recommended for use in children and in the elderly.
When to take LOZANOC
LOZANOC can be taken before or after a meal.
If you forget to take LOZANOC
LOZANOC should be taken regularly at the same time each day.
If it is almost time for your next dose, skip the dose you missed and take your next dose when you are meant to.
Do not take a double dose to make up for the dose you missed.
If you are not sure what to do, ask your doctor or pharmacist.
If you have trouble remembering when to take your medicine, ask your pharmacist for some hints.
If you take too much LOZANOC
If you think that you have taken too much LOZANOC, you may need urgent medical attention.
You should immediately:
- phone the Poisons Information Centre
(by calling 13 11 26), or - contact your doctor, or
- go to the Emergency Department at your nearest hospital.
You should do this even if there are no signs of discomfort or poisoning.
5. What should I know while taking LOZANOC?
Things you should do:
Always follow your doctor's instructions carefully.
If you have to take LOZANOC continuously for more than 1 month, your doctor may ask you to have your blood checked regularly to make sure that your liver is not affected.
Always complete the treatment as directed by your doctor, even if the signs of infection have gone.
Call your doctor straight away if you:
- become pregnant while taking this medicine.
If there is any chance of you becoming pregnant, talk to your doctor about the need for adequate contraception.
Remind any doctor, dentist or pharmacist you visit that you are taking LOZANOC.
Things you should not do:
- Do not take LOZANOC to treat any other complaint unless your doctor says so.
- Do not give this medicine to anyone else, even if their symptoms seem similar to yours.
Driving or using machines
Be careful before you drive or use any machines or tools until you know how LOZANOC affects you.
LOZANOC may cause dizziness in some people.
If you experience this or similar effects, you should avoid driving and using machines.
Make sure you know how you react to LOZANOC before you drive a car, operate machinery or do anything else that could be dangerous if you are dizzy or lightheaded.
Looking after your medicine
- Keep the LOZANOC capsules in the pack until it is time to take them. If you take the capsules out of the pack, they may not keep well.
- Store below 25°C.
Follow the instructions in the carton on how to take care of your medicine properly.
Store it in a cool dry place away from moisture, heat or sunlight; for example, do not store it:
- in the bathroom or near a sink, or
- in the car or on windowsills.
Keep it where young children cannot reach it.
When to discard your medicine/Getting rid of any unwanted medicine
If you no longer need to take this medicine or it is out of date, take it to any pharmacy for safe disposal.
Do not take this medicine after the expiry date.
6. Are there any side effects?
All medicines can have side effects. If you do experience any side effects, most of them are minor and temporary. However, some side effects may need medical attention.
See the information below and, if you need to, ask your doctor or pharmacist if you have any further questions about side effects.
Less serious side effects
| Less serious side effects | What to do |
| Speak to your doctor if you have any of these less serious side effects and they worry you. |
Serious side effects
| Serious side effects | What to do |
| Call your doctor straight away, or go straight to the Emergency Department at your nearest hospital if you notice any of these serious side effects. |
| STOP taking LOZANOC and call your doctor straight away, or go straight to the Emergency Department at your nearest hospital if you notice any of these serious side effects. |
Tell your doctor or pharmacist if you notice anything else that may be making you feel unwell.
Other side effects not listed here may occur in some people.
Reporting side effects
After you have received medical advice for any side effects you experience, you can report side effects to the Therapeutic Goods Administration online at www.tga.gov.au/reporting-problems. By reporting side effects, you can help provide more information on the safety of this medicine.
Always make sure you speak to your doctor or pharmacist before you decide to stop taking any of your medicines.
7. Product details
This medicine is only available with a doctor's prescription.
What LOZANOC contains
| Active ingredient (main ingredient) | itraconazole |
| Other ingredients (inactive ingredients) |
|
| Potential allergens | LOZANOC does not contain lactose or gluten. |
Do not take this medicine if you are allergic to any of these ingredients.
What LOZANOC looks like
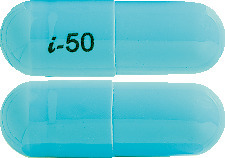
LOZANOC capsules are blue opaque capsules with i-50 printed in black.
They are supplied in a blister pack or bottle pack.
Blister pack AUST R 206361
Bottle pack AUST R 206360
Who distributes LOZANOC?
Mayne Pharma International Pty Ltd
1538 Main North Road
Salisbury South, SA 5106
This leaflet was prepared in January 2024
Published by MIMS March 2024

 An alternative dosage regimen for dermatomycosis of nails (onychomycosis) is pulsed therapy. A pulse treatment consists of two capsules twice daily for one week. Two pulse treatments are recommended for fingernail infections, three pulse treatments for toenail infections. Pulse treatments are always separated by a 3 week drug free interval. Clinical response will become evident as the nail regrows, following discontinuation of the treatment.
An alternative dosage regimen for dermatomycosis of nails (onychomycosis) is pulsed therapy. A pulse treatment consists of two capsules twice daily for one week. Two pulse treatments are recommended for fingernail infections, three pulse treatments for toenail infections. Pulse treatments are always separated by a 3 week drug free interval. Clinical response will become evident as the nail regrows, following discontinuation of the treatment.




 For the effect (middle column) the name of the parent drug is stated, even when the effect is related to the active moiety or the active metabolite of a prodrug.
For the effect (middle column) the name of the parent drug is stated, even when the effect is related to the active moiety or the active metabolite of a prodrug. The following is a list of additional adverse effects associated with itraconazole. The adverse effects are related to the active substance and are not specifically formulation dependent. See Table 6.
The following is a list of additional adverse effects associated with itraconazole. The adverse effects are related to the active substance and are not specifically formulation dependent. See Table 6.

 The following clinical trials were conducted with a conventional formulation of itraconazole. One capsule of Lozanoc 50 mg is therapeutically equivalent to one 100 mg capsule of conventional itraconazole capsules. The recommended dose for Lozanoc is therefore half the recommended dose for conventional itraconazole capsules.
The following clinical trials were conducted with a conventional formulation of itraconazole. One capsule of Lozanoc 50 mg is therapeutically equivalent to one 100 mg capsule of conventional itraconazole capsules. The recommended dose for Lozanoc is therefore half the recommended dose for conventional itraconazole capsules. Molecular formula: C35H38CI2N8O4.
Molecular formula: C35H38CI2N8O4.