What is in this leaflet
This leaflet answers some common questions about PIOGLITAZONE AN.
It does not contain all of the available information. It does not take the place of talking to your doctor or pharmacist.
All medicines have benefits and risks. Your doctor has weighed the risks of you taking PIOGLITAZONE AN against the benefits they expect it will have for you.
If you have any concerns about taking this medicine, talk to your doctor or pharmacist.
Keep this leaflet with your medicine.
You may need to read it again.
What PIOGLITAZONE AN is used for
PIOGLITAZONE AN is a tablet that is used to improve the action of the body's naturally produced insulin. PIOGLITAZONE AN is used in the management of type 2 diabetes not controlled by diet.
PIOGLITAZONE AN helps to control the level of glucose in your blood when you have type 2 diabetes. This is the 'adult onset' type of diabetes and is controlled by diet, certain oral medications and occasionally insulin.
This medicine is also called pioglitazone hydrochloride and belongs to a group of medicines called glitazones. Glitazones decrease insulin resistance.
Ask your doctor if you have any questions about why this medicine has been prescribed for you.
Your doctor may have prescribed it for another reason.
PIOGLITAZONE AN can be used alone (when diet and exercise is not enough to treat your diabetes) or together with other anti-diabetic medicines.
This medicine is available only with a doctor's prescription.
The use of PIOGLITAZONE AN has not been studied in children.
Before You Take PIOGLITAZONE AN
When you must not take PIOGLITAZONE AN
Do not take PIOGLITAZONE AN if:
- you have heart failure requiring treatment. Talk to your doctor if you have heart failure
- you have type 1 diabetes or diabetic ketoacidosis (often caused b very high blood glucose levels)
- you have had an allergy to any medicine containing pioglitazone hydrochloride or any of the ingredients listed at the end of this leaflet (see ‘product description’).
Some of the symptoms of an allergic reaction may include shortness of breath, wheezing or difficulty breathing; swelling of the face, lips, tongue or other parts of the body; rash, itching or hives on the skin.
Do not take this medicine after the date printed on the pack or if the packaging is torn or shows signs of tampering.
If it has expired or is damaged, return it to your pharmacist for disposal.
If you are not sure whether you should start taking this medicine, talk to your doctor.
Before you start to take PIOGLITAZONE AN
Tell your doctor if you are allergic to any other medicines, foods, dyes or preservatives.
Tell your doctor if you have had any of the following medical conditions:
- heart disease with shortness of breath after minimal physical activity
- heart disease with severe symptoms at rest
- swelling of hands, ankles or feet
- bladder cancer or symptoms associated with bladder cancer such as blood n the urine (hematuria) often accompanied by pain and burning
- problems with your liver
- problems with your kidneys that requires dialysis. PIOGLITAZONE AN is not recommended for use if you are on dialysis
- some women who don’t have monthly periods and have not been through menopause may restart their periods when taking PIOGLITAZONE AN. These women may be at increased risk of pregnancy.
- Bone fractures, usually in the hand, upper arm or foot have been seen in some women when taking PIOGLITAZONE AN. Talk to your doctor for advice on how to keep your bones healthy.
Tell your doctor if you are pregnant or plan to become pregnant or are breast feeding.
Like most medicines, PIOGLITAZONE AN is not recommended for use during pregnancy. If there is a need to consider PIOGLITAZONE AN during your pregnancy, your doctor will discuss with you the benefits and risks of taking PIOGLITAZONE AN. It is recommended that you do not breast feed while taking PIOGLITAZONE AN, as it is not known whether this medicine passes into breast milk.
Tell your doctor if you are using another medicine for diabetes. PIOGLITAZONE AN can enhance the action of other medicines. You may be at risk of low blood sugar (hypoglycaemia).
If this happens, your doctor may need to adjust the dose of your other medicines.
Tell your doctor if you suffer from lactose intolerance (because PIOGLITAZONE AN contain lactose).
Taking other medicines
Tell your doctor if you are taking any other medicines, including any that you buy without a prescription from a pharmacy, supermarket or health food shop.
Some medicines and PIOGLITAZONE AN may interfere with each other. These include:
- Chlorpropamide
- Gemfibrozil
- Glibenclamide
- Gliclazide
- Insulin
- Metformin
- Oral contraceptives
- Rifampicin
- Tolbutamide
These medicines may be affected by PIOGLITAZONE AN or may affect how well it works. You may need different amounts of your medicines or you may need to take different medicines.
Your doctor or pharmacist has more information on medicines to be careful with or avoid while taking this medicine.
How to take PIOGLITAZONE AN
Follow all directions given to you by your doctor or pharmacist carefully.
They may differ from the information contained in this leaflet.
If you do not understand the instructions on the carton, ask your doctor or pharmacist for help.
How much to take
Your doctor will tell you how many PIOGLITAZONE AN tablets you should take. The dose your doctor will prescribe for you will usually be in the range of 15 mg to 45 mg per day
PIOGLITAZONE AN tablets should be taken once a day as advised by your doctor.
Your doctor may increase or decrease your dose in order to find the appropriate dose for your condition
How to take PIOGLITAZONE AN
PIOGLITAZONE AN should be swallowed whole with a glass of water.
When to take PIOGLITAZONE AN
Take your medicine at about the same time each day.
Taking it at the same time each day will have the best effect. It will also help you remember when to take it.
It does not mater if you take this medicine before or after food.
How long to take PIOGLITAZONE AN
Continue taking your medicine for as long as your doctor tells you.
This medicine helps to control your condition, but does not cure it. It is important to keep taking your medicine even if you feel well.
If you forget to take PIOGLITAZONE AN
If it is almost time for your next dose, skip the dose you missed and take your next dose when you are meant to.
Otherwise, take the missed dose as soon as you remember, and then go back to taking your tablets as you would normally.
Do not take a double dose to make up for the dose you missed.
If you are not sure what to do, ask your doctor or pharmacist.
If you have trouble remembering to take your medicine, ask your pharmacist for some hints.
If you take too much (overdose)
Immediately telephone your doctor or the Poisons Information Centre (telephone 13 11 26) for advice, or go to Accident and Emergency at the nearest hospital, if you think you or anyone else may have taken too much PIOGLITAZONE AN. Do this even if there are no signs of discomfort or poisoning.
You may need urgent medical attention.
While you are taking PIOGLITAZONE AN
Things you must do
It is important that you remember to take PIOGLITAZONE AN daily and at the dose prescribed by your doctor.
Tell any other doctors, dentists and pharmacists who treat you that you are taking PIOGLITAZONE AN.
If you are about to be started on any new medicine, remind your doctor and pharmacist that you are taking PIOGLITAZONE AN.
If you are going to have surgery, tell the surgeon or anaesthetist that you are taking this medicine.
It may affect other medicines used during surgery.
If you become pregnant while taking this medicine, tell your doctor immediately.
If you are about to have any blood tests, tell your doctor that you are taking this medicine.
It may interfere with the results of some tests.
Keep all of your doctor's appointments so that your progress can be checked.
Your doctor may do some tests from time to time to make sure the medicine is working and to prevent unwanted side effects.
Tell your doctor if you have gained weight since taking PIOGLITAZONE AN.
Weight gain can be associated with improved blood sugar control however; it may also be a symptom of heart failure.
Things you must not do
Do not take PIOGLITAZONE AN to treat any other complaints unless your doctor tells you to.
Do not give your medicine to anyone else, even if their symptoms seem similar to yours or they have the same condition as you.
Do not stop taking your medicine or lower the dosage without checking with your doctor.
If you stop taking it suddenly, your condition may worsen or you may have unwanted side effects.
Things to be careful of
PIOGLITAZONE AN alone is unlikely to affect your ability to drive or operate machinery. However, be careful to avoid hypoglycaemia whilst driving or operating machinery if using PIOGLITAZONE AN in combination with other diabetes medicines.
Side Effects
Tell your doctor or pharmacist as soon as possible if you experience any undesirable effect or feel unwell while you are taking PIOGLITAZONE AN.
This medicine helps most people with type 2 diabetes not controlled by diet, but it may have unwanted side effects in some people.
All medicines can have side effects. Sometimes they are serious, most of the time they are not. You may need medical attention if you get some of the side effects.
Some side effects may be related to the dose of PIOGLITAZONE AN. Accordingly, it is important that you tell your doctor as soon as possible about any unwanted effects. Your doctor may then decide to adjust the dose of PIOGLITAZONE AN you are taking.
Do not be alarmed by the following list of side effects. You may not experience any of them.
Ask your doctor or pharmacist to answer any questions you may have.
A few patients have experienced the following side effects whilst taking PIOGLITAZONE AN:
- A small increase in weight
- Low blood sugar levels (hyprglycaemia). This occurs more often with PIOGLITAZONE AN is taken with a sulfonylurea or insulin.
- Heart failure which may show as localised swelling of the ankles, feet and hands (oedema) and/or fluid in the lungs (pulmonary oedema). This has been reported in clinical trials mainly in patients who are taking pioglitazone in combination with insulin.
- Increased risk of fracture in women
- Macular oedema (an eye disorder than can affect vision)
- Altered or impaired liver function.
Tell your doctor if you notice any of the following:
- weight gain
- signs of hypoglycaemia which may include weakness, trembling or shaking, sweating, light-headedness, headache, dizziness, lack of concentration, tearfulness or crying, irritability, hunger, numbness around the lips and fingers
- eye problems including blurred or double vision
The above list includes the more common side effects of this medicine.
Tell your doctor as soon as possible if you notice ant of the following:
- dark urine or pale stools, yellowing of the skin or eyes, severe cramps of the stomach, nausea or vomiting, loss of weight, tiredness
- shortness of breath when at rest or after minimal activity with swelling of legs, feet and hands, rapid increase in weight
- blood in the urine often accompanied by pain and burning. These can be symptoms of bladder cancer.
The above list includes serious side effects which may require medical attention. Serious side effects are rare.
Tell your doctor or pharmacist if you notice anything that is making you feel unwell.
Other side effects not listed above may also occur in some patients.
After taking PIOGLITAZONE AN
Storage
Keep your tablets in the aluminium blister pack until it is time to take them.
Keep your tablets in a cool dry place where the temperature stays below 25 degrees C.
Do not store PIOGLITAZONE AN or any other medicine in the bathroom or near a sink. Do not leave it on the window sill or in the car.
Heat and dampness can destroy some medicines.
Keep it where children cannot reach it.
A locked cupboard at least one-and-a- half metres above the ground is a good please to store medicines..
Disposal
If your doctor tells you to stop taking PIOGLITAZONE AN or the expiry date has passed, ask your pharmacist what to do with any medicine that is left over.
Product description
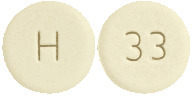
What PIOGLITAZINE AN looks like
PIOGLITAZONE AN 15, 30 & 45 is presented in pack size of 28 tablets in a blister.
PIOGLITAZONE AN 15mg (AUST R 289430)
White to off white, round, biconvex, uncoated tablets, debossed with ‘PIO’ on one side and ‘15’ on the other side
PIOGLITAZONE AN 30mg (AUST R 289431)
White to off white, round, flat faced, bevel edge, uncoated tablets, debossed with ‘PIO’ on one side and ‘30’ on the other side
PIOGLITAZONE AN 45mg (AUST R 289432)
White to off white, round, flat faced, bevel edge, uncoated tablets, debossed with ‘PIO’ on one side and ‘45’ on the other side.
Ingredients
Active Ingredient:
Pioglitazone (as hydrochloride)
Each tablet may contain either 15 mg, 30 mg & 45 mg of pioglitazone as hydrochloride.
Other Ingredients:
- lactose monohydrate
- carmellose calcium
- hyprolose
- magnesium stearate
Please read this leaflet carefully before you start taking PIOGLITAZONE AN. You may wish to keep it to read again.
Name and Address of the Sponsor
Amneal Pharma Australia Pty Ltd.
12 River St, South Yarra
VIC – 3141
Australia
Date of Preparation
August 2017




 The study population included patients not previously treated with antidiabetic medication (naive; 31%) and patients who were receiving antidiabetic medication at the time of study enrolment (previously treated; 69%). The data for the naive and previously treated patient subsets are shown in Table 1. This run-in period was associated with little change in HbA1c and FBG values from screening to baseline for the naive patients. However, for the previously-treated group, washout from previous antidiabetic medication resulted in deterioration of glycaemic control and increases in HbA1c and FBG. With pioglitazone, while most patients in the previously-treated group had a decrease from baseline in HbA1c and FBG in many cases the values did not return to screening levels by the end of the study. The study design did not permit the evaluation of patients who switched directly to pioglitazone from another antidiabetic agent.
The study population included patients not previously treated with antidiabetic medication (naive; 31%) and patients who were receiving antidiabetic medication at the time of study enrolment (previously treated; 69%). The data for the naive and previously treated patient subsets are shown in Table 1. This run-in period was associated with little change in HbA1c and FBG values from screening to baseline for the naive patients. However, for the previously-treated group, washout from previous antidiabetic medication resulted in deterioration of glycaemic control and increases in HbA1c and FBG. With pioglitazone, while most patients in the previously-treated group had a decrease from baseline in HbA1c and FBG in many cases the values did not return to screening levels by the end of the study. The study design did not permit the evaluation of patients who switched directly to pioglitazone from another antidiabetic agent. Pioglitazone has been shown to reduce total plasma triglycerides and free fatty acids and to increase HDL-cholesterol levels. LDL-cholesterol levels remain unchanged. In a 26-week, placebo-controlled, dose-ranging study, mean triglyceride levels decreased in the 15 mg, 30 mg and 45 mg pioglitazone dose groups compared to a mean increase in the placebo group. Mean HDL levels increased to a greater extent in the pioglitazone-treated patients than in the placebo-treated patients. There were no consistent differences for LDL and total cholesterol in pioglitazone-treated patients compared with placebo (Table 2).
Pioglitazone has been shown to reduce total plasma triglycerides and free fatty acids and to increase HDL-cholesterol levels. LDL-cholesterol levels remain unchanged. In a 26-week, placebo-controlled, dose-ranging study, mean triglyceride levels decreased in the 15 mg, 30 mg and 45 mg pioglitazone dose groups compared to a mean increase in the placebo group. Mean HDL levels increased to a greater extent in the pioglitazone-treated patients than in the placebo-treated patients. There were no consistent differences for LDL and total cholesterol in pioglitazone-treated patients compared with placebo (Table 2). In a separate 24-week study, 260 patients with type 2 diabetes were randomised to one of two forced-titration pioglitazone treatment arms (final doses 30 or 45 mg), or a mock titration placebo arm. In one pioglitazone treatment group, patients received an initial dose of 7.5 mg once daily. After four weeks, the dose was increased to 15 mg once daily and after another four weeks: the dose was increased to 30 mg once daily for the remainder of the study (16 weeks). In the second pioglitazone treatment group, patients received an initial dose of 15 mg once daily and were titrated to 30 mg once daily and 45 mg once daily in a similar manner. Treatment with pioglitazone, as described, produced statistically significant improvements in HbA1c and FBG at endpoint compared with placebo (see Table 3).
In a separate 24-week study, 260 patients with type 2 diabetes were randomised to one of two forced-titration pioglitazone treatment arms (final doses 30 or 45 mg), or a mock titration placebo arm. In one pioglitazone treatment group, patients received an initial dose of 7.5 mg once daily. After four weeks, the dose was increased to 15 mg once daily and after another four weeks: the dose was increased to 30 mg once daily for the remainder of the study (16 weeks). In the second pioglitazone treatment group, patients received an initial dose of 15 mg once daily and were titrated to 30 mg once daily and 45 mg once daily in a similar manner. Treatment with pioglitazone, as described, produced statistically significant improvements in HbA1c and FBG at endpoint compared with placebo (see Table 3). For patients who had not been previously treated with antidiabetic medication (24%), mean values at screening were 10.1% for HbA1c and 13.22 mmol/L for FBG. At baseline, mean HbA1c was 10.2% and mean FBG was 13.5 mmol/L. Compared with placebo, treatment with pioglitazone titrated to a final dose of 30 mg and 45 mg resulted in reductions from baseline in mean HbA1c of 2.3% and 2.6% and mean FBG of 3.5 mmol/L and 5.28 mmol/L, respectively. For patients who had been previously treated with antidiabetic medication (76%), this medication was discontinued at screening. Mean values at screening were 9.4% for HbA1c and 12 mmol/L for FBG. At baseline, mean HbA1c was 10.7% and mean FBG was 16.11 mmol/L. Compared with placebo, treatment with pioglitazone titrated to a final dose of 30 mg and 45 mg resulted in reductions from baseline in mean HbA1c of 1.3% and 1.4% and mean FBG of 3.06 mmol/L and 3.33 mmol/L, respectively. For many previously-treated patients, HbA1c and FBG had not returned to screening levels by the end of the study.
For patients who had not been previously treated with antidiabetic medication (24%), mean values at screening were 10.1% for HbA1c and 13.22 mmol/L for FBG. At baseline, mean HbA1c was 10.2% and mean FBG was 13.5 mmol/L. Compared with placebo, treatment with pioglitazone titrated to a final dose of 30 mg and 45 mg resulted in reductions from baseline in mean HbA1c of 2.3% and 2.6% and mean FBG of 3.5 mmol/L and 5.28 mmol/L, respectively. For patients who had been previously treated with antidiabetic medication (76%), this medication was discontinued at screening. Mean values at screening were 9.4% for HbA1c and 12 mmol/L for FBG. At baseline, mean HbA1c was 10.7% and mean FBG was 16.11 mmol/L. Compared with placebo, treatment with pioglitazone titrated to a final dose of 30 mg and 45 mg resulted in reductions from baseline in mean HbA1c of 1.3% and 1.4% and mean FBG of 3.06 mmol/L and 3.33 mmol/L, respectively. For many previously-treated patients, HbA1c and FBG had not returned to screening levels by the end of the study. For patients who had not been previously treated with antidiabetic medication (40%), mean values at screening were 10.3% for HbA1c and 13.33 mmol/L for FBG. At baseline, mean HbA1c was 10.4% and mean FBG was 14.11 mmol/L. Compared with placebo, treatment with pioglitazone 30 mg resulted in reductions from baseline in mean HbA1c of 1.0% and mean FBG of 3.44 mmol/L. For patients who had been previously treated with antidiabetic medication (60%), this medication was discontinued at screening. Mean values at screening were 9.4% for HbA1c and 12 mmol/L for FBG. At baseline, mean HbA1c was 10.6% and mean FBG was 15.94 mmol/L. Compared with placebo, treatment with pioglitazone 30 mg resulted in reductions from baseline in mean HbA1c of 1.3% and mean FBG of 2.56 mmol/L. For many previously-treated patients, HbA1c and FBG had not returned to screening levels by the end of the study.
For patients who had not been previously treated with antidiabetic medication (40%), mean values at screening were 10.3% for HbA1c and 13.33 mmol/L for FBG. At baseline, mean HbA1c was 10.4% and mean FBG was 14.11 mmol/L. Compared with placebo, treatment with pioglitazone 30 mg resulted in reductions from baseline in mean HbA1c of 1.0% and mean FBG of 3.44 mmol/L. For patients who had been previously treated with antidiabetic medication (60%), this medication was discontinued at screening. Mean values at screening were 9.4% for HbA1c and 12 mmol/L for FBG. At baseline, mean HbA1c was 10.6% and mean FBG was 15.94 mmol/L. Compared with placebo, treatment with pioglitazone 30 mg resulted in reductions from baseline in mean HbA1c of 1.3% and mean FBG of 2.56 mmol/L. For many previously-treated patients, HbA1c and FBG had not returned to screening levels by the end of the study.



 In the PROactive study, which involved a high risk population of patients with pre-existing macrovascular disease, treatment emergent adverse events that occurred more often in the pioglitazone group compared to placebo group were oedema (26.4% and 15.1% respectively), hypoglycaemia (27.2% and 18.8% respectively) and cardiac failure, including serious and non-serious cases (12.6% and 8.7% respectively).
In the PROactive study, which involved a high risk population of patients with pre-existing macrovascular disease, treatment emergent adverse events that occurred more often in the pioglitazone group compared to placebo group were oedema (26.4% and 15.1% respectively), hypoglycaemia (27.2% and 18.8% respectively) and cardiac failure, including serious and non-serious cases (12.6% and 8.7% respectively).