What is in this leaflet
This leaflet answers some common questions about Sertraline AN.
It does not contain all the available information.
It does not take the place of talking to your doctor or pharmacist.
All medicines have risks and benefits.
Your doctor has weighed the risks of you taking Sertraline AN against the benefits it is expected to have for you.
If you have any concerns about taking this medicine, ask your doctor or pharmacist.
Keep this leaflet with the medicine.
You may need to read it again.
What Sertraline AN is used for
Sertraline AN is used to treat depression and conditions called obsessive compulsive disorder (OCD), panic disorder, social phobia (social anxiety disorder) and premenstrual dysphoric disorder (PMDD).
PMDD affects some women in the days before their period. PMDD is different from premenstrual syndrome (PMS). The mood symptoms (anger, sadness, tension, etc) in PMDD are more severe than in PMS and affect the woman's daily activities and relationships with others.
Sertraline AN belongs to a group of medicines called selective serotonin reuptake inhibitors (SSRIs). They are thought to work by blocking the uptake of a chemical called serotonin into nerve cells in the brain. Serotonin and other chemicals called amines are involved in controlling mood.
Your doctor, however, may have prescribed Sertraline AN for another purpose.
Ask your doctor if you have any questions about why Sertraline AN has been prescribed for you.
Sertraline AN should not be used in children and adolescents under the age of 18 years for the treatment of any medical condition other than obsessive compulsive disorder (OCD). The safety and efficacy of Sertraline AN for the treatment of medical conditions (other than OCD) in this age group has not been satisfactorily established.
For the treatment of OCD, Sertraline AN is not recommended for use in children under the age of 6, as the safety and efficacy in children of this age group has not been established.
This medicine is only available with a doctor's prescription.
There is no evidence that this medicine is addictive.
Before You Take Sertraline AN
When you must not take it:
Do not take Sertraline AN if you have an allergy to:
- any medicine containing sertraline
- any of the ingredients listed at the end of this leaflet.
Some of the symptoms of an allergic reaction may include:
- shortness of breath
- wheezing or difficulty breathing
- swelling of the face, lips, tongue or other parts of the body
- rash, itching or hives on the skin.
Do not take Sertraline AN if you have epilepsy not properly controlled by medication.
Do not take Sertraline AN if you are taking another medicine for depression called a monoamine oxidase inhibitor (MAOI) or have been taking it within the last 14 days.
Taking this medicine with a MAOI (e.g. Aurorix, Eldepryl, Nardil, Parnate) may cause a serious reaction with a sudden increase in body temperature, extremely high blood pressure and convulsions (fits).
Do not take Sertraline AN if you are taking phentermine (used to help weight loss), tryptophan (contained in protein-based foods or dietary proteins), methadone (used to treat drug addiction), medicines used to treat migraine, e.g. sumatriptan (Imigran), dextromethorphan (used as a cough suppressant in cold and 'flu medications), medicines used for pain management such as fentanyl, tapentadol (Palexia), tramadol or pethidine.
These medicines can cause an exaggerated response to Sertraline AN.
Do not take Sertraline AN if you are taking pimozide (used to treat disturbances in thinking, feeling and behaviour).
Ask your doctor or pharmacist if you are not sure if you have been taking one of these medicines.
Do not give Sertraline AN to children or adolescents under the age of 18 unless the doctor has prescribed it for the treatment of OCD. Do not give Sertraline AN to children under the age of 6 for the treatment of OCD.
If you are not sure whether you should be taking Sertraline AN, talk to your doctor.
Do not take Sertraline AN if:
- the expiry date marked on the packaging has passed, even though the tablets may look alright
- the packaging is torn or shows signs of tampering.
If it has expired or is damaged, return it to your pharmacist for disposal.
Before you start to take it:
Tell your doctor if you have any allergies to any foods, dyes, preservatives or any other medicines.
Tell your doctor if you have or have had any of the following medical conditions:
- any other mental illness
- epilepsy or seizures
- liver or kidney problems
- heart conditions causing irregular heartbeats
- a tendency to bleed more than normal
- diabetes mellitus
- glaucoma, an eye condition.
Tell your doctor if you are pregnant or intend to become pregnant.
There have been reports that babies exposed to Zoloft and other antidepressants during the third trimester of pregnancy may develop complications immediately after birth.
Tell your doctor if you are breastfeeding or wish to breastfeed.
Sertraline AN passes into breast milk and may affect your baby.
Your doctor will discuss the risks and benefits of taking Sertraline AN when pregnant or breastfeeding.
Taking other medicines
Tell your doctor or pharmacist if you are taking any other medicines, including:
- all prescription medicines
- all medicines, vitamins, herbal supplements or natural therapies you buy without a prescription from a pharmacy, supermarket, naturopath or health food shop.
Some medicines may be affected by Sertraline AN or may affect how well it works. You may need different amounts of your medicines, or you may need to take different medicines. Your doctor will advise you.
Tell your doctor or pharmacist if you are taking any of the following:
- other medicines for the treatment of depression called monoamine oxidase inhibitors (MAOIs).
Taking Sertraline AN with, or within 14 days of stopping a MAOI may cause a serious reaction with a sudden increase in body temperature, extremely high blood pressure and convulsions. - other MAOI drugs such as linezolid, an antibiotic used to treat pneumonia and certain skin infections
- other medicines for depression, panic disorder, social anxiety disorder or obsessive illnesses (e.g. Prothiaden, Prozac, Aropax, Luvox, Cipramil, Efexor-XR, Zoloft)
- lithium (e.g. Lithicarb), a medicine used to treat mood swings
- other medicines for PMDD (e.g. Prozac, Lovan, Zoloft)
- tryptophan (contained in protein based foods or dietary proteins)
- phentermine (weight-reducing medicines)
- dextromethorphan (used in cold and 'flu medicines to suppress cough)
- medicines for strong pain management such as fentanyl, tapentadol (Palexia), tramadol or pethidine
- methadone (used to treat drug addiction)
- other medicines used to relieve pain, swelling and other symptoms of inflammation, including arthritis (e.g. aspirin or NSAIDs such as ibuprofen or diclofenac)
- pimozide (used to treat disturbances in thinking, feeling and behaviour)
- St John's wort, a herbal remedy used to treat mood disorders
- medicines for treating psychotic illness such as clozapine, (e.g. Clozaril) which is used to treat schizophrenia
- medicines for irregular heartbeats (e.g. Tambocor)
- warfarin (e.g. Marevan, Coumadin) or other medicines that stop the blood from clotting
- phenytoin (e.g. Dilantin), a medicine used to treat epilepsy
- sumatriptan (e.g. Imigran), a medicine used to treat migraine
- diazepam or other medicines that act on the brain or nervous system (e.g. Serepax, Valium)
- cimetidine (e.g. Tagamet), a medicine used to treat reflux and ulcers
- antibiotics.
Not all brand names are given for the medicines listed above. Your doctor or pharmacist has more information on these medicines or other medicines to be careful with or avoid while taking Sertraline AN.
If you have not told your doctor or pharmacist about these things, tell them before you start taking Sertraline AN.
Some combinations of medicines may increase the risk of serious side effects and are potentially life threatening.
How to take Sertraline AN
Follow all directions given to you by your doctor and pharmacist carefully.
They may differ from the information contained in this leaflet.
If you do not understand the instructions on the packaging, ask your doctor or pharmacist for help.
How much to take
Your doctor will tell you how many tablets you need to take each day. This may depend on your age, your condition and whether or not you are taking any other medicines.
Depression - Adults
The usual starting dose is one 50 mg tablet each day. The dose can be increased gradually up to 200 mg a day if necessary.
Obsessive Compulsive Disorder - Children (6-12 Years)
The usual starting dose is 25 mg a day which is half a 50 mg tablet. Increase to one 50 mg tablet a day after one week.
Obsessive Compulsive Disorder -Adults and Adolescents (13-18 Years)
The usual starting dose is one 50 mg tablet each day.
Panic Disorder - Adults
The usual starting dose is 25 mg day which is half a 50 mg tablet. Increase to one 50 mg tablet a day after one week.
Social Phobia (Social Anxiety Disorder) - Adults
The usual starting dose is 25 mg a day which is half a 50 mg tablet. Increase to one 50 mg a day after one week. Do not take more than 200 mg a day for the conditions listed above.
Premenstrual Dysphoric Disorder (PMDD)
If taking throughout the menstrual cycle
The usual starting dose is one 50 mg tablet a day. This may be increased to a maximum of 150 mg a day if needed. Increase the dose in a step wise fashion. If you are unclear how to do this ask your pharmacist or doctor for advice.
If taking in the last 14 days of the menstrual cycle
The usual starting dose is one 50 mg tablet a day. This may be increased to a maximum of 100 mg a day.
Do not take more than the maximum doses recommended above for PMDD
How to take it
Swallow the tablets with a glass of water.
Try to take your tablet at the same time each day, either morning or evening.
Taking it at the same time each day will have the best effect. It will also help you remember when to take it.
It does not matter if you take this medicine before or after food.
How long to take it
Most medicines for depression and obsessive illnesses take time to work so do not be discouraged if you do not feel better straight away.
It may take 2 to 4 weeks or even longer to feel the full benefit of Sertraline AN.
Continue taking Sertraline AN until your doctor tells you to stop.
Even when you feel well, you may need to take Sertraline AN for several months or longer.
If you have PMDD, your doctor may ask you to take this medicine only at certain times of the month.
Do not stop taking Sertraline AN, or change the dose, without first checking with your doctor.
Occasionally the symptoms of depression or other psychiatric conditions may include thoughts of harming yourself or committing suicide. It is possible that these symptoms may continue or increase until the full anti-depressant effect of your medicine becomes apparent (i.e. one to two months).
You or anyone close to you or caring for you should watch for these symptoms and tell your doctor immediately or go to the nearest hospital if you have any distressing thoughts or experiences during this initial period or at any other time.
Contact your doctor if you experience any worsening of your depression or other symptoms at any time during your treatment.
If you forget to take it
Do not take a double dose to make up for the dose that you missed.
Wait until the next day and take your normal dose then.
If you are not sure what to do in this situation, ask your doctor or pharmacist.
If you have trouble remembering to take your medicine, ask your pharmacist for some hints.
In case of an overdose
Immediately telephone your doctor or Poisons Information Centre (telephone 13 11 26) for advice, or go to Accident and Emergency at your nearest hospital if you think you or anyone else may have taken too much Sertraline AN.
Do this even if there are no signs of discomfort or poisoning.
You may need urgent medical attention.
Symptoms of an overdose may include:
- feeling drowsy
- nausea, diarrhoea, vomiting
- fast or irregular heartbeats
- tremors
- feeling agitated or dizzy.
While you are taking Sertraline AN
Things you must do
Tell all doctors, dentists and pharmacists who are treating you that you are taking Sertraline AN.
Tell your doctor or pharmacist that you are taking Sertraline AN if you are about to be started on any new medicines.
Tell your doctor if you become pregnant while taking Sertraline AN.
If you are a woman of child-bearing age, you should avoid becoming pregnant while taking Sertraline AN.
Tell your doctor immediately if you have any suicidal thoughts or other mental/mood changes.
A worsening of depressive symptoms including thoughts of suicide or self-harm may occur in the first one or two months of you taking Sertraline AN or when the doctor changes your dose. These symptoms should subside when the full effect of Sertraline AN takes place.
Children, adolescents or young adults under 24 years of age are more likely to experience these effects during the first few months of treatment.
Patients and caregivers should be alert and monitor for these effects.
Signs and symptoms of suicide include:
- thoughts or talk of death or suicide
- thoughts or talk of self-harm or harm to others
- any recent attempts of suicide or self-harm
- increase in aggressive behaviour, irritability or agitation
- worsening of depression.
All mention of suicide or violence must be taken seriously.
If you or someone you know is demonstrating these warning signs of suicide while taking Sertraline AN, contact your doctor or a mental health professional right away.
Children should have regular check-ups with the doctor to monitor growth and development.
If you are going to have surgery, tell the surgeon or anaesthetist that you are taking this medicine.
It may interact with other medicines used during surgery and cause unwanted side effects.
If you are about to have any urine tests, tell your doctor that you are taking this medicine.
It may interfere with the results of some tests.
Things you must not do
Do not stop taking Sertraline AN, or change the dose, without first checking with your doctor.
Do not let yourself run out of tablets over the weekend or on holidays.
Suddenly stopping Sertraline AN may cause dizziness, light headedness, numbness, unusual tingling feelings or shakiness.
Do not give this medicine to anyone else, even if their symptoms seem similar to yours.
Do not take Sertraline AN to treat any other complaints unless your doctor says to.
Things to be careful of
Be careful driving or operating machinery until you know how Sertraline AN affects you.
Some medicines for depression may affect your ability to drive or operate machinery or do things that could be dangerous if you are not alert.
Although drinking moderate amounts of alcohol is unlikely to affect your response to Sertraline AN, your doctor may suggest avoiding alcohol while you are taking Sertraline AN.
If you are feeling drowsy or are uncoordinated, be careful that you do not fall over.
Sertraline AN, like other medicines in this class, may increase your risk of bone fracture.
You should wait at least 14 days after stopping Sertraline AN before starting any other medicines for depression or obsessive illnesses from the MAOI group, such as Aurorix, Eldepryl, Nardil, and Parnate.
All of the above precautions are important even after you have stopped taking Sertraline AN.
The effects of Sertraline AN may last for some days after you have stopped taking it.
Side Effects
Tell your doctor or pharmacist as soon as possible if you do not feel well while you are taking Sertraline AN.
All medicines can have side effects.
Sometimes they are serious, most of the time they are not. You may need medical attention if you get some of the side effects.
It can be difficult to tell whether side effects are the result of taking Sertraline AN, effects of your condition or side effects of other medicines you may be taking. For this reason it is important to tell your doctor of any change in your condition.
Do not be alarmed by the list of side effects.
You may not experience any of them.
Ask your doctor or pharmacist to answer any questions you may have.
Tell your doctor or pharmacist if you notice any of the following and they worry you:
- headache, dizziness, shakiness, muscle stiffness or weakness, decrease or loss of touch or other senses
- dry mouth, increased sweating, feeling sick, diarrhoea, indigestion, vomiting, stomach pain
- tiredness, hot flushes, fever, feeling unwell
- weight increase or loss
- sleeping difficulties, sexual problems, sleepiness
- vision disturbance
- menstrual irregularities
- difficulty in passing urine, or
- increased frequency
- unusually overactive
- shaking or tremors.
Tell your doctor as soon as possible if you notice any of the following:
- agitation, nervousness, anxiety, frightening dreams, yawning, abnormal thinking, teeth grinding, loss of appetite, impaired concentration
- symptoms of agitation, anxiety dizziness, headache, nausea and tingling or numbness of the hands and feet after stopping Sertraline AN
- uncontrollable muscle spasms affecting the eyes, head, neck and body
- uncontrollable movements of the body, shuffling walk
- palpitations, fainting or chest pain
- irregular heartbeats
- abnormal bleeding
- sudden onset of severe headache.
Tell your doctor immediately or go to Accident and Emergency at your nearest hospital, if you notice any of the following:
- fits or seizures
- signs of allergy such as rash or hives, swelling of the face, lips or tongue, wheezing or difficulty breathing
- symptoms of sudden fever with sweating, fast heartbeat and muscle stiffness, which may lead to loss of consciousness
- thoughts of suicide or attempting suicide or self-harm.
The above list includes very serious side effects. You may need urgent medical attention or hospitalisation.
Tell your doctor or pharmacist if you notice anything else that is making you feel unwell.
Other side effects not listed above may also occur in some people.
Some of these side effects (e.g. changes in thyroid function, liver function or glucose control) can only be found when your doctor does tests from time to time to check your progress.
After taking Sertraline AN
Storage
Keep your tablets where young children cannot reach them.
A locked cupboard at least 1 and a half metres above the ground is a good place to store medicines.
Keep Sertraline AN in a cool, dry place where the temperature stays below 30°C.
Do not store it or any other medicine in the bathroom or near a sink. Do not leave it in the car or on window sills.
Heat and dampness can destroy some medicines.
Keep your tablets in their blister pack until it is time to take them.
Disposal
If your doctor tells you to stop taking Sertraline AN, or the tablets have passed their expiry date, ask your pharmacist what to do with any left over.
Product description
What it looks like
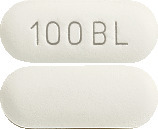
Sertraline AN tablets come in two strengths:
- Sertraline AN 50 mg (AUST R 195315) - White to off-white, capsule shaped, biconvex film coated tablets with '50' and 'BL' embossed on either side of the breakline
- Sertraline AN 100 mg (AUST R 195326) - White to off-white, capsule shaped, biconvex film coated tablets with '100' and 'BL' embossed on one side.
Ingredients
Active ingredient:
Sertraline hydrochloride
Inactive ingredients
- microcrystalline cellulose
- calcium hydrogen phosphate
- hydroxypropyl cellulose
- hydromellose
- Macrogol 400
- Polysorbate 80
- sodium starch glycollate
- magnesium stearate
- Titanium oxide
Sertraline AN does not contain gluten, lactose or sugar.
Sertraline AN is presented in PVC-Alu blisters containing 30 tablets.
Sponsor
Amneal Pharma Australia Pty Ltd
12 River Street
South Yarra
VIC – 3141
Australia
This leaflet was prepared in October 2014.
Doc ID: 110.AN.M.1.0