What is in this leaflet
Please read this leaflet carefully before you take SEAZE tablets.
This leaflet answers some common questions about SEAZE. It does not contain all of the available information.
It does not take the place of talking to your doctor or pharmacist.
All medicines have benefits and risks. Your doctor has weighed the expected benefits of you taking SEAZE tablets against the risks this medicine could have for you.
If you have any concerns about taking this medicine, talk to your doctor or pharmacist.
Keep this leaflet with your medicine.
You may need to read it again.
What SEAZE is used for
Lamotrigine (the active ingredient in SEAZE tablets) belongs to a group of medicines called “anti-epileptic drugs”.
SEAZE tablets are used to treat epilepsy in adults and children. Usually SEAZE tablets are initially used in addition to other medicines for the treatment of epilepsy. SEAZE is used in partial or generalised seizures including Lennox-Gastaut Syndrome.
An epileptic seizure, fit or turn results when abnormal electrical impulses occur in nerve cells in the brain. These abnormal electrical impulses are believed to be due to altered levels of some chemicals in the brain.
It is thought to work by changing the levels of some of the chemicals associated with seizures.
Ask your doctor if you have any questions about why SEAZE has been prescribed for you.
Your doctor may have prescribed it for another reason.
SEAZE is available only with a doctor's prescription.
There is no evidence that it is addictive.
Before you take it
When you must not take it
Do not take SEAZE if you are allergic to medicines containing lamotrigine or any of the ingredients listed at the end of this leaflet.
Some of the symptoms of an allergic reaction may include skin rash, itching or hives; swelling of the face, lips or tongue which may cause difficulty in swallowing or breathing; wheezing or shortness of breath.
Do not take SEAZE if the expiry date (Exp.) printed on the pack has passed.
Do not take SEAZE if the packaging shows signs of tampering or the tablets do not look quite right.
Before you start to take it
Tell your doctor if:
- you are allergic to any other medicines, foods, dyes or preservatives
- you have any medical conditions, especially liver or kidney disorders
- you are taking any other medications for epilepsy.
This is particularly important for tablets containing sodium valproate. - you have ever developed meningitis after taking lamotrigine
- you are taking any form of hormonal contraceptive (e.g. “the pill”) or HRT
- you are breastfeeding, pregnant or trying to become pregnant.
Your doctor will discuss the risks and benefits of using SEAZE tablets if you are breastfeeding, pregnant or intending to become pregnant, including the risk to mother and foetus of uncontrolled epilepsy, when deciding on treatment options.
If you have not told your doctor about any of the above, tell them before you start taking SEAZE.
Taking other medicines
Tell your doctor if you are taking any medicines that you buy without a prescription from a pharmacy, supermarket or health food shop.
Some medicines may be affected by SEAZE, or may affect how well it works. Your doctor can tell you what to do if you are taking any of these medicines.
Your doctor and pharmacist have more information on medicines to be careful with or avoid while taking SEAZE.
How to take it
Taking SEAZE for the first time
You may notice that you feel dizzy, tired or unsteady in the first few weeks of treatment with SEAZE tablets. During this period you may also notice that you have slight problems with your vision. As your reactions may be slower during this period you should not operate any machinery or appliances and you should not drive a car. If any of these effects do not go away or are troublesome you should see your doctor.
If you develop any skin rash (e.g. spots or hives) during SEAZE treatment contact your doctor immediately.
There are reports of skin rash associated with SEAZE treatment. Some of these may be serious and cause severe illness.
Ask your doctor or pharmacist if you have any questions about taking SEAZE tablets.
How much to take
Take SEAZE tablets exactly as directed by your doctor or pharmacist.
Never change the dose yourself. Do not increase the dose more quickly than you have been told.
It is usual for the dose of SEAZE tablets to start at quite a low level and be slowly increased during the first few weeks of treatment. The doses that your doctor prescribes will generally depend on any other anti-epileptic medications you are taking and your response to SEAZE tablets.
If you start or stop taking hormonal contraceptives (e.g. “the pill”) while taking SEAZE, your doctor may need to adjust the dose of SEAZE depending on how well your condition is being treated.
You should tell your doctor if there are any changes in your menstrual pattern, such as breakthrough bleeding.
Your doctor may need to change the dose of SEAZE during your pregnancy.
Ask your doctor or pharmacist if there is something that you do not understand.
How long to take it
Do not stop taking SEAZE tablets or change the dose without first checking with your doctor.
Use in children
Children's weight should be checked and the dose reviewed as weight changes occur.
How to take it
SEAZE tablets may be swallowed whole, chewed or dispersed in a small volume of water (at least enough to cover the whole tablet).
If you forget to take SEAZE
If it is almost time for your next dose, skip the dose you missed and take your next dose when you are meant to.
Otherwise, take the missed dose as soon as you remember, and then go back to taking your tablets as you would normally.
Do not take a double dose to make up for the dose you missed.
If you are not sure what to do, ask your doctor or pharmacist.
If you take too much SEAZE (overdose)
Immediately telephone your doctor or the Poisons Information Centre (telephone 13 11 26) for advice, or go to the Accident and Emergency Department at the nearest hospital if you think you or anyone else may have taken too many SEAZE tablets. Do this even if there are no signs of discomfort or poisoning.
You may need urgent medical attention.
Symptoms of overdose may include nausea, vomiting, tiredness, drowsiness, impaired consciousness, twitching, increased seizures and blurred vision.
While you are taking it
Things you must do
Contact your doctor immediately if you develop any skin rash, like spots or hives, during SEAZE treatment.
There are reports of skin rash associated with SEAZE that may need hospital treatment or drug withdrawal; rarely serious skin rash may cause death.
Tell all the doctors, dentists and pharmacists who are treating you that you are taking SEAZE.
Tell your doctor or pharmacist that you are taking SEAZE tablets before starting any new medicine.
SEAZE may interfere with some laboratory tests to detect other drugs. If you require a laboratory test, tell your doctor or hospital that you are taking SEAZE.
Tell your doctor immediately if you become pregnant or are breastfeeding while taking SEAZE.
Your doctor will discuss the risks and benefits of taking this medicine.
Tell your doctor if, for any reason, you have not taken your medicine exactly as prescribed.
Otherwise, your doctor may think that SEAZE is not effective and change your dosage unnecessarily.
Things you must not do
Do not stop taking SEAZE, even if you feel better, or change the dose without first checking with your doctor.
Stopping this medicine suddenly may cause your epilepsy to come back or be worse. This is known as “rebound seizures”. Your doctor will advise you if you need to stop taking SEAZE and how to do it gradually.
Do not use it to treat any other conditions unless your doctor tells you to.
Do not give SEAZE to anyone else, even if they have the same condition as you.
Things to be careful of
Be careful driving or operating machinery until you know how SEAZE affects you.
As with other anti-epileptic medicines, SEAZE may cause drowsiness or dizziness and affect alertness in some people, especially after the first dose. Make sure you know how you react to it before you drive a car, operate machinery or do anything else that could be dangerous if you are dizzy or light-headed. If this occurs do not drive. If you drink alcohol, dizziness or light-headedness may be worse.
Children should not ride a bike, climb trees or do anything else that could be dangerous if they are feeling dizzy or sleepy.
Side effects
Check with your doctor as soon as possible if you think you are experiencing any side effects or allergic reactions due to taking SEAZE tablets, even if the problem is not listed below.
Like other medicines, SEAZE tablets can cause some side effects. If they occur, they are most likely to be minor and temporary. However, some may be serious and need medical attention.
Ask your doctor or pharmacist to answer any questions you may have.
Tell your doctor if you notice any of the following common side effects and they worry you:
- rash
- dizziness, unsteadiness, tremor
- headache
- drowsiness, tiredness or feeling sleep
- nausea, vomiting
- feeling weak
- blurred or double vision
- problems sleeping
- depression
- loss of memory
- confusion, agitation
- irritability, aggression
- increased activity in children
- joint or back pain
- for women, menstrual changes.
In general, these side effects usually only occur during the first few weeks of treatment with SEAZE.
Tell your doctor immediately if you notice any of the following:
- any skin reaction such as severe rash or hives
- swelling of the face, lips or tongue
- sore mouth or sore eyes
- a high temperature or fever
- swollen glands
- drowsiness
- unusual bleeding or bruising more easily than normal
- yellowing of the skin (jaundice).
A rare side effect is “Lupus-like reactions” which may present as a collection of symptoms consisting of fever, pain in the joints and general ill-health.
These are all serious side effects and may need urgent medical attention or hospitalisation.
Serious side effects are rare.
A very rare side effect is meningitis which may present as a group of symptoms consisting of fever, nausea, vomiting, headache, stiff neck and extreme sensitivity to bright light.
Tell your doctor immediately or go to the Accident and Emergency department of your nearest hospital if you:
- or anyone you know have any thoughts of self-harm or committing suicide. Patients and caregivers of children who are taking SEAZE should be watchful for any warning signs associated with suicide.
- think you are having an allergic reaction. Symptoms of an allergic reaction may include wheezing, difficulty breathing, swelling of the lips or mouth, hay fever, lumpy rash or hives or fainting.
Tell your doctor if you notice anything else that is making you feel unwell.
Other side effects not listed above may also occur in some patients.
Do not be alarmed by this list of possible side effects.
You may not experience any of them.
After taking it
Storage
Keep SEAZE where children cannot reach it.
A locked cupboard at least one-and-a-half metres above the ground is a good place to store medicines.
Keep your tablets in the pack until it is time to take them.
If you take the tablets out of the pack they may not keep well.
Keep your tablets in a cool dry place, protected from light and moisture, where the temperature stays below 25°C.
Do not store this medicine in the bathroom or near a sink. Do not leave it in the car or on window sills.
Heat and dampness can destroy some medicines.
Disposal
If your doctor tells you to stop taking SEAZE or your tablets have passed their expiry date, return any unused or expired medicine to your pharmacist.
Product description
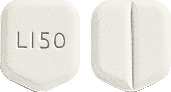
What it looks like
SEAZE tablets come in 4 strengths. Available in blister packs of 56 tablets.
- SEAZE 25 - white to off-white shield-shaped tablet, embossed with ‘L|25’ on one side and a scoreline on the other side.
- SEAZE 50 - white to off-white shield-shaped tablet, embossed with ‘L|50’ on one side and a scoreline on the other side.
- SEAZE 100 - white to off-white shield-shaped tablet, embossed with ‘L|100’ on one side and a scoreline on the other side.
- SEAZE 200 - white to off-white shield-shaped tablet, embossed with ‘L|200’ on one side and a scoreline on the other side.
Ingredients
The active ingredient in SEAZE is lamotrigine.
- each SEAZE 25 tablet contains 25 mg of lamotrigine
- each SEAZE 50 tablet contains 50 mg of lamotrigine
- each SEAZE 100 tablet contains 100 mg of lamotrigine
- each SEAZE 200 tablet contains 200 mg of lamotrigine.
The tablets also contain:
- mannitol
- cellulose-microcrystalline
- croscarmellose sodium
- silica-colloidal anhydrous
- povidone
- saccharin sodium
- talc-purified
- magnesium stearate
- blackcurrant flavour (1218806237).
The tablets are gluten free.
Sponsor
Aspen Pharma Pty Ltd
34-36 Chandos Street
St Leonards NSW 2065
Australia
Australian Registration Numbers:
SEAZE 25 - AUST R 99032
SEAZE 50 - AUST R 99037
SEAZE 100 - AUST R 99038
SEAZE 200 - AUST R 99039
This leaflet was prepared in June 2014.





 The relative risk for suicidal thoughts or behaviour was higher in clinical trials for epilepsy than in clinical trials for psychiatric or other conditions, but the absolute risk differences were similar for the epilepsy and psychiatric indications.
The relative risk for suicidal thoughts or behaviour was higher in clinical trials for epilepsy than in clinical trials for psychiatric or other conditions, but the absolute risk differences were similar for the epilepsy and psychiatric indications. Approximately 96% of a given dose of lamotrigine is eliminated by conjugation metabolism mediated by glucuronyl transferases. Cytochrome P450 is not involved in the elimination of lamotrigine to any significant extent. Therefore, the likelihood that lamotrigine inhibits the elimination of drugs metabolised by cytochrome P450 is low.
Approximately 96% of a given dose of lamotrigine is eliminated by conjugation metabolism mediated by glucuronyl transferases. Cytochrome P450 is not involved in the elimination of lamotrigine to any significant extent. Therefore, the likelihood that lamotrigine inhibits the elimination of drugs metabolised by cytochrome P450 is low. Irritability/ aggression, tiredness, drowsiness, agitation, confusion and hallucinations have also been reported. In children, hyperkinesia has been reported (5%). Very rarely, lupus-like reactions have been reported.
Irritability/ aggression, tiredness, drowsiness, agitation, confusion and hallucinations have also been reported. In children, hyperkinesia has been reported (5%). Very rarely, lupus-like reactions have been reported. Because of a risk of rash, the initial dose and subsequent dose escalation should not be exceeded (see Precautions).
Because of a risk of rash, the initial dose and subsequent dose escalation should not be exceeded (see Precautions).