What is in this leaflet
This leaflet answers some common questions about MYLERAN tablets. It does not contain all of the available information. It does not take the place of talking to your doctor or pharmacist.
All medicines have risks and benefits. Your doctor has weighed the risks of you taking MYLERAN tablets against the benefits this medicine is expected to have for you.
If you have any concerns about taking this medicine, ask your doctor.
Keep this leaflet with the medicine. You may need to read it again.
What MYLERAN is used for
MYLERAN contains busulfan as the active ingredient. It belongs to a group of medicines called cytotoxics.
MYLERAN is used to treat certain blood disorders.
It works by reducing the amount of certain types of blood cells in your body.
Ask your doctor if you have any questions about why MYLERAN has been prescribed for you. Your doctor may have prescribed it for another purpose.
This medicine is only available with a doctor’s prescription.
There is no evidence that it is addictive.
Before you take it
When you must not take it
Do not take MYLERAN if you have ever had an allergic reaction to:
- busulphan
- any of the tablet ingredients listed at the end of this leaflet.
Symptoms of an allergic reaction may include shortness of breath, wheezing or difficulty in breathing; swelling of the face, lips, tongue or any other parts of the body; rash, itching or hives on the skin.
Do not take MYLERAN if you are planning to become pregnant or father a child unless you and your doctor have discussed the risks and benefits involved. MYLERAN may harm eggs and sperm and may cause sterility in both men and women. Reliable contraceptive methods must be taken to avoid pregnancy whilst you or your partner is taking this medicine.
Do not take MYLERAN if you are pregnant unless you and your doctor have discussed the risks and benefits involved. It may affect your developing baby if you take it during pregnancy.
Do not take this medicine whilst breast feeding.
Do not take it after the expiry date (EXP) printed on the pack. If you take it after the expiry date has passed, it may not work as well.
Do not take MYLERAN if the bottle shows signs of tampering.
Before you start to take it
Tell your doctor if you are allergic to any other medicines or any other foods, dyes or preservatives.
Tell your doctor if you have or have had any of the following conditions:
- you have recently received or are receiving radiotherapy or chemotherapy
- you have recently been vaccinated or are planning to be vaccinated
- kidney, lung or liver disease
- gout.
If you have not told your doctor about any of the above, tell them before you start taking MYLERAN.
Taking other medicines
Tell your doctor if you are taking any other medicines, including any that you buy without a prescription from a pharmacy, supermarket or health food shop.
Some medicines may be affected by MYLERAN or may affect how well it works. You may need to take different amounts of your medicine or you may need to take different medicines. These include:
- phenytoin
- itraconazole or metronidazole
- thioguanine
- other cytotoxic drugs
- vaccinations with ‘live’ organism vaccines.
Your doctor or pharmacist has more information on medicines to be careful with or avoid while taking this medicine.
How to take it
How much to take
Take MYLERAN tablets exactly as directed by your doctor. Your doctor will decide what dose and for how long you will be taking MYLERAN. This depends on factors such as your weight, any pre-existing conditions and your response to the treatment. Your doctor may change the dose and frequency of your medicine as your condition changes.
Your doctor may order regular blood tests while you are taking MYLERAN in order to monitor your blood cell count and to change your dose if necessary.
How to take it
Swallow each tablet whole with water.
Do not break, crush or chew the tablets.
If you forget to take it
Tell your doctor if you forget to take a dose.
Do not take a double dose to make up for the dose that you missed.
If you take too much (overdose)
Immediately telephone your doctor or the Poisons Information Centre (telephone 131126) for advice, or go to Accident and Emergency at your nearest hospital if you think that you or anyone else may have taken too much MYLERAN. Do this even if there are no signs of discomfort or poisoning. You may need urgent medical attention.
While you are taking it
Things you must do
Tell your doctor if, for any reason, you have not taken your medicine exactly as prescribed. Otherwise your doctor may think that it was not effective and change your treatment unnecessarily.
It is important that you visit your doctor regularly, so your doctor can check your progress and make sure your medicine is working.
Tell any other specialist, doctor, dentist or pharmacist that you are taking MYLERAN, especially if you are about to be started on any new medicines, immunisations, vaccinations or radiotherapy.
If you are about to undergo surgery or an operation, tell your doctor that you are taking MYLERAN tablets.
Tell your doctor if you become pregnant, are trying to become pregnant or trying to father a child.
Things you must not do
Do not stop taking MYLERAN or change the dose without first checking with your doctor.
Do not give this medicine to anyone else, even if their symptoms seem similar to yours.
Do not use MYLERAN to treat any other complaints unless your doctor says to.
Things to be careful of
Do not break, crush or chew the tablet. Provided the outer coating of the tablet is intact, there is no risk in handling MYLERAN tablets.
Be careful driving or operating machinery until you know how MYLERAN affects you.
Do not have any vaccinations without your doctor’s approval.
Side effects
Tell your doctor as soon as possible if you do not feel well while you are taking MYLERAN.
All medicines can cause some side effects. Sometimes they are serious, most of the time they are not. You may need medical treatment if you get some of the side effects.
The following side effects have been reported with MYLERAN:
- production of bone marrow cells may be reduced. You may notice an increase in infections. Your doctor will do regular blood tests, but you should tell him at once if you notice any signs of fever or infection or any unexpected bruising, bleeding or signs of blood in your urine
- in women, ovarian failure, periods may stop
- in men, sperm production may be reduced or stop. The testes may reduce in size and may not function.
- in girls, the onset of puberty may be delayed or stop.
Tell your doctor if you notice any of the following side effects:
- nausea and vomiting
- diarrhoea
- darker areas of skin
- weight loss
- jaundice, a yellowing of the whites of the eyes or the skin
- pain in the liver
- gaining weight quickly
- swelling of arms, legs and stomach
- unusual tiredness, looking pale, feeling weaker or dizzy
- skin rash or itching
- hair loss
- frequent infections such as fever, sore throat or mouth ulcers
- bruisingorbleedingmore easily than normal, nose bleeds
- blood in the urine
- convulsions
- persistentcoughor breathlessness
- muscle weakness
- problems with your eyesight
- in men, breast enlargement.
Tell your doctor immediately if you notice any of the following allergic-type symptoms:
- wheezing
- swelling of the lips/mouth
- difficulty in breathing
- hay fever
- lumpy rash ("hives")
- fainting
Tell your doctor if you notice anything else that is making you feel unwell, even if you think the problems are not connected with this medicine and are not referred to in this leaflet. Other side effects not listed above may occur in some people.
Do not be alarmed by this list of possible side effects. You may not experience any of them.
After taking it
Things to be aware of
Because of the way this medicine works there is a chance it might cause other unwanted effects that may not occur until months or years after the medicine is used. These delayed effects may include certain types of cancer such as leukaemia.
Discuss these possible effects with your doctor.
Storage
Keep MYLERAN tablets in a cool, dry place where it stays below 25°C.
Keep your tablets in the bottle until it is time to take them. If you take the medicine out of the bottle it may not keep as well.
Do not leave it in the car, on window sills, near a sink or in the bathroom. Heat and dampness can destroy some medicines.
Keep this medicine where young children cannot reach it. A locked cupboard at least one-and-a half metres above the ground is a good place to store medicines.
Product description
What it looks like
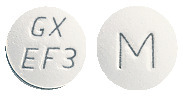
MYLERAN tablets are white, film-coated, round and biconvex. They are engraved “GX EF3”on one side and “M” on the other.
Available in bottles of 100 tablets.
Ingredients
Active ingredient:
Each tablet contains 2 mg busulfan.
Inactive ingredients:
- lactose anhydrous
- starch – pregelatinised maize
- magnesium stearate
- hypromellose
- titanium dioxide
- glycerol triacetate.
Sponsor
Aspen Pharmacare Australia Pty Ltd
34-36 Chandos Street
St Leonards NSW 2065
Australian Registration Number: AUST R 68028
This leaflet was revised in July 2017
Published by MIMS October 2017