What is in this leaflet
This leaflet answers some common questions about NIDEM.
It does not contain all of the available information. It does not take the place of talking to your doctor, pharmacist or diabetes educator.
All medicines have benefits and risks. Your doctor has weighed the risks of you taking NIDEM against the benefits they expect it will have for you.
Talk to your doctor, pharmacist or diabetes educator if you have any concerns about taking this medicine.
Keep this leaflet with your medicine. You may need to read it again.
What NIDEM is used for
NIDEM is used to control blood glucose in people with Type 2 diabetes mellitus. This type of diabetes is also called non-insulin dependent diabetes mellitus (NIDDM) or maturity onset diabetes.
NIDEM is used when diet and exercise are not enough to control your blood glucose levels. It can be used alone, or in combination with other medicines for treating diabetes.
NIDEM is available only with a doctor's prescription.
How NIDEM works
NIDEM belongs to a group of medicines called sulphonylureas. These medicines lower blood glucose by increasing the amount of insulin produced by your pancreas.
If your blood glucose is not properly controlled, you may experience hypoglycaemia (low blood glucose) or hyperglycaemia (high blood glucose).
Hypoglycaemia
Hypoglycaemia (low blood glucose) can occur suddenly. Signs may include:
- weakness, trembling or shaking
- sweating
- lightheadedness, dizziness, headache or lack of concentration
- irritability, tearfulness or crying
- hunger
- numbness around the lips and tongue.
If not treated promptly, these may progress to:
- loss of co-ordination
- slurred speech
- confusion
- fits or loss of consciousness
Hyperglycaemia
Hyperglycaemia (high blood glucose) usually occurs more slowly than hypoglycaemia. Signs of hyperglycaemia may include:
- lethargy or tiredness
- headache
- thirst
- passing large amounts or urine
- blurred vision
Long-term hyperglycaemia can lead to serious health problems such as heart disease, blindness, poor blood circulation, gangrene, and kidney damage.
Before you take NIDEM
When you must not take it
Do not take this medicine if you are allergic to:
- medicines containing gliclazide or any other sulphonylurea
- sulfonamide (sulfur) antibiotics
- certain types of fluid tablets (thiazide diuretics)
- any of the ingredients listed at the end of this leaflet.
Do not take it if you have any of the following medical conditions:
- type 1 diabetes mellitus that is well controlled by insulin alone
- unstable diabetes that is not well controlled
- diabetic acidosis
- diabetic coma
- severe kidney disease
- you are taking an antibiotic medicine containing the active ingredient miconazole
- severe liver disease.
Do not take it if you are pregnant or plan to become pregnant. Insulin is more suitable for controlling blood glucose during pregnancy. Your doctor will replace NIDEM with insulin while you are pregnant.
Do not take it if you are breastfeeding. This medicine can pass into breast milk and may harm your baby.
Do not take it if the expiry date (Exp.) printed on the pack has passed.
Do not take it if the packaging shows signs of tampering or the tablets do not look quite right.
If you are not sure whether you should start taking NIDEM, ask your doctor.
Before you start to take it
Tell your doctor if you are allergic to any other medicines, foods, dyes or preservatives.
Tell your doctor if you have any medical conditions, especially the following:
- liver problems
- kidney problems
- a history of diabetic coma
- heart failure
- adrenal, pituitary or thyroid problems.
- If you have a family history of or know you have the hereditary condition glucose-6- phosphate dehydrogenase (G6PD) deficiency (abnormality of red blood cells), lowering of the haemoglobin level and breakdown of red blood cells (haemolytic anaemia) can occur.
- you have any medical condition, or do anything, that may increase the risk of hyperglycaemia - for example
Tell your doctor if you
- drink alcohol in any amount
- do not eat regular meals
- do a lot of exercise
- are ill or feeling unwell.
- you are pregnant or plan to become pregnant or are breast- feeding.
Your doctor can discuss with you the risks and benefits involved.
Alcohol, diet, exercise and your general health all strongly affect the control of your diabetes.
Discuss these with your doctor.
If you have not told your doctor about any of the above, tell them before you start taking NIDEM.
Taking other medicines
Tell your doctor if you are taking any other medicines, including any that you buy without a prescription from a pharmacy, supermarket or health food shop.
Some medicines may be affected by NIDEM or may affect how well it works. These include:
- other medicines used to treat diabetes (such as biguanides and insulin)
- some medicines used to treat fungal or yeast infections (miconazole which is contraindicated)
- alcohol
- medicines used to treat high blood pressure and some heart conditions
- monoamine oxidase inhibitors (MAOIs), medicines used to treat depression
- clofibrate, a medicine used to reduce high blood fat levels
- medicines used to prevent blood clots
- diuretics, also called fluid tablets
- some antibiotics
- cimetidine, a medicine used to treat reflux and ulcers
- corticosteroids such as prednisone, cortisone
- some medicines used to relieve pain, swelling and other symptoms of inflammation, including arthritis
- oestrogens such as in oral contraceptives or hormone replacement therapy
- barbiturates, medicines used to treat epilepsy.
Some medicines may lead to high blood glucose levels (hyperglycaemia) by weakening the blood glucose-lowering effect of Nidem
These include:
- alcohol
- some medicines for epilepsy (danazol)
- some medicines used to treat depression and other mental illness (chlorpromazine)
- some hormones used in hormone replacement therapy and oral contraceptives (oestrogen, progesterone)
- St John's Wort (Hypericum perforatum) preparations used to treat depression
- some medicines for asthma (salbutamol, intravenous terbutaline).
- barbiturates, medicines used for sedation
- glucocorticoids
Some medicines may lead to unstable blood glucose (low blood sugar and high blood sugar) when taken at the same time as NIDEM, especially in elderly patients.
These include:
- A class of antibiotics called fluoroquinolones.
NIDEM may change the effects of some other medicines.
These include:
- some medicines used to prevent blood clots (warfarin)
You may need different amounts of your medicine or you may need to take different medicines. Your doctor, pharmacist or diabetes educator can tell you what to do if you are taking any of these medicines. They also have a more complete list of medicines to be careful with or avoid while taking NIDEM.
Your doctor or pharmacist can tell you what to do if you are taking any of these medicines. They also have more information on medicines to be careful with or avoid while taking NIDEM.
Check with your doctor or pharmacist if you are not sure whether you are taking any of these medicines.
How to take it
How much to take
The dose varies from patient to patient. Your doctor will decide the right dose for you.
The usual starting dose for adults is half an 80 mg tablet each day.Your doctor may increase this dose up to four tablets a day, depending on your blood glucose levels.
How to take NIDEM
Swallow the tablets with a glass of water.
This medicine can be taken before, during or after food.
If you forget to take it
If it is almost time for your next dose, skip the dose you missed and take your next dose when you are meant to.
Otherwise, take the missed dose as soon as you remember (with food), and then go back to taking your tablets as you would normally.
Do not take a double dose to make up for the dose you missed.
If you are not sure what to do, ask your doctor or pharmacist.
How long to take it for
Keep taking NIDEM for as long as your doctor recommends.
This medicine will help control diabetes but will not cure it. Most people will need to take NIDEM for long periods of time.
If you take too much (overdose)
Immediately telephone your doctor, or the Poisons Information Centre (telephone 13 11 26), or go to Accident and Emergency at the nearest hospital, if you think you or anyone else may have taken too much NIDEM. Do this even if there are no signs of discomfort or poisoning.
If you take too much medicine, you may experience symptoms of hypoglycaemia (low blood glucose).
If you do experience any signs of hypoglycaemia, raise your blood glucose quickly by eating jelly beans, sugar or honey, drinking non-diet soft drink or taking glucose tablets.
While you are taking it
Things you must do
Before starting any new medicine, tell your doctor or pharmacist that you are taking NIDEM.
Tell all the doctors, dentists and pharmacists who are treating you that you are taking NIDEM.
If you become pregnant while taking this medicine, tell your doctor immediately.
Make sure that you, your friends, family and work colleagues can recognise the symptoms of hypoglycaemia and hyperglycaemia and know how to treat them.
Hypoglycaemia
If you experience any of the symptoms of hypoglycaemia, you need to raise your blood glucose immediately. You can do this by doing one of the following:
- eating 5-7 jelly beans
- eating 3 teaspoons of sugar or honey
- drinking half a can of non-diet soft drink
- taking 2-3 concentrated glucose tablets.
Unless you are within 10 to 15 minutes of your next meal or snack, follow up with extra carbohydrates such as plain biscuits, fruit or milk. Taking this extra carbohydrate will prevent a second drop in your blood glucose level.
Hyperglycaemia
If you experience any of the symptoms of hyperglycaemia, contact your doctor immediately.
The risk of hyperglycaemia is increased in the following situations:
- uncontrolled diabetes
- illness, infection or stress
- taking less NIDEM than prescribed
- taking certain other medicines
- too little exercise
- eating more carbohydrates than normal.
Tell your doctor if any of the following happen:
- you become ill
- you are injured
- you have a fever
- you have a serious infection
- you are having surgery.
Your blood glucose may become difficult to control at these times.Your doctor may decide to replace NIDEM with insulin.
Visit your doctor regularly for check-ups. Your doctor may want to check your kidneys, liver, heart and blood while you are taking this medicine.
Make sure you check your blood glucose levels regularly. This is the best way to tell if your diabetes is being controlled properly. Your doctor or diabetes educator will show you how and when to do this.
Carefully follow your doctor's and dietician’s advice on diet, drinking alcohol and exercise. If you drink alcohol while taking this medicine, you may get flushing, headache, breathing difficulties, rapid heartbeat, stomach pains or feel sick and vomit. The combination of alcohol and NIDEM also increases the risk of hypoglycaemia occurring.
Tell your doctor immediately if you notice the return of any symptoms of hyperglycaemia you have experienced before starting NIDEM. These may include lethargy or tiredness, headache, thirst, passing large amounts of urine and blurred vision. These may be signs that this medicine is no longer working, even though you may have been taking it successfully for some time.
Things you must not do
Do not skip meals while taking NIDEM.
Do not stop taking it or change the dose without checking with your doctor.
Do not give it to anyone else, even if they have the same condition as you.
Things to be careful of
Be careful driving or operating machinery until you know how this medicine affects you. NIDEM may cause dizziness in some people. Drinking alcohol can make this worse. If either of these occur, do not drive, operate machinery or do anything else that could be dangerous.
If you drink alcohol while taking NIDEM, you may get flushing, headache, breathing difficulties, rapid heart beat, stomach pains or feel sick and vomit.
Be careful not to let your blood glucose levels fall too low. Low blood glucose levels may slow your reaction time and affect your ability to drive or operate machinery.
If you become sick with a cold, fever or flu, it is very important to continue taking NIDEM and eating your normal meals. If you have trouble eating solid food, use sugar-sweetened drinks as a carbohydrate substitute or eat small amounts of bland food. Your diabetes educator or dietician can give you a list of foods to eat on sick days.
When you are travelling, it is a good idea to:
- wear some form of identification (e.g. bracelet) showing you have diabetes
- carry some form of sugar to treat hypoglycaemia if it occurs, for example, sugar sachets or jelly beans
- carry emergency food rations in case of a delay, for example, dried fruit, biscuits or muesli bars
- bring enough NIDEM with you, so you don't miss any doses.
Protect your skin when you are in the sun, especially between 10am and 3pm. Sulphonylureas (the group of medicines that NIDEM belongs to) may cause your skin to be more sensitive to sunlight than it is normally. Exposure to sunlight may cause a skin rash, itching, redness, or a severe sunburn.
If outdoors, wear protective clothing and use a 30+ sunscreen. If your skin does appear to be burning, tell your doctor immediately.
Side effects
Tell your doctor or pharmacist as soon as possible if you do not feel well while you are taking NIDEM.
NIDEM helps most people with diabetes but it may have unwanted side effects in some people.
All medicines can have side effects. Sometimes they are serious, most of the time they are not. You may need medical treatment if you get some of the side effects.
NIDEM helps most people with Type 2 diabetes, but it may sometimes have unwanted side effects. These can include:
- hyPOglycaemia and hyPERglycaemia. A section at the end of this leaflet contains advice about recognising and treating hyPOglycaemia and hyPERglycaemia
- runny or blocked nose, sneezing, facial pressure or pain, bronchitis, sore throat and discomfort when swallowing, upper respiratory infection, coughing
- back pain, arthralgia, arthrosis,
- high blood pressure, chest pain,
- Headache, unusual weakness,
- Viral infection, urinary tract infection,
- dizziness
- decrease in the number of cells in the blood (e.g. platelets, red and white blood cells) which may cause paleness, prolonged bleeding, bruising, sore throat and fever have been reported. These symptoms usually vanish when the treatment is discontinued
- Increase of some hepatic enzymes levels, and exceptionally a liver disease,
- your vision may be affected for a short time especially at the start of treatment. This effect is due to changes in blood sugar levels.
Ask your doctor or pharmacist to answer any questions you may have.
Do not be alarmed by this list of possible side effects. You may not experience any of them.
Tell your doctor if you notice any of the following and they worry you:
- stomach upset such as feeling sick (nausea), heartburn
- constipation or a feeling of fullness in the stomach
- headache
- tiredness.
Tell your doctor immediately if you notice any of the following symptoms:
- Skin rash, redness itching and/ or hives, angioedema (rapid swelling of tissues such as eyelids, face, lips, mouth, tongue or throat that may result in breathing difficulty) have been reported. The rash may progress to widespread blistering or peeling of the skin and may be the first sign of rare life threatening conditions (e.g Stevens-Johnson syndrome (SJS), toxic epidermal necrolysis (TEN) and severe hypersensitivity reactions (DRESS).
- As for other sulphonylureas, the following adverse events have been observed: cases of severe changes in the number of blood cells and allergic inflammation of the wall of blood vessels, reduction in blood sodium (hyponatraemia), symptoms of liver impairment (e.g. jaundice) which in most cases disappeared after withdrawal of the sulfonylurea, but may lead to life-threatening liver failure in isolated cases
Other side effects not listed above may also occur in some people. Tell your doctor if you notice anything that is making you feel unwell.
After using it
Storage
Keep your medicine where children cannot reach it. A locked cupboard at least one-and-a-half metres above the ground is a good place to store medicines.
Keep your tablets in a cool dry place where the temperature stays below 30°C.
Do not store NIDEM or any other medicine in the bathroom or near a sink.
Do not leave it in the car or on window sills. Heat and dampness can destroy some medicines.
Disposal
If your doctor tells you to stop taking NIDEM, or your tablets have passed their expiry date, ask your pharmacist what to do with any that are left over.
Product description
What it looks like
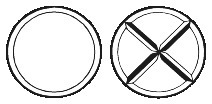
NIDEM is a white to off white round, bevel-edged, uncoated tablet with cross score (+) on one face and plain on the other.
Each pack contains 100 tablets.
Ingredients
The active ingredient in NIDEM is gliclazide. Each NIDEM tablet contains 80 mg of gliclazide.
The tablets also contain:
- lactose monohydrate
- microcrystalline cellulose
- povidone
- sodium starch glycollate type A
- purified talc
- magnesium stearate.
The tablets do not contain gluten, sucrose, tartrazine or any other azo dyes.
The tablets contain sugars as lactose.
Sponsor
Arrow Pharma Pty Ltd
15-17 Chapel Street
Cremorne VIC 3121
Australia
Australian registration number: NIDEM – AUST R 79023
Recognising and treating hyPOglycaemia (very LOW blood sugar levels)
Hypoglycaemia may occur during NIDEM treatment.
The first signs of hypoglycaemia are usually weakness, trembling or shaking, sweating, lightheadedness, dizziness, headache or lack of concentration, irritability, tearfulness,hunger, and/ or numbness around the lips and tongue.
At the first signs of hypoglycaemia take some sugar to raise your blood sugar level quickly. Do this by eating 5 to 7 jelly beans, 3 teaspoons of sugar or honey, drinking half a can of non-diet soft drink, taking 2-3 glucose tablets or a tube of glucose gel.
Then take some extra carbohydrates
such as plain biscuits, fruit or milk - unless you are within 10-15 minutes of your next meal. Taking this extra carbohydrate will help to prevent a second drop in your blood glucose level.
If not treated quickly,
hypoglycaemia symptoms may progress to loss of co-ordination, slurred speech, confusion, fits or loss of consciousness.
If hypoglycaemia symptoms do not get better straight away after taking sugar then go to the Accident and Emergency department at your nearest hospital - if necessary by calling an ambulance.
Contact your doctor or diabetes educator for advice if you are concerned about hypoglycaemia.
Recognising and treating hyPERglycaemia (HIGH blood sugar levels)
Some people may feel fine when their glucose levels are high. Others notice symptoms of hyperglycaemia like tiredness, lack of energy, thirst, passing large amounts of urine, headache, and/or blurred vision.
If you notice symptoms of hyperglycaemia , or your blood sugar levels are high, tell your doctor immediately. You may need adjustments of the dose or type of medicines you are taking.
It is very important to control high blood glucose whether or not you feel unwell. This really helps to avoid serious long-term health Problems, which can involve the heart, eyes, circulation, and/or kidneys.
If you experience any of the signs of hyperglycaemia (high blood glucose) contact your doctor or diabetes educator for advice immediately
This leaflet was last revised in November 2021.
Published by MIMS January 2022