SUMMARY CMI
VZOLE
Consumer Medicine Information (CMI) summary
The full CMI on the next page has more details. If you are worried about using this medicine, speak to your doctor or pharmacist.
1. Why am I using VZOLE?
VZOLE contains the active ingredient voriconazole. VZOLE is used to treat fungal and yeast infections.
For more information, see Section 1. Why am I using VZOLE? in the full CMI.
2. What should I know before I use VZOLE?
Do not use if you have ever had an allergic reaction to voriconazole, any similar medicines, or any of the ingredients listed at the end of the CMI.
Talk to your doctor if you have any other medical conditions, take any other medicines, or are pregnant or plan to become pregnant, or are breastfeeding. VZOLE should NOT be used during pregnancy or breastfeeding, unless indicated by your doctor. Effective contraception should be used in women of childbearing potential.
For more information, see Section 2. What should I know before I use VZOLE? in the full CMI.
3. What if I am taking other medicines?
Some medicines may interfere with VZOLE and affect how it works.
A list of these medicines is in Section 3. What if I am taking other medicines? in the full CMI.
4. How do I use VZOLE?
- Your doctor will prescribe the amount required of VZOLE based on your weight. The dose will be based on the form being prescribed.
- More instructions can be found in Section 4. How do I use VZOLE? in the full CMI.
5. What should I know while using VZOLE?
| Things you should do |
|
| Things you should not do |
|
| Driving or using machines |
|
| Looking after your medicine |
|
For more information, see Section 5. What should I know while using VZOLE? in the full CMI.
6. Are there any side effects?
Common side effects maybe headache, nausea or rash. More serious side effects maybe sudden skin symptoms or changes, allergic reaction, changes to urine colour or seizures.
For more information, including what to do if you have any side effects, see Section 6. Are there any side effects? in the full CMI.
FULL CMI
VZOLE
Active ingredient(s): VORICONAZOLE (vori-con-a-zole)
Consumer Medicine Information (CMI)
This leaflet provides important information about using VZOLE. You should also speak to your doctor or pharmacist if you would like further information or if you have any concerns or questions about using VZOLE.
Where to find information in this leaflet:
1. Why am I using VZOLE?
2. What should I know before I use VZOLE?
3. What if I am taking other medicines?
4. How do I use VZOLE?
5. What should I know while using VZOLE?
6. Are there any side effects?
7. Product details
1. Why am I using VZOLE?
VZOLE contains the active ingredient voriconazole.
VZOLE belongs to a group of medicines called triazole antifungals.
This medicine works by preventing the growth of fungal and yeast organisms causing your infection.
VZOLE is used to treat fungal and yeast infections such as:
- invasive aspergillosis (as-pur-ji-losis), a fungal infection caused by a fungus called Aspergillus (as-pur-jilus), which usually begins in the respiratory tract (in the nose, sinuses or lungs). Aspergillus is harmless in most healthy people; however, in people with poor immune systems (such as people who have had organ transplants and people with cancer or HIV/AIDS) invasive aspergillosis can be serious and spread to other tissues and organs.
- serious Candida (can-did-da) infections, including Candida infections of the oesophagus (food pipe or gullet) and those that have spread into the blood stream or to other parts of the body.
- serious fungal infections caused by Scedosporium (ski-doe-spore-rium) species and Fusarium (few-saa-rium) species.
- other serious fungal infections in patients who do not respond to, or cannot tolerate, other antifungal medicines.
VZOLE is also used to prevent invasive fungal infections in patients who are at risk of developing such infections.
2. What should I know before I use VZOLE?
Warnings
Do not use VZOLE if:
- you are allergic to voriconazole, any similar medicines, or any of the ingredients listed at the end of this leaflet.
Symptoms of an allergic reaction may include shortness of breath, wheezing or difficulty breathing; swelling of the face, lips, tongue or other parts of the body; skin rash, itching or hives.
- Always check the ingredients to make sure you can use this medicine.
- Do not use VZOLE if you are taking any of the following medicines:
- Medicines to treat mental illness:
- pimozide, a medicine used to treat mental illness.
- St John's Wort (a herbal medicine).
- lurasidone, a medicine to treat schizophrenia and bipolar disorder. - Medicines used to manage heart health
- quinidine, a medicine used to treat irregular heartbeat.
- ivabradine, a medicine used to treat heart problems. - Medicines used to treat infections
- rifampicin, a medicine used to treat tuberculosis and other infections.
- rifabutin an antibiotic.
- efavirenz (e.g., Stocrin) (a medicine used to treat HIV infection) in doses of 400 mg or more once a day.
- ritonavir (a medicine used to treat HIV infection) in doses of 400 mg or more twice a day. - Medicines used for seizures, insomnia or migraines
- carbamazepine, a medicine used to treat seizures.
- long-acting barbiturates such as phenobarbitone, medicines used to treat severe insomnia and seizures.
- ergotamine or dihydroergotamine, medicines used to treat migraine. - Other medicines:
- sirolimus, a medicine used in transplant patients.
- naloxegol, a medicine used to treat constipation caused by opioids (narcotic pain medicines).
- tolvaptan used to treat low levels of sodium in your blood or for kidney problems).
- venetoclax, a medicine used to treat blood cancers.
- Lemborexant, a medicine used to help manage insomnia
VZOLE should not be given to a child under the age of 2 years. Safety and effectiveness in children younger than 2 years has not been established.
Do not use this medicine after the expiry date printed on the pack or if the packaging is torn or shows signs of tampering. If it has expired or is damaged, return it to your pharmacist for disposal.
Check with your doctor if you:
- have any other medical conditions, including:
- heart problems.
- any problems affecting your kidneys.
- any problems affecting your liver. If you have liver disease your doctor may prescribe a lower dose.
- recent chemotherapy or stem cell transplant.
- take any medicines for any other condition - have allergies to foods, preservatives or dyes or any other medicines, especially antifungal medicines such as itraconazole, fluconazole, posaconazole or ketoconazole.
During treatment, you may be at risk of developing certain side effects. It is important you understand these risks and how to monitor for them. See additional information under Section 6. Are there any side effects?
Pregnancy and breastfeeding
Check with your doctor if you are pregnant or intend to become pregnant.
VZOLE should not be used during pregnancy, unless indicated by your doctor. Effective contraception should be used in women of childbearing potential. Your doctor can discuss with you the risks and benefits involved.
Talk to your doctor if you are breastfeeding or intend to breastfeed.
VZOLE should not be used whilst breastfeeding, unless indicated by your doctor. It is not known if the active ingredient voriconazole passes into breast milk. Your doctor can discuss with you the risks and benefits involved.
3. What if I am taking other medicines?
Tell your doctor or pharmacist if you are taking any other medicines, including any medicines, vitamins or supplements that you buy without a prescription from your pharmacy, supermarket or health food shop.
Some medicines should NOT be taken with VZOLE. Please see Section 2 above for a list of those medicines.
Some medicines and VZOLE may interfere with each other. These include (not all brands given):
- Medicines used to treat infections
- fluconazole, a medicine used to treat fungal infections.
- flucloxacillin, a medicine used to treat bacterial infections.
- indinavir and some other medicines used to treat HIV infection. - Medicines used for cancer treatment:
- everolimus, a medicine used to treat cancer
- other cancer drugs such as glasdegib, axitinib, bosutinib, cabozantinib, ceritinib, cobimetinib, dabrafenib, dasatinib, nilotinib, sunitinib, ibrutinib, ribociclib, sunitinib.
- tretinoin, a medicine used for the treatment of acne and acute promyelocytic leukemia.
- Vincristine, vinblastine or vinorelbine, medicines used in treating cancer. - Medicines used in management of organ transplant:
- ciclosporin, a medicine used to prevent organ transplant rejection or to treat certain problems with the immune system.
- tacrolimus, a medicine used in patients who have had a liver or kidney transplant.
- letermovir used to prevent viral infections after bone marrow transplant). - Medicines for management of diabetes and other heart-related conditions:
- warfarin, a medicine used to stop blood clots.
- sulphonylureas, medicines used to treat diabetes such as glibenclamide, gliclazide and glipizide.
- statins, medicines used for lowering cholesterol. - Medicines for management of mental health
- benzodiazepines, medicines used to treat insomnia or anxiety.
- eszopiclone, a medicine used to treat insomnia. - Medicines used for pain management:
- strong pain killers such as alfentanil, fentanyl and oxycodone.
- non-steroidal anti-inflammatory drugs, medicines used to treat pain and inflammation such as ibuprofen and diclofenac. - Other medicines:
- ivacaftor, a medicine used to treat cystic fibrosis.
- phenytoin, a medicine used to treat epilepsy. osome antihistamines, medicines used to treat hayfever, allergic skin reactions, itching.
- theophylline, a medicine used to treat asthma.
- omeprazole, a medicine used to treat indigestion, reflux and stomach or duodenal ulcers.
- methadone (used to treat heroin addiction).
- oral contraceptives (the Pill). - methotrexate, a medicine used to treat arthritis and cancers.
These medicines may be affected by VZOLE or may affect how well it works. You may need different amounts of your medicines or you may need to take different medicines.
Check with your doctor or pharmacist if you are not sure about what medicines, vitamins or supplements you are taking and if these affect VZOLE.
4. How do I use VZOLE?
How much to take / use
Your doctor will tell you how much to take depending on your weight.
Adults
Treatment of invasive fungal infections
The usual dose of VZOLE tablets in adults weighing 40 kg and greater is 400 mg (two 200 mg tablets twice a day) for the first day and then 200 mg to 300 mg twice a day thereafter.
Prevention of invasive fungal infections.
The usual dose in adults weighing 40 kg and greater is one 200 mg tablet twice a day.
In adults weighing less than 40 kg the dose of VZOLE tablets is halved.
Children
VZOLE should not be given to a child under the age of 2 years.
Your doctor will determine the dose of VZOLE required for your child.
Depending on how serious the infection is and how your child reacts to the medicine, your doctor may increase or decrease the dose.
Oral voriconazole should be administered to these patients unless an assessment of the risk to the patient justifies the use of intravenous voriconazole.
Adolescents (12-16 years of age)
Adolescents aged 12-16 years of age are usually given the same dose as adults.
How to take / use VZOLE
Swallow the tablets whole with a full glass of water.
Take VZOLE tablets at least one hour before or one hour after a meal.
VZOLE needs to be taken regularly to be effective.
When to take / use VZOLE
- Take your medicine at about the same time each day.
- Taking it at the same time each day will have the best effect. It will also help you remember when to take it.
- Take your medicine 1 hour before food after a meal.
How long to take it
- The length of time you take VZOLE will depend on the type of infection you have.
- If you have a weakened immune system or a difficult infection, you may need long-term treatment to prevent the infection from returning.
- Continue taking VZOLE for as long as your doctor or pharmacist recommends. Do not stop taking VZOLE because you are feeling better.
- If you do not complete the full course prescribed by your doctor, the infection may not clear completely or your symptoms may return.
If you forget to take VZOLE
If it is almost time for your next dose, skip the dose you missed and take your next dose when you are meant to.
Do not take a double dose to make up for the dose you missed.
This may increase the chance of you getting an unwanted side effect.
If you are not sure what to do, ask your doctor or pharmacist.
However, tell your doctor or pharmacist if you think that a dose has been forgotten.
If you take too much VZOLE
If you think that you have taken too much VZOLE, you may need urgent medical attention.
You should immediately:
- phone the Poisons Information Centre (by calling 13 11 26), or
- contact your doctor, or
- go to the Emergency Department at your nearest hospital.
You should do this even if there are no signs of discomfort or poisoning.
Symptoms of an overdose may include upset stomach, diarrhoea, headache and sensitivity to light.
5. What should I know while using VZOLE?
Things you should do
- If you are going to have surgery, tell the surgeon or anaesthetist that you are taking this medicine. It may affect other medicines used during surgery.
- Avoid going out in the sun for long periods of time while you are taking VZOLE. VZOLE can cause sensitivity to sunlight.
- Make sure you follow your doctor's instructions and keep all appointments, including blood tests.
Your doctor should monitor the function of your liver and kidneys using blood tests. If you have liver disease, your doctor might lower your dose of VZOLE or stop your VZOLE treatment. Your doctor might also monitor the function of your pancreas. - If you are about to have any blood tests, tell your doctor that you are taking this medicine.
It may interfere with the results of some tests.
Call your doctor straight away if you:
- notice any changes to your skin while you are taking VZOLE.
- develop a rash or blisters while taking VZOLE. If this rash worsens, VZOLE may need to be stopped.
- suffer from chronic, or long-lasting fatigue, muscle weakness, loss of appetite, weight loss or abdominal pain while on VZOLE.
- notice the symptoms of your infection do not improve within a few days, or if they become worse, tell your doctor.
- become pregnant while taking VZOLE, tell your doctor immediately. If you are a woman of child-bearing age, you should avoid becoming pregnant while taking VZOLE.
Remind any doctor or dentist you visit that you are using VZOLE.
Things you should not do
- Do not stop taking your medicine or lower the dosage without checking with your doctor.
- If you do not complete the full course prescribed by your doctor, the infection may not clear completely or your symptoms may return
- Do not use VZOLE to treat any other complaints unless your doctor tells you to.
- Do not give your medicine to anyone else even if they have the same condition as you or if their symptoms seem similar to yours.
Driving or using machines
Be careful before you drive or use any machines or tools until you know how VZOLE affects you.
You may experience changes to your vision, such as blurriness, colour changes or uncomfortable sensitivity to light.
If you have any of these symptoms, do not drive, operate machinery or do anything else that could be dangerous. Do not drive at night.
Children should be careful when riding bicycles or climbing.
Drinking alcohol
Tell your doctor if you drink alcohol.
Looking after your medicine
Store it in a cool dry place away from moisture, heat or sunlight; for example, do not store it:
- in the bathroom or near a sink, or
- in the car or on window sills.
Keep your tablets in the pack until it is time to take them.
If you take the tablets out of the blister pack, they may not keep well.
Keep your tablets in a cool dry place where the temperature stays below 30°C.
Do not use this medicine after the expiry date.
Keep it where young children cannot reach it.
Getting rid of any unwanted medicine
If you no longer need to use this medicine or it is out of date, take it to any pharmacy for safe disposal.
6. Are there any side effects?
All medicines can have side effects. If you do experience any side effects, most of them are minor and temporary. However, some side effects may need medical attention.
See the information below and, if you need to, ask your doctor or pharmacist if you have any further questions about side effects.
Less serious side effects
| Less serious side effects | What to do |
Symptoms at injection site:
| Speak to your doctor if you have any of these less serious side effects and they worry you. |
Serious side effects
| Serious side effects | What to do |
Skin changes:
| Call your doctor straight away, or go straight to the Emergency Department at your nearest hospital if you notice any of these serious side effects. |
Tell your doctor or pharmacist if you notice anything else that may be making you feel unwell.
Other side effects not listed here may occur in some people.
Reporting side effects
After you have received medical advice for any side effects you experience, you can report side effects to the Therapeutic Goods Administration online at www.tga.gov.au/reporting-problems. By reporting side effects, you can help provide more information on the safety of this medicine.
Always make sure you speak to your doctor or pharmacist before you decide to stop taking any of your medicines.
7. Product details
This medicine is only available with a doctor's prescription.
What VZOLE contains
| Active ingredient (main ingredient) |
|
| Other ingredients (inactive ingredients) |
|
| Potential allergens | This medicine contains sugars as lactose. |
Do not take this medicine if you are allergic to any of these ingredients.
What VZOLE looks like
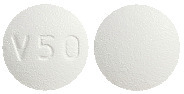
VZOLE tablets come in two strengths, 50 mg and 200 mg.
VZOLE 50 mg tablets are white, round, biconvex, film coated tablets with ‘V50’ debossed on one side and plain on other side.
- VZOLE 50 mg blister pack - AUST R 238239
- VZOLE 50 mg bottle - AUST R 238240
VZOLE 200 mg tablets are white, caplet shaped, film coated tablets with ‘V200’ debossed on one side and plain on other side.
- VZOLE 200 mg blister pack - AUST R 238242
- VZOLE 200 mg bottle - AUST R 238241
Who distributes VZOLE
Arrotex Pharmaceuticals Pty Ltd
15-17 Chapel Street
Cremorne VIC 3121
This leaflet was prepared in February 2024
Published by MIMS March 2024


 Dosage recommendations for other indications are provided in Tables 2 and 3.
Dosage recommendations for other indications are provided in Tables 2 and 3.


 See Table 6.
See Table 6.


 The results of this comparative trial confirmed the results of an earlier trial in the primary treatment of patients with acute invasive aspergillosis (study 304). In this study, an overall success rate of 54% was seen in patients treated with voriconazole.
The results of this comparative trial confirmed the results of an earlier trial in the primary treatment of patients with acute invasive aspergillosis (study 304). In this study, an overall success rate of 54% was seen in patients treated with voriconazole.


