What is in this leaflet
This leaflet answers some common questions about MELOXIBINDO. It does not contain all available information, nor does it take the place of talking to your doctor or pharmacist.
All medicines have risks and benefits. Your doctor has weighed the risks of you taking MELOXIBINDO against the benefits they expect it will have for you.
Keep this information.
You may need to read it again later.
If you have any concerns about taking this medicine, ask your doctor or pharmacist.
What MELOXIBINDO is used for
MELOXIBINDO is used to treat the symptoms of:
- osteoarthritis
- rheumatoid arthritis
Both diseases mainly affect the joints causing pain and swelling.
Although MELOXIBINDO can relieve symptoms such as pain and inflammation, it will not cure your condition.
MELOXIBINDO belongs to a family of medicines called Non-Steroidal Anti-inflammatory Drugs (NSAIDs). These medicines work by relieving pain and inflammation.
Ask your doctor if you have any questions about why MELOXIBINDO has been prescribed for you.
Your doctor may have prescribed MELOXIBINDO for another reason.
Before you take MELOXIBINDO
When you must not take it
Do not take MELOXIBINDO if you have an allergy to:
- the active ingredient, meloxicam, or any of the other ingredients in MELOXIBINDO (all of these ingredients are listed at the end of this leaflet). This includes rare inherited conditions of galactose intolerance.
- aspirin or any other NSAID medicine.
Some of the symptoms of an allergic reaction may include:
- rash, itching or hives on the skin
- swelling of the face, lips, tongue or other parts of the body
- shortness of breath, wheezing or troubled breathing.
Ask your doctor if you are unsure if you are allergic to these ingredients.
Do not take MELOXIBINDO if:
- you are about to undergo coronary artery bypass graft surgery
- you have a disease of the heart with shortness of breath, and swelling of the feet or lips due to fluid build-up
- you experience bleeding from the stomach, gut or any other bleeding
- you have had a stroke resulting from a bleed in the brain or have a bleeding disorder
- you are breastfeeding, or intend to breastfeed.
The active ingredient in MELOXIBINDO may pass into breast milk and may affect your baby.
- you currently have a peptic (stomach) ulcer
- you have Crohn’s Disease or Ulcerative Colitis
- you have severe liver or kidney problems
- you are currently taking other medicines known as: sulfinpyrazone (used to treat gout), fluconazole (used to treat fungal infections) or certain sulfur antibiotics (eg. sulfaphenazole or sulfamethoxazole).
Do not give MELOXIBINDO to children and adolescents under 18 years of age.
Do not take MELOXIBINDO if the packaging is torn or shows signs of tampering.
Do not take MELOXIBINDO if the EXPIRY DATE printed on the pack has passed.
Before you start to take it
You must tell your doctor or pharmacist if:
- you have any allergies to any other medicines, including aspirin or other NSAID medicines
- you have or have had any medical conditions, especially the following:
- high blood pressure or fluid retention
- diabetes
- high cholesterol
- heartburn, indigestion, ulcers or other stomach problems
- kidney or liver disease
- asthma or any other breathing problems - you are using an IUD for birth control
- you are pregnant or intend to become pregnant
If it is necessary for you to take MELOXIBINDO, your doctor will discuss the risks and benefits of taking it during pregnancy. - you are taking MELOXIBINDO together with any medicines used to treat high blood pressure and some other heart problems such as ACE inhibitors, angiotensin receptor antagonists and diuretics (also called fluid or water tablets).
When taken together these medicines can cause kidney problems.
If you have not told your doctor or pharmacist about any of the above, tell them before you start taking MELOXIBINDO.
Taking other medicines
Before taking MELOXIBINDO, tell your doctor or pharmacist if you are taking any other medicines, including medicines that you buy without a prescription from a pharmacy, supermarket or health food shop.
There may be interference between MELOXIBINDO and some medicines. These include:
- aspirin, salicylates or other NSAID medicines
- medicines used to thin your blood (such as warfarin, heparin and ticlopidine)
- lithium, a medicine used to treat some types of depression
- antidepressants called selective serotonin reuptake inhibitors (SSRIs)
- methotrexate, a medicine used to treat rheumatoid arthritis (a painful joint disease) and some types of cancer
- cyclosporin, a medicine used to treat rheumatoid arthritis and certain problems with the immune system
- diuretics, also called fluid or water tablets
- medicines used to treat high blood pressure
- medicines used to treat heart problems
- medicines to treat diabetes
- cholestyramine, a medicine used to treat high cholesterol levels in the blood
- corticosteroids (drugs usually used to treat inflammatory conditions, such as skin rash and asthma)
- some medicines used to treat fungal infections
- some sulfur antibiotics
- some medicines used to treat irregular heart beats
- some antihistamines (medicines used to prevent or relieve the symptoms of allergy, such as hay fever or insect stings).
These medicines may be affected by MELOXIBINDO or may affect how well MELOXIBINDO works. Your doctor or pharmacist has more information on medicines to be careful with or avoid while taking MELOXIBINDO.
How to take MELOXIBINDO
Follow all directions given to you by your doctor or pharmacist carefully.
They may differ from the information contained in this leaflet.
How much to take
For the treatment of osteoarthritis
The usual dose of MELOXIBINDO is 7.5 mg, taken as a single dose each day.
However, your doctor will prescribe a dose suitable for your condition.
For the treatment of rheumatoid arthritis
The usual dose of MELOXIBINDO is 15 mg taken as a single dose each day.
Depending on your response, your doctor may reduce this dose to 7.5 mg taken as a single dose each day.
The maximum recommended daily dose of MELOXIBINDO is 15 mg. For patients with kidney problems undergoing dialysis, the maximum recommended daily dose is 7.5 mg.
Ask your doctor for more information if you have been advised to take a different dose.
How to take it
Swallow the tablets with fluid.
It is best to take MELOXIBINDO immediately after food to avoid the chance of an upset stomach.
Try to take MELOXIBINDO at the same time each day, either morning or evening.
How long to take it
Keep taking MELOXIBINDO every day until your doctor tells you to stop.
MELOXIBINDO will not cure your condition but it should help control pain, swelling and stiffness.
If you forget to take it
If it is almost time for your next dose (eg. within 2-3 hours), skip the dose you missed and take the next dose when you are meant to.
Otherwise, take it as soon as you remember, then go back to taking it as you would normally.
Do not try to make up for missed doses by taking more than one dose at a time.
If you are not sure what to do, check with your doctor or pharmacist.
If you have taken too much (overdose)
Immediately telephone your doctor or Poisons Information Centre (telephone 13 11 26) for advice, or go to Accident and Emergency at your nearest hospital if you think that you or anyone else may have taken too much MELOXIBINDO. Do this even if there are no signs of discomfort or poisoning.
Signs of an overdose with MELOXIBINDO may include:
- nausea and/or vomiting
- headache
- drowsiness
- blurred vision
- dizziness
- fits or seizures
- low blood pressure
- difficulty in breathing
- impaired consciousness
- kidney failure.
While you are taking MELOXIBINDO
Things you must do
If you become pregnant while taking MELOXIBINDO, tell your doctor immediately.
If you are about to start any new medicines, tell your doctor and pharmacist that you are taking MELOXIBINDO.
If you are going to have surgery, including dental surgery, tell your doctor or dentist that you are taking MELOXIBINDO.
MELOXIBINDO can slow down blood clotting.
If you get an infection while using MELOXIBINDO, tell your doctor.
MELOXIBINDO may hide some of the signs of an infection (eg. pain, fever, redness and swelling). You may think, mistakenly, that you are better or that the infection is not serious.
Things to be careful of
Be careful driving or operating machinery until you know how MELOXIBINDO affects you.
As with other NSAID medicines, MELOXIBINDO may cause dizziness, drowsiness or blurred vision in some people.
Make sure you know how you react to MELOXIBINDO before you drive a car, operate machinery, or do anything else that could be dangerous if you are not alert.
Side Effects
You should be aware that all medicines carry some risks and that all possible risks may not be known at this stage despite thorough testing.
Check with your doctor as soon as possible if you have any problems while taking MELOXIBINDO, even if you do not think the problems are connected with the medicine or are not listed in this leaflet.
Tell your doctor if you notice any of the following and they worry you:
- stomach upset including nausea, vomiting, heartburn, indigestion, belching, cramps or pain
- headache
- sore mouth or throat, discomfort when swallowing
- constipation, diarrhoea or wind
- dizziness or light-headedness
- skin rash or itching
- skin rashes, which may be caused by exposure to sunlight, can blister and may take on the appearance of a severe burn
- increase in blood pressure
- tinnitus (ringing in the ear).
These side effects are usually mild.
Tell your doctor immediately if you notice any of the following:
- blurred vision
- any change in the amount or colour of your urine (red or brown)
- any pain or difficulty experienced when urinating
- collapse or fainting, shortness of breath or tiredness, fast or irregular heartbeat (also called palpitations), chest pain, swollen or sore leg veins
- severe pain or tenderness in the stomach
- severe dizziness
- yellowing of the skin and eyes (known as jaundice)
- swelling of your ankles, legs or other parts of your body
- signs of anaemia (such as tiredness, being short of breath and looking pale)
- irritation of your mucous membranes (eg. lips, mouth, eyes or genitals).
These are rare but serious side effects. You may need urgent medical attention.
If any of the following happen, STOP taking MELOXIBINDO and tell your doctor immediately or go to Emergency at your nearest hospital:
- vomiting of blood or material that looks like coffee grounds
- bleeding from your back passage (rectum), black sticky motions (stools) or bloody diarrhoea
- swelling of the face, lips or tongue which may make swallowing or breathing difficult
- asthma, wheezing or shortness of breath
- sudden or severe itching, skin rash or hives
- weakness in one part or side of your body, slurred speech, blurred vision or visual disturbances.
These are rare but very serious side effects. You may need urgent medical attention or hospitalisation.
Not all of these side effects have been reported with MELOXIBINDO but have been seen with similar medicines.
Other side effects not listed above may occur in some people.
Tell your doctor if you notice anything else that is making you feel unwell.
Do not be alarmed by this list of possible side effects. You may not experience any of them.
After taking MELOXIBINDO
Storage
Keep your tablets in their pack until it is time to take them.
If you take them out of their packaging, they will not keep well.
Keep MELOXIBINDO in a cool dry place where the temperature stays below 25 degrees C and protected from light.
MELOXIBINDO should not be stored in direct sunlight or heat.
Keep your tablets where children cannot reach them.
A locked cupboard at least one-and-one-half metres above the ground is a good place to store medicines.
Disposal
Your pharmacist or doctor should be able to safely dispose of any unused MELOXIBINDO.
Product Description
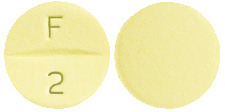
What MELOXIBINDO looks like
MELOXIBINDO (7.5 & 15 mg meloxicam) is presented in pack sizes of 30’s & 60’s in blister.
- MELOXIBINDO 7.5
Light yellow, round, uncoated tablet with score line between ‘F’ and ‘1’ debossed on one side and plain on the other side. - MELOXIBINDO 15
Light yellow, round, uncoated tablet with score line between ‘F’ and ‘2’ debossed on one side and plain on the other side.
Ingredients
Active Ingredient:
Meloxicam.
Each tablet may contain either 7.5 mg or 15 mg of Meloxicam.
Other Ingredients:
- sodium citrate
- lactose
- microcrystalline cellulose
- povidone
- crospovidone
- colloidal anhydrous silica
- magnesium stearate.
Name and Address of the Sponsor
Aurobindo Pharma Australia Pty Ltd
Unit 3 North Rydelink
277-283 Lane Cove Road
Macquarie Park NSW 2113
Australia
Date of Approval:
31 July 2012



 The data from both studies indicate that meloxicam is effective and safe for the treatment of patients with rheumatoid arthritis.
The data from both studies indicate that meloxicam is effective and safe for the treatment of patients with rheumatoid arthritis. As with other NSAIDs, caution should be exercised when treating patients with a history of upper gastrointestinal disease and in patients receiving treatment with anticoagulants. Patients with GI symptoms should be monitored. Meloxicam therapy should cease if peptic ulceration or GI bleeding occurs. The consequences of such events are generally more serious in the elderly.
As with other NSAIDs, caution should be exercised when treating patients with a history of upper gastrointestinal disease and in patients receiving treatment with anticoagulants. Patients with GI symptoms should be monitored. Meloxicam therapy should cease if peptic ulceration or GI bleeding occurs. The consequences of such events are generally more serious in the elderly. Adverse events that occurred in ≥ 1% of the MOBIC treatment groups in two 12-week placebo controlled rheumatoid arthritis trials are presented in Table 4.
Adverse events that occurred in ≥ 1% of the MOBIC treatment groups in two 12-week placebo controlled rheumatoid arthritis trials are presented in Table 4. Higher doses of meloxicam (22.5 mg and greater) have been associated with an increased risk of serious GI events, therefore the daily dose of meloxicam should not exceed 15 mg.
Higher doses of meloxicam (22.5 mg and greater) have been associated with an increased risk of serious GI events, therefore the daily dose of meloxicam should not exceed 15 mg.