What is in this leaflet
This leaflet answers some common questions about Nesina.
It does not contain all the available information. It does not take the place of talking to your doctor, pharmacist or diabetes educator.
The information in this leaflet was last updated on the date listed on the final page. More recent information on the medicine may be available. You should ensure that you speak to your pharmacist or doctor to obtain the most up to date information on this medicine. You can also download the most up to date leaflet from https://takeda.com/en-au/what-we-do/our-products/.
Those updates may contain important information about the medicine and its use of which you should be aware.
All medicines have risks and benefits. Your doctor has weighed the risks of you taking this medicine against the benefits they expect it will have for you.
If you have any concerns about taking this medicine, ask your doctor or pharmacist.
Keep this leaflet with the medicine. You may need to read it again.
What Nesina is used for
Nesina is used to lower blood sugar levels in adults with type 2 diabetes mellitus.
It must be taken together with other antidiabetic medicines, which your doctor will have prescribed for you, such as sulfonylureas (e.g. glipizide, glimepiride, glibenclamide), metformin and/or thiazolidinediones (e.g. pioglitazone) or insulin with or without metformin.
Nesina is used when your blood sugar cannot be adequately controlled by diet, exercise and one or more of these other antidiabetic medicines.
It is important that you continue to take your other antidiabetic medication and continue to follow the advice on diet and exercise that your doctor or diabetes educator has given you.
Type 2 Diabetes mellitus
Type 2 diabetes is also called non-insulin-dependent diabetes mellitus (NIDDM).
Type 2 diabetes develops if the body does not make enough insulin, or if the insulin that your body makes does not work as well as it should. It can also develop if the body produces too much glucagon.
Insulin is a hormone which helps lower the level of sugar in your blood, especially after meals. Glucagon is another hormone which triggers the production of sugar by the liver, causing the blood sugar to rise. The pancreas makes both of these hormones.
If your blood glucose is not properly controlled, you may experience hypoglycaemia (low blood glucose) or hyperglycaemia (high blood glucose). High blood glucose can lead to serious problems with your heart, eyes, circulation and/or kidneys.
The main goal of treating diabetes is to lower your blood sugar to a level deemed appropriate by your doctor. Lowering and controlling blood sugar may help prevent or delay complications of diabetes.
How Nesina works
Nesina contains the active ingredient alogliptin, which is a member of a class of medicines you take by mouth called DPP-4 inhibitors (dipeptidyl peptidase-4 inhibitors), that lowers blood sugar levels in patients with type 2 diabetes mellitus.
- Nesina lowers blood sugar when blood sugar is high, especially after a meal.
- Nesina helps improve the levels of insulin produced by your own body after a meal.
- Nesina decreases the amount of blood sugar made by the body.
- Nesina by itself is unlikely to cause low blood sugar (hypoglycaemia) because it does not work when blood sugar is low.
Ask your doctor or pharmacist if you have any questions about why it has been prescribed for you.
This medicine is only available with a doctor’s prescription.
This medicine is not addictive.
Before you take it
When you must not take it
Do not take Nesina if you are allergic to alogliptin (the active ingredient in Nesina) or any of the ingredients listed at the end of this leaflet. Some symptoms of an allergic reaction include skin rash, itching, shortness of breath or swelling of the face, lips or tongue, which may cause difficulty in swallowing or breathing.
Do not give Nesina to a child or adolescent. Nesina is not recommended for children and adolescents under 18 years due to the lack of data in these patients.
Do not take it after the expiry date printed on the pack. The expiry date refers to the last day of that month. If you take it after the expiry date has passed, it may not work as well.
Do not take it if the packaging is torn or shows signs of tampering.
Before you start to take it
Tell your doctor if you have allergies to any other medicines or any other substances, such as foods, preservatives or dyes. Your doctor will want to know if you are prone to allergies.
Tell your doctor if you are pregnant or intend to become pregnant. Like most medicines of this kind, Nesina is not recommended to be used during pregnancy. Your doctor will discuss the risks and benefits of taking it if you are pregnant.
Tell your doctor if you are breastfeeding or planning to breastfeed. It is not known whether Nesina passes into breast milk. Your doctor will discuss the risks and benefits of taking it if you are breastfeeding or planning to breastfeed.
Tell your doctor if you are taking an antidiabetic medicine known as sulphonylurea (e.g. glipizide, glimepiride, glibenclamide) or insulin. Your doctor may want to reduce your dose of sulphonylurea or insulin when you take any of them together with Nesina in order to avoid too low blood sugar (hypoglycaemia).
Tell your doctor if you have or have had any medical conditions, especially the following:
- problems with your kidneys
If you have kidney problems, your doctor may prescribe lower doses. Your doctor might test your kidney function before you start treatment with Nesina and periodically during treatment. - heart failure
There is limited experience with alogliptin in patients with heart failure. - liver disease
- disease of the pancreas
- type 1 diabetes, also called insulin-dependent diabetes mellitus (IDDM) or juvenile onset diabetes, where the body does not produce enough insulin
- diabetic ketoacidosis, a complication of diabetes where chemicals called ketones build up in the body due to very low insulin levels
Nesina should not be used in patients with type 1 diabetes mellitus or for the treatment of diabetic ketoacidosis.
If you are not sure whether any of the above conditions apply to you, your doctor can advise you.
If you have not told your doctor about any of the above, tell him/her before you take Nesina.
Taking other medicines
Tell your doctor or pharmacist if you are taking any other medicines, including any that you buy without a prescription from your pharmacy, supermarket or health food store.
Nesina can be taken with most other medicines.
How to take it
Follow all directions given to you by your doctor and pharmacist carefully. They may differ from the information contained in this leaflet. If you do not understand the instructions on the label, ask your doctor or pharmacist for help.
How much to take
The usual dose for this medicine is one 25 mg tablet once a day.
If you have kidney problems your doctor may prescribe lower doses. This may be 12.5 mg or 6.25 mg once a day, depending on the severity of your kidney disease.
Ask your doctor or pharmacist if you are unsure of the correct dose for you.
Your doctor will prescribe Nesina in combination with other antidiabetic medicine, if that medicine alone is not sufficient to control your blood sugar level.
How to take it
Swallow the tablet whole with a glass of water.
When to take it
You can take Nesina with or without food.
Take Nesina at about the same time each day. Taking it at the same time each day will have the best effect. It will also help you remember when to take it.
If you are not sure when to take it, ask your doctor or pharmacist.
How long to take it
Continue taking your medicine for as long as your doctor tells you to. It is important to keep taking your medicine even if you feel well.
Your doctor will check your progress and monitor your blood sugar levels to make sure the medicine is working and will discuss with you how long your treatment should continue for.
Diet and exercise can help your body use its blood sugar better. It is important to stay on your doctor’s or diabetic educator’s recommended diet, exercise and weight loss program while taking Nesina.
Ask your doctor or pharmacist if you are not sure how long to take the medicine for.
If you forget to take it
If you forget to take a dose, take it as soon as you remember it, and then go back to taking it as you would normally.
Do not take a double dose (two doses at the same time) to make up for the dose that you missed. This may increase the chance of getting an unwanted side effect.
If it is almost time for your next dose, skip the dose you missed and take your next dose when you are meant to.
If you are not sure what to do, ask your doctor or pharmacist.
If you have trouble remembering when to take your medicine, ask your pharmacist for some hints.
If you take too much (overdose)
Immediately telephone your doctor or the Poisons Information Centre (telephone 13 11 26), or go to Accident and Emergency at your nearest hospital, if you think you or anyone else may have taken too much Nesina. Take this leaflet or some tablets with you so that your doctor knows exactly what you have taken.
Do this even if there are no signs of discomfort or poisoning. You may need urgent medical attention.
While you are taking it
Things you must do
If you become pregnant while you are taking this medicine, tell your doctor immediately. Like most medicines of this kind, Nesina is not recommended to be used during pregnancy. Your doctor will discuss the risks and benefits of taking it if you are pregnant.
Tell all the doctors, dentists and pharmacists who are treating you that you are taking Nesina.
If you are about to be started on any new medicine, tell your doctor and pharmacist that you are taking Nesina.
Carefully follow your doctor's and/or dietician's advice on diet, drinking alcohol and exercise.
Keep all of your doctor's appointments so that your progress can be checked. Your doctor will do regular checks to help prevent you from having side effects from the medicine or developing serious complications of diabetes.
Make sure you check your blood glucose levels regularly. This is the best way to tell if your diabetes is being controlled properly. Your doctor or diabetes educator will show you how and when to do this.
If you become ill or experience extra stress, injury, fever, infection or need surgery, tell your doctor. Your blood glucose may become difficult to control at these times.
Make sure you keep enough medicine to last over weekends and holidays. It is important to keep your blood glucose controlled at all times to prevent serious complications of diabetes from happening.
Things you must not do
Do not take more than the recommended dose unless your doctor or pharmacist tells you to.
Do not give this medicine to anyone else, even if they have the same condition as you.
Do not use this medicine to treat any other complaints unless your doctor tells you to.
Do not stop taking Nesina without checking with your doctor.
Do not skip meals while taking Nesina.
Things to be careful of
Be careful driving, operating machinery or doing jobs that require you to be alert until you know how this medicine affects you.
If your blood glucose level becomes too low, you may feel dizzy, lightheaded, weak or tired and your reaction time may be slower than usual.
If you have any of these symptoms, do not drive or do anything else that could be dangerous.
Be careful when doing any of the following things, which increase the risk of your blood glucose becoming too low:
- drinking alcohol
- not eating enough
- doing unexpected or vigorous exercise
Side effects
All medicines have some unwanted side effects. Sometimes they are serious, but most of the time they are not. Your doctor has weighed the risks of using this medicine against the benefits they expect it will have for you.
Do not be alarmed by this list of possible side effects. You may not experience any of them.
Tell your doctor or pharmacist as soon as possible if you do not feel well while you are taking Nesina.
Tell your doctor or pharmacist if you notice any of the following and they worry you:
- headache
- cold-like symptoms such as stuffy or runny nose, sore throat, feeling tired
- stomach pain
- indigestion, heartburn
- rash
- itchy skin
- joint pain
Tell your doctor immediately if you notice any of the following:
- blisters or the breakdown of the outer layer of your skin (erosion).
Some people who take medicines called DPP-4 inhibitors, like Nesina, may develop a skin reaction called bullous pemphigoid, that may require treatment in a hospital. Your doctor may tell you to stop taking Nesina.
If any of the following happen, stop taking this medicine and tell your doctor immediately, or go to Accident and Emergency at your nearest hospital:
- Symptoms of allergic reaction.
The symptoms may include: a rash, hives, swallowing or breathing problems, swelling of your lips, face, throat or tongue and feeling faint. - A severe allergic reaction including general itching and feeling of heat, especially affecting the scalp, mouth, throat, palms of hands or soles of feet (Stevens-Johnson syndrome).
This severe allergic reaction has been reported in a very small number of patients. - Severe and persistent pain around the top of your stomach which might reach into your back, often with nausea and vomiting.
This could be a sign of an inflamed pancreas (pancreatitis). - Yellowing of your skin or the whites of your eyes, nausea, loss of appetite, unusual or unexplained tiredness, dark urine
These could be signs of liver problems. - Symptoms of low blood sugar (hypoglycaemia): trembling, sweating, anxiety, blurred vision, tingling lips, paleness, mood change or feeling confused.
Hypoglycaemia may occur when Nesina is taken in combination with insulin or sulphonylureas (e.g. glipizide, glimepiride, glibenclamide). Your blood sugar could fall below the normal level and can be increased by taking sugar. Your doctor, pharmacist or diabetes educator may have recommended that you carry some glucose tablets, sugar lumps, sweets, biscuits or sugary fruit juice.
These may be serious side effects of Nesina. You may need urgent medical attention.
Tell your doctor or pharmacist if you notice anything else that is making you feel unwell. Other side effects not listed above may occur in some consumers.
Ask your doctor or pharmacist to answer any questions you may have.
After taking it
Storage
Keep your tablets in the blister pack until it is time to take them.
Keep the medicine in a cool, dry place where the temperature stays below 25°C.
Do not store it or any other medicine in the bathroom, near a sink, or on a windowsill.
Do not leave it in the car. Heat and damp can destroy some medicines.
Keep it where children cannot reach it. A locked cupboard at least one-and-a-half metres above the ground is a good place to store medicines.
Disposal
If your doctor tells you to stop taking Nesina, or the medicine has passed its expiry date, ask your pharmacist what to do with any tablets left over.
Product description
What it looks like
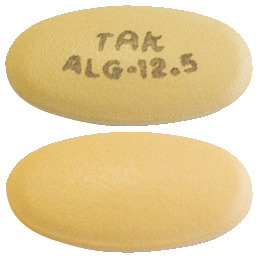
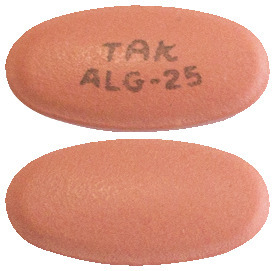
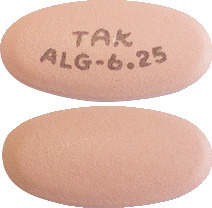
Nesina comes in three strengths of tablets:
Nesina 25 mg film-coated tablets are light red, oval, biconvex, film-coated tablets, with “TAK" and "ALG-25” printed in grey ink on one side.
Nesina 12.5 mg film-coated tablets are yellow, oval, biconvex, film-coated tablets, with “TAK" and "ALG-12.5” printed in grey ink on one side.
Nesina 6.25 mg film-coated tablets are light pink, oval, biconvex, film-coated tablets, with “TAK" and "ALG-6.25” printed in grey ink on one side.
Nesina is available in blister packs of 7 (sample) and 28 tablets.
Ingredients
The active substance in Nesina is alogliptin.
Active Ingredient:
Each tablet contains alogliptin benzoate equivalent to 25 mg, 12.5 mg, or 6.25 mg alogliptin.
Inactive Ingredients:
- mannitol
- microcrystalline cellulose
- hyprolose
- croscarmellose sodium
- magnesium stearate
- hypromellose
- titanium dioxide (E171)
- iron oxide red (CI77491) (present in 25 mg and 6.25 mg tablets)
- iron oxide yellow (CI77492) (present in 12.5 mg tablets)
- macrogol
- edible ink gray F1 (printing ink)
Nesina does not contain gluten, sucrose or lactose.
Sponsor
Takeda Pharmaceuticals Australia Pty Ltd
Level 39
225 George Street
Sydney NSW 2000 Australia
Tel: 1800 012 612
www.takeda.com/en-au
This leaflet was prepared in September 2021.
Australian Registration Numbers
25 mg tablets: AUST R 199539
12.5 mg tablets: AUST R 199543
6.25 mg tablets: AUST R 199541
NESINA®, TAKEDA® and the TAKEDA Logo® are registered trademarks of Takeda Pharmaceutical Company Limited.
Published by MIMS November 2021




 There were 703 patients who experienced an event within the secondary MACE composite endpoint (first event of cardiovascular death, nonfatal myocardial infarction, nonfatal stroke and urgent revascularization due to unstable angina). In the alogliptin group, 12.7% (344 subjects) experienced an event within the secondary MACE composite endpoint, compared with 13.4% (359 subjects) in the placebo group [hazard ratio = 0.95; 1 sided 99% confidence interval: 0-1.14].
There were 703 patients who experienced an event within the secondary MACE composite endpoint (first event of cardiovascular death, nonfatal myocardial infarction, nonfatal stroke and urgent revascularization due to unstable angina). In the alogliptin group, 12.7% (344 subjects) experienced an event within the secondary MACE composite endpoint, compared with 13.4% (359 subjects) in the placebo group [hazard ratio = 0.95; 1 sided 99% confidence interval: 0-1.14]. Molecular formula: C18H21N5O2.C7H6O2.
Molecular formula: C18H21N5O2.C7H6O2.