SUMMARY CMI
RETROVIR
Consumer Medicine Information (CMI) summary
The full CMI on the next page has more details. If you are worried about using this medicine, speak to your doctor or pharmacist.
1. Why am I taking RETROVIR?
RETROVIR contains the active ingredient zidovudine. RETROVIR is used, alone or in combination with other antiretrovirals, to slow down the progression of human immunodeficiency virus (HIV) infection which can lead to Acquired Immune Deficiency Syndrome (AIDS) and other related illnesses (e.g. AIDS-related Complex (ARC)).
For more information, see Section 1. Why am I taking RETROVIR? in the full CMI.
2. What should I know before I take RETROVIR?
Do not use if you have ever had an allergic reaction to RETROVIR or any of the ingredients listed at the end of the CMI.
Talk to your doctor if you have any other medical conditions, take any other medicines, or are pregnant or plan to become pregnant or are breastfeeding.
For more information, see Section 2. What should I know before I take RETROVIR? in the full CMI.
3. What if I am taking other medicines?
Some medicines may interfere with RETROVIR and affect how it works.
A list of these medicines is in Section 3. What if I am taking other medicines? in the full CMI.
4. How do I use RETROVIR?
- The usual dosage of RETROVIR is 500 mg to 600 mg daily taken as a divided dose (can be between two and five separate doses).
- A daily dose of 1000 mg taken in two divided doses can also be prescribed.
- Swallow the capsules with some water.
More instructions can be found in Section 4. How do I take RETROVIR? in the full CMI.
5. What should I know while taking RETROVIR?
| Things you should do |
|
| Things you should not do |
|
| Driving or using machines |
|
| Looking after your medicine |
|
For more information, see Section 5. What should I know while taking RETROVIR? in the full CMI.
6. Are there any side effects?
Side effects that have been reported include body odour, chills, increased sensitivity to pain, back pain, chest pain, weakness, weight loss, loss of appetite, generally feeling unwell, feeling faint and fainting, constipation, blood in the stool, difficulty in swallowing, mouth ulcers, bleeding gums, heartburn, vomiting, nausea, nose bleeds, muscle aches or pains, muscle spasms or twitching, confusion, depression, nervousness, loss of mental clarity, dizziness, seizures, headache, sleeplessness, cough, sore throat, hay fever, acne, itchiness, changes in nail, skin or mouth colour, vision problems, sensitivity to light, hearing loss, passing too much urine and increased frequency of urination.
For more information, including what to do if you have any side effects, see Section 6. Are there any side effects? in the full CMI.
FULL CMI
RETROVIR
Active ingredient(s): zidovudine
Consumer Medicine Information (CMI)
This leaflet provides important information about using RETROVIR. You should also speak to your doctor or pharmacist if you would like further information or if you have any concerns or questions about using RETROVIR.
Where to find information in this leaflet:
1. Why am I taking RETROVIR?
2. What should I know before I take RETROVIR?
3. What if I am taking other medicines?
4. How do I take RETROVIR?
5. What should I know while taking RETROVIR?
6. Are there any side effects?
7. Product details
1. Why am I taking RETROVIR?
RETROVIR contains the active ingredient zidovudine. RETROVIR belongs to a group of medicines called antiretrovirals.
RETROVIR is used, alone or in combination with other antiretrovirals, to slow down the progression of human immunodeficiency virus (HIV) infection which can lead to Acquired Immune Deficiency Syndrome (AIDS) and other related illnesses (e.g. AIDS-related Complex (ARC)).
RETROVIR does not cure AIDS or HIV infection however it slows down production of HIV in the body. In this way it stops ongoing damage to the body's immune system which fights infection.
You can still pass on HIV when taking this medicine through sexual activity or through passing on blood or bodily secretions which carry the HIV virus, although the risk is lowered by taking antiretroviral therapy.
You should use proper precautions to prevent this from occurring. Discuss with your doctor the precautions needed to avoid infecting other people.
While taking RETROVIR and/or any other therapy for HIV, you may continue to develop other infections and other complications of HIV infection. You should keep in regular contact with your doctor.
2. What should I know before I take RETROVIR?
Warnings
Do not use RETROVIR if:
- you are allergic to zidovudine, or any of the ingredients listed at the end of this leaflet.
Always check the ingredients to make sure you can use this medicine. - you weigh less than 30 kg
- you have a reduced red blood cell count (anaemia) or white blood cell count (neutropenia)
Check with your doctor if you:
- have any other medical conditions
- take any medicines for any other condition
- are allergic to any other foods, dyes, preservatives or medicines
During treatment, you may be at risk of developing certain side effects. It is important you understand these risks and how to monitor for them. See additional information under Section 6. Are there any side effects?
Pregnancy and breastfeeding
Talk to your doctor if you are pregnant or intend to become pregnant.
Talk to your doctor if you are breastfeeding or intend to breastfeed.
Your doctor can discuss with you the benefits and risks of taking RETROVIR whilst pregnant or breastfeeding.
Symptoms of infection and inflammation
People with advanced HIV infection (AIDS) have weak immune systems and are more likely to develop serious infections (opportunistic infections). When they start treatment, the immune system becomes stronger and so the body starts to fight infections.
Symptoms of infection and inflammation may develop, caused by either:
- old, hidden infections flaring up at the body fights them
- the immune system attacking healthy body tissue (autoimmune disorders)
The symptoms of autoimmune disorders may develop many months after you start taking medications to treat your HIV infection.
Symptoms may include:
- muscle weakness and/or muscle pain
- joint pain or swelling
- weakness beginning in the hands or feet and moving towards the trunk of the body
- palpitations or tremor
- hyperactivity (excessive restlessness and movement)
If you get symptoms of infection or if you notice any of the symptoms above, tell your doctor immediately. Do not take other medicines for the infection without your doctor's advice.
3. What if I am taking other medicines?
Tell your doctor or pharmacist if you are taking any other medicines, including any medicines, vitamins or supplements that you buy without a prescription from your pharmacy, supermarket or health food shop.
Some medicines may interfere with RETROVIR and affect how it works.
If you take ribavirin (e.g. Ibavyr) and RETROVIR together it may cause or worsen anaemia (low red blood cells). Tell your doctor if you notice symptoms of anaemia such as tiredness and shortness of breath.
Tell your doctor if you are taking any of the medicines below:
- medicines used to treat pain including paracetamol, aspirin, codeine, morphine, methadone, indomethacin, ketoprofen, naproxen
- medicines used in epilepsy including phenytoin
- medicines used to treat anxiety and insomnia including oxazepam, lorazepam
- cimetidine, a medicine used to treat heartburn, stomach ulcers
- clofibrate, a medicine used to treat high cholesterol, high triglycerides
- probenecid, a medicine used in the treatment of gout
- antimicrobial medicines such as pentamidine
- medicines used to treat parasite infections including pyrimethamine, dapsone
- antimicrobial medicines including atovaquone
- amphotericin, flucytosine, medicines used to treat fungal infections
- other antiviral medicines such as ganciclovir, interferon
- clarithromycin, an antibacterial medicine
- medicines used in the treatment of cancer including vincristine, vinblastine and doxorubicin
Check with your doctor or pharmacist if you are not sure about what medicines, vitamins or supplements you are taking and if these affect RETROVIR.
4. How do I take RETROVIR?
How much to take
- The usual dosage of RETROVIR is 500 mg to 600 mg daily taken as a divided dose. This may be taken across two to five separate doses.
- A daily dose of 1000 mg in two divided doses can also be prescribed.
- Follow the instructions provided by your doctor or pharmacist and use RETROVIR until your doctor tells you to stop.
How to take RETROVIR
- Swallow the capsule whole with a drink of water.
If you forget to take RETROVIR
RETROVIR should be used regularly at the same time each day.
If it is almost time for your next dose, skip the dose you missed and take your next dose when you are meant to. Otherwise, take it as soon as you remember and then go back to taking your medicine as you would normally.
Do not take a double dose to make up for the dose you missed.
If you take too much RETROVIR
If you think that you have taken too much RETROVIR, you may need urgent medical attention.
You should immediately:
- phone the Poisons Information Centre
(by calling 13 11 26), or - contact your doctor, or
- go to the Emergency Department at your nearest hospital.
You should do this even if there are no signs of discomfort or poisoning.
5. What should I know while taking RETROVIR?
Things you should do
Ensure you have blood tests when you are meant to. It is important that your doctor monitors your health and checks the levels of red and white blood cells. If you develop anaemia or neutropenia your doctor may reduce your dose or stop RETROVIR.
Tell your doctor straight away if you:
- become pregnant or intend to become pregnant
- have not taken RETROVIR as intended
Remind any doctor, dentist or pharmacist you visit that you are using RETROVIR.
This is especially important for any medicines that might have an effect on your liver, kidneys, red or white blood cells or other cells in the body.
Stay in regular contact with your doctor
RETROVIR helps to control your condition, but it is not a cure for HIV infection. You need to keep taking it everyday to stop your illness from getting worse. Because RETROVIR does not cure HIV infections, you may still develop other infections and illnesses linked to HIV.
Things you should not do
- Do not stop taking this medicine suddenly or change the dose.
- Do not give this medicine to anyone else, even if their symptoms seem similar to yours.
- Do not use this medicine to treat any other complaints unless your doctor tells you to.
Driving or using machines
Be careful before you drive or use any machines or tools until you know how RETROVIR affects you.
Looking after your medicine
Keep RETROVIR in the pack until it is time to take it.
Store it in a cool dry place (below 30°C) away from moisture, heat or sunlight; for example, do not store it:
- in the bathroom or near a sink, or
- in the car or on window sills.
Keep it where young children cannot reach it.
Getting rid of any unwanted medicine
If you no longer need to use this medicine or it is out of date, take it to any pharmacy for safe disposal.
Do not use this medicine after the expiry date.
6. Are there any side effects?
All medicines can have side effects. If you do experience any side effects, most of them are minor and temporary. However, some side effects may need medical attention.
Within the first few weeks of treatment with anti-HIV medicines, some people, particularly those that have been HIV positive for some time, may develop inflammatory reactions (e.g. pain, redness, swelling, high temperature) which may resemble an infection and may be severe. It is thought that these reactions are caused by a recovery in the body's ability to fight infections, previously suppressed by HIV.
If you become concerned about any new symptoms, or any changes in your health after starting HIV treatment, discuss with your doctor immediately.
See the information below and, if you need to, ask your doctor or pharmacist if you have any further questions about side effects.
Less serious side effects
| Less serious side effects | What to do |
| Speak to your doctor if you have any of these less serious side effects and they worry you. |
Serious side effects
| Serious side effects | What to do |
The frequency and severity of anaemia and neutropenia are greater in patients with advanced HIV disease or in patients who start taking RETROVIR in the later stages of HIV disease.
Treatment with RETROVIR may cause a loss of fat from the legs, arms and face (lipoatrophy). If this occurs tell your doctor and they will assess if you should stop taking RETROVIR and your HIV treatment be changed. If you stop taking RETROVIR it may take several months to see any lost fat return and you might not regain it all. If you are taking medication for HIV and become unwell with fast breathing, stop taking RETROVIR and talk to your doctor immediately. This might be a condition known as ‘lactic acidosis’. The fast breathing is due to high acid levels in the blood. Your liver may not be working properly and gets big and fatty and can be life threatening. This illness occurs more often in women than men. | Call your doctor straight away, or go straight to the Emergency Department at your nearest hospital if you notice any of these serious side effects. |
Tell your doctor or pharmacist if you notice anything else that may be making you feel unwell.
Other side effects not listed here may occur in some people.
Reporting side effects
After you have received medical advice for any side effects you experience, you can report side effects to the Therapeutic Goods Administration online at www.tga.gov.au/reporting-problems. By reporting side effects, you can help provide more information on the safety of this medicine.
Always make sure you speak to your doctor or pharmacist before you decide to stop taking any of your medicines.
7. Product details
This medicine is only available with a doctor's prescription.
What RETROVIR capsules contain
| Active ingredient (main ingredient) | zidovudine |
| Other ingredients (inactive ingredients) | gelatin indigo carmine (250 mg capsules only) magnesium stearate maize starch microcrystalline cellulose polysorbate 80 sodium starch glycollate titanium dioxide |
What RETROVIR syrup contains
| Active ingredient (main ingredient) | zidovudine |
| Other ingredients (inactive ingredients) | citric acid glycerol maltitol solution sodium saccharin sodium benzoate Strawberry Flavour PHL-134189 White Sugar Flavour DA13780 purified water |
| Potential allergens | maltitol solution sodium benzoate saccharin sodium |
Do not take this medicine if you are allergic to any of these ingredients.
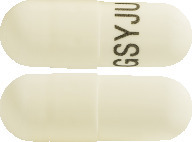
What RETROVIR looks like
RETROVIR capsules are available in 2 strengths:
- 100 mg capsules: opaque white cap and body coded GSYJU. Available in blister packs of 100 capsules.
AUST R 178383 - 250 mg capsules: opaque blue cap and opaque white body coded GSJV2. Available in blister packs of 40 or 60 capsules.
AUST R 178384
Not all pack sizes may be marketed.
RETROVIR syrup is a pale yellow, strawberry flavoured liquid and is supplied in a 200 mL bottle with a syringe, syringe adaptor and a plastic cap.
AUST R 41043
Who distributes RETROVIR
ViiV Healthcare Pty Ltd
Level 4, 436 Johnson Street
Abbotsford VIC 3067
Australia
Trademarks are owned by or licenced to the ViiV Healthcare group of companies.
© 2022 ViiV Healthcare group of companies or its licensor.
This leaflet was prepared October 2022
Version 9.0
Published by MIMS March 2023


 Patients with advanced renal failure should receive Retrovir at the lower end of the dosage range. Haematological parameters and clinical response may influence the need for subsequent dosage adjustment. Haemodialysis and peritoneal dialysis have no significant effect on zidovudine elimination. In a small number of patients haemodialysis would appear to be more efficient in eliminating the glucuronide metabolite than peritoneal dialysis.
Patients with advanced renal failure should receive Retrovir at the lower end of the dosage range. Haematological parameters and clinical response may influence the need for subsequent dosage adjustment. Haemodialysis and peritoneal dialysis have no significant effect on zidovudine elimination. In a small number of patients haemodialysis would appear to be more efficient in eliminating the glucuronide metabolite than peritoneal dialysis.

 The most serious adverse reactions include anaemia (which may require transfusions), neutropenia and leucopenia. These occur more frequently at higher dosages (1200-1500 mg/day) and in patients with advanced HIV disease (especially when there is poor bone marrow reserve prior to treatment), particularly in patients with CD4 cell counts less than 100/mm3. Dosage reduction or cessation of therapy may become necessary (see Section 4.2 Dose and Method of Administration). The anaemia appeared to be the result of impaired erythrocyte maturation as evidenced by increasing macrocytosis (MCV) while on the drug.
The most serious adverse reactions include anaemia (which may require transfusions), neutropenia and leucopenia. These occur more frequently at higher dosages (1200-1500 mg/day) and in patients with advanced HIV disease (especially when there is poor bone marrow reserve prior to treatment), particularly in patients with CD4 cell counts less than 100/mm3. Dosage reduction or cessation of therapy may become necessary (see Section 4.2 Dose and Method of Administration). The anaemia appeared to be the result of impaired erythrocyte maturation as evidenced by increasing macrocytosis (MCV) while on the drug. Clinical adverse events which occurred in less than 5% of all patients treated with zidovudine in the advanced HIV study are listed below. Since many of these adverse events were seen in placebo-treated patients as well as zidovudine recipients, their possible relationship to the drug is unknown.
Clinical adverse events which occurred in less than 5% of all patients treated with zidovudine in the advanced HIV study are listed below. Since many of these adverse events were seen in placebo-treated patients as well as zidovudine recipients, their possible relationship to the drug is unknown.
 The following events have also been reported in patients treated with zidovudine. They may occur as part of the underlying disease process or as a result of the wide range of drugs used in the management of HIV disease. The relationship between these events and the use of zidovudine is therefore difficult to evaluate, particularly in the medically complicated situations which characterise advanced HIV disease. If the severity of the symptoms warrants it, a reduction or suspension of zidovudine therapy may assist in the assessment and management of these conditions:
The following events have also been reported in patients treated with zidovudine. They may occur as part of the underlying disease process or as a result of the wide range of drugs used in the management of HIV disease. The relationship between these events and the use of zidovudine is therefore difficult to evaluate, particularly in the medically complicated situations which characterise advanced HIV disease. If the severity of the symptoms warrants it, a reduction or suspension of zidovudine therapy may assist in the assessment and management of these conditions: Treatment with zidovudine has been associated with loss of subcutaneous fat (see Section 4.4 Special Warnings and Precautions for Use).
Treatment with zidovudine has been associated with loss of subcutaneous fat (see Section 4.4 Special Warnings and Precautions for Use). Clinical end-point data from a prospective study indicate that lamivudine in combination with zidovudine alone or in combination with zidovudine containing treatment regimens results in a significant reduction in the risk of disease progression and mortality.
Clinical end-point data from a prospective study indicate that lamivudine in combination with zidovudine alone or in combination with zidovudine containing treatment regimens results in a significant reduction in the risk of disease progression and mortality. The data showed there was a significant reduction in progression to the combined endpoint of a new AIDS event or death for patients who received lamivudine in combination with zidovudine containing regimens compared to patients maintained on zidovudine containing regimens alone (p < 0.0001). The Hazard Ratio (HR) was 0.427 (95% confidence interval 0.318-0.572), or a 57% reduction in risk. In addition, the data indicated a significant reduction in death, regardless of causality, in the combination lamivudine plus zidovudine containing regimens as compared to the zidovudine containing regimens alone (p = 0.0007); HR = 0.399 (95% CI 0.230-0.693) or a 60% reduction in risk.
The data showed there was a significant reduction in progression to the combined endpoint of a new AIDS event or death for patients who received lamivudine in combination with zidovudine containing regimens compared to patients maintained on zidovudine containing regimens alone (p < 0.0001). The Hazard Ratio (HR) was 0.427 (95% confidence interval 0.318-0.572), or a 57% reduction in risk. In addition, the data indicated a significant reduction in death, regardless of causality, in the combination lamivudine plus zidovudine containing regimens as compared to the zidovudine containing regimens alone (p = 0.0007); HR = 0.399 (95% CI 0.230-0.693) or a 60% reduction in risk.
