WHAT IS IN THIS LEAFLET
This leaflet answers some common questions about OZOLE (fluconazole 150 mg) capsules.
It does not contain all the available information.
It does not take the place of talking to your doctor or pharmacist.
All medicines have risks and benefits. Your doctor has weighed the risks of you taking OZOLE against the benefits it is expected to have for you.
If you have any concerns about using/taking this medicine, ask your doctor or pharmacist.
Keep this leaflet with this medicine. You may need to read it again.
WHAT OZOLE IS USED FOR
OZOLE contains the active ingredient fluconazole. It is used to treat vaginal thrush in women, when topical treatment has failed. If this is the first time you have had symptoms, talk to your doctor before using any treatment.
Treating vaginal thrush in women
Taken by mouth, OZOLE treats the yeast infection, vaginal thrush, which is caused by a yeast called Candida albicans. Most women have vaginal thrush some time during their lives. Many women have this yeast living harmlessly within their bodies. However, the natural balance that keeps Candida albicans under control can be upset by other factors, e.g. antibiotics, diabetes, the Pill, wearing tight clothing, or using perfumed soaps, bath additives and vaginal deodorants. When the levels of yeast become too high, thrush develops.
You may have one or more of these common symptoms:
- Vaginal itching
- Vaginal burning and redness
- Pain during intercourse
- A white, curdy, odourless discharge from the vagina (like cottage cheese)
Rubbing and scratching can aggravate the soreness and itching. Also, the salt in urine can sting the sore tissue.
BEFORE YOU TAKE OZOLE
Do not use OZOLE:
- If you are pregnant, suspect you might be pregnant or are trying to become pregnant or are breast-feeding
- If you are allergic to any of the ingredients in OZOLE or other thrush treatments such as miconazole, clotrimazole or ketoconazole
- If you are taking cisapride (a medicine to treat stomach problems), astemizole (used in the treatment of allergy symptoms), erythromycin (an antibiotic used to treat bacterial infections), pimozide (an antipsychotic medication), quinidine (used to treat abnormal heart rhythms) and terfenadine (used to treat allergic conditions).
Do not use OZOLE unless you have spoken to your doctor or pharmacist about the following:
- If you are taking any medicines. Some medicines and OZOLE may interfere with each other. These include amiodarone, anticoagulants (anticoagulant medicines reduce the blood's natural ability to clot), cyclosporin, oral contraceptives, phenytoin, short acting benzodiazepines, rifabutin, tacrolimus, theophylline, zidovudine, warfarin, gastrointestinal drugs and oral hypoglycaemics (oral hypoglycaemics are medicines to treat diabetes).
- Tell your doctor or pharmacist before using OZOLE if you are taking warfarin, as bleeding or bruising may occur
- If you are unsure about the cause of your symptoms
- If you have had thrush more than twice in the last six months
- If you have any disease or illness affecting your liver or kidneys or have any unexplained jaundice
- If you have had heart problems
- If you or your partner have had exposure to a sexually transmitted disease
- If you have had any abnormal or irregular vaginal bleeding or a blood stained discharge
- If you have vulval or vaginal sores, ulcers or blisters
- If you are experiencing lower abdominal pain or burning on passing urine
HOW OZOLE IS GIVEN
How much to take
The complete OZOLE course of treatment for thrush is one capsule, once.
How to take it
Take by mouth with a drink of water at any time of day, with or without food.
OZOLE is not recommended for children.
SIDE EFFECTS
Taking this medicine may cause mild side effects such as nausea or feeling sick, headache, stomach pain, indigestion or diarrhoea.
Consult your doctor if you notice anything that is making you feel unwell.
A few people develop allergic reactions to medicines. If you experience difficulty breathing, facial swelling or general itchiness, consult your doctor immediately.
AFTER TAKING OZOLE
You should notice an improvement in your symptoms in a day or two. Consult your doctor if you are no better in 3 days.
How you may avoid thrush in future
- Wear cotton briefs, stockings and loose fitting clothes rather than tight synthetic clothing
- Wash regularly but do not wash and dry yourself too harshly
- Avoid perfumed soaps, bath additives and vaginal deodorants
STORAGE
Keep OZOLE where children cannot reach it.
Keep your capsule in the pack until it is time to take it.
If you take your capsule out of the pack it may not keep as well.
Keep OZOLE in a cool dry place where temperatures stay below 25°C.
Do not store OZOLE or any other medicine in the bathroom or near a sink. Do not leave your medicines on a window sill or in the car. Heat and dampness can destroy some medicines.
Do not use after the expiry date stamped on the pack.
PRODUCT DESCRIPTION
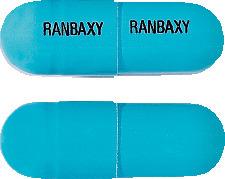
What it looks like
OZOLE 150 mg capsules are hard gelatin capsules, with a blue opaque body and a blue opaque cap. The body and cap have 'RANBAXY' printed in black edible ink. Available in blister packs containing one capsule.
Ingredients
Active ingredient:
Each capsule contains 150 mg fluconazole.
Inactive ingredients:
Other ingredients are lactose, maize starch, colloidal anhydrous silica, magnesium stearate, sodium lauryl sulfate, the colours patent blue V and titanium dioxide, and a gelatin capsule shell.
Australian Registration Number
OZOLE 150 mg: AUST R 122904
Sponsor
OZOLE is supplied in Australia by:
Sun Pharma ANZ Pty Ltd
Suite 2.02, Level 2
12 Waterloo Road
Macquarie Park NSW 2113
This leaflet was prepared in September 2018.
Published by MIMS November 2020

 Molecular formula: C13H12F2N6O.
Molecular formula: C13H12F2N6O.