What is in this leaflet
This leaflet answers some common questions about ZAVESCA.
It does not contain all the available information.
It does not take the place of talking to your doctor or pharmacist.
All medicines have risks and benefits. Your doctor has weighed the risks of you taking ZAVESCA against the benefits he/she expects it will have for you.
If you have any concerns about taking this medicine, ask your doctor or pharmacist.
Keep this leaflet with the medicine. You may need to read it again.
What ZAVESCA is used for
ZAVESCA is a medicine that is used to treat mild to moderate Type 1 Gaucher disease in adults and it is also used to treat Niemann-Pick type C (NP-C) disease in children, adolescents and adults.
Type 1 Gaucher disease is an inherited disease that you get from both of your parents. People with Type 1 Gaucher disease are partially missing an enzyme that breaks down a chemical in the body called glucosylceramide. Too much glucosylceramide causes an increase in the size of the liver and spleen. It also causes bone disease and changes in the blood.
ZAVESCA reduces the formation of glucosylceramide to a level the partially missing enzyme can cope with.
You may be prescribed ZAVESCA if your doctor decides other treatments for this disease are not right for you.
Niemann-Pick disease is an inherited disease that you get from both parents. If you have NP-C, fats (glycosphingolipids) build up in the cells of your brain. This can result in disturbances in neurological functions such as eye movements, balance, swallowing, and memory, and in seizures.
ZAVESCA works by inhibiting the enzyme called ‘glucosylceramide synthase’ which is responsible for the first step in the synthesis of most glycosphingolipids.
Your doctor may have prescribed ZAVESCA for another reason. Ask your doctor if you have any questions about why ZAVESCA has been prescribed for you.
Before you take ZAVESCA
When you must not take it
Do not take ZAVESCA if you are allergic to miglustat or any of the ingredients listed at the end of this leaflet.
Do not take ZAVESCA if you are pregnant or planning to become pregnant. ZAVESCA may harm your baby. You must use effective birth control while you are taking ZAVESCA.
Do not take ZAVESCA if you are breastfeeding. It is not known if this medicine passes into breast milk and if it can harm your baby.
ZAVESCA may harm sperm. All men should use effective birth control while taking this medicine and for 3 months after they stop taking it.
Do not take ZAVESCA if you suffer from severe kidney disease.
Do not take it after the expiry date (EXP) printed on the pack. If you take this medicine after the expiry date has passed it may not work as well.
Do not take it if the packaging is torn or shows signs of tampering.
Before you start to take it
Tell your doctor if you are pregnant or planning to become pregnant.
Tell your doctor if you are breastfeeding or are planning to breastfeed.
Tell your doctor if you have or have had any medical conditions especially the following:
- kidney disease
- liver disease
If you have not told your doctor about any of the above, tell them before you take ZAVESCA.
Your doctor may perform the following tests before treatment and during treatment with ZAVESCA:
- an examination to check the nerves in your arms and legs
- a test of your memory and thinking ability
- blood test to check your platelet count
- measurement of vitamin B12 levels (for GD-1 only)
- if you are a child or adolescent with NP-C your doctor will also check measurements of your growth
The reason these tests are done is that some patients have had tingling or numbness in the hands and feet, or memory and thinking problems, while taking ZAVESCA. The tests will help your doctor decide whether these effects are due to existing conditions, or due to side effects of ZAVESCA.
Taking other medicines
Tell your doctor if you are taking any other medicines including any that you buy without a prescription from your pharmacy, supermarket or health food shop. Some medicines may be affected by ZAVESCA or may affect how well it works.
Your doctor has more information on medicines to be careful with or to avoid while taking ZAVESCA.
How to take ZAVESCA
Always take ZAVESCA exactly as your doctor has instructed you to do. You should check with your doctor or pharmacist if you are unsure.
How much to take
Type 1 Gaucher disease
The usual dose for adults is one capsule (100 mg) three times a day (morning, afternoon and evening).
Niemann-Pick type C disease
The usual dose for adults and adolescents is two capsules (200 mg) three times a day (morning, afternoon and evening).
For children under the age of 12 years, the dose is determined by body surface area (BSA m2); your doctor will work this out for you.
If you have a problem with your kidneys you may receive a lower starting dose.
How to take it
ZAVESCA should be swallowed whole with water. It is recommended to take ZAVESCA without food.
When to take it
Take ZAVESCA at the same time(s) each day.
How long to take it
You must take ZAVESCA every day.
Continue taking the medicine for as long as your doctor tells you to.
Do not stop taking it unless your doctor tells you to even if you feel better.
If you forget to take it
If it is almost time for your next dose, skip the dose you missed and take your next dose when you are meant to.
Otherwise, take it as soon as you remember and then go back to taking it as you would normally.
Do not take a double dose to make up for the dose that you missed.
If you are not sure what to do, ask your doctor or pharmacist.
If you have trouble remembering when to take your medicine, ask your pharmacist for some tips.
If you take too much (overdose)
Immediately telephone your doctor, or the Poisons Information Centre or go to accident and emergency at you nearest hospital if you think you or anyone else may have taken too much ZAVESCA. Do this even if there are no signs of discomfort or poisoning.
Poison Information Centre telephone numbers:
- Australia: 13 11 26
- New Zealand: 0800 POISON or 0800 764 766
You may need urgent medical attention.
While you are taking ZAVESCA
Things you must do
Tell your doctor if you become pregnant while you are taking ZAVESCA.
Men and women should use effective birth control while taking ZAVESCA.
Men should keep using effective birth control for 3 months after treatment with ZAVESCA is stopped.
Tell all the doctors, dentists and pharmacists who are treating you that you are taking ZAVESCA.
If you have diarrhoea your doctor may ask you to change your diet to reduce your lactose and carbohydrate intake such as sucrose (cane sugar), or not to take ZAVESCA together with food, or to temporarily reduce your dose. In some cases, the doctor may prescribe anti-diarrhoeal medications such as loperamide. If your diarrhoea does not respond to these measures, or if you have any other abdominal complaint, consult your doctor. In such a case, your doctor may decide to conduct further investigations.
Keep all of your doctor or clinic appointments.
Your doctor may do certain tests, including blood tests, from time to time to make sure the medicine is working and to prevent unwanted side effects.
Things you must not do
Do not get pregnant while you are taking ZAVESCA.
Do not breast-feed while on ZAVESCA.
Do not give ZAVESCA to anyone else, even if they have the same condition as you.
Do not stop taking ZAVESCA or change your dose without checking with your doctor.
Things to be careful of
Be careful before you drive or use any machines or tools until you know how ZAVESCA affects you.
ZAVESCA may make you feel dizzy. Do not drive or operate any tools or machines if you feel dizzy.
Side effects
Tell your doctor or pharmacist as soon as possible if you do not feel well while you are taking ZAVESCA.
All medicines can have side effects. Sometimes they are serious, most of the time they are not. You may need medical treatment if you get some of the side effects.
Ask your doctor or pharmacist to answer any questions you may have.
Tell your doctor immediately if you notice any of the following:
- tremor usually in your hands. This often disappears without stopping ZAVESCA. Sometimes it may be necessary for your doctor to reduce your dose of ZAVESCA or stop ZAVESCA treatment to stop the tremor.
- tingling or numbness in your hands and feet
- memory or thinking problems
These could be side effects of ZAVESCA or they could be due to existing conditions. Your doctor will perform some tests before and during treatment with ZAVESCA to assess this.
Tell your doctor if you notice any of the following and they worry you:
- diarrhoea (sometimes with blood)
- constipation
- inability to control bowel movement
- frequent, abnormal urination
- stomach pain or discomfort, abdominal swelling or wind (flatulence)
- feeling sick (nausea)
- heartburn/ indigestion
- vomiting
- decreased or lack of appetite (anorexia)
- dry mouth and thirsty
- burping
- lactose intolerance
- dizziness
- headache or migraine
- weight loss
- low platelet count (thrombocytopenia) causing symptoms like easy or excessive bruising and bleeding
- low red blood cell (anaemia) causing symptoms like fatigue, weakness, pale skin
- abnormal blood test results
- muscle spasms or weakness
- loss of coordination of muscles (ataxia)
- reduced sensation to touch (hypoesthesia)
- difficulty in falling asleep (insomnia)
- tiredness (fatigue) or feeling of weakness
- increase in energy
- feeling anxious
- depression
- chills
- loss of strength (asthenia)
- joint or bone pain
- swelling spleen or liver causing symptoms like abdominal pain, tiredness, yellowing of the skin and the whites of the eyes
- rash
- chest pain
- blurry vision
- unclear speech
You may get some weight loss when you start treatment with ZAVESCA. If you do lose some weight when you start treatment with ZAVESCA, don't worry. People usually stop losing weight as treatment goes on.
These are the more common side effects of ZAVESCA. Mostly these are mild and short-lived. They usually happen at the start of treatment or at intervals during treatment.
Other side effects not listed above may also occur in some patients. Tell your doctor if you notice anything else that is making you feel unwell.
Do not be alarmed by this list of possible side effects. You may not experience any of them.
After using ZAVESCA
Storage
Keep your capsules in the blister pack until it is time to take them. If you take the capsules out of the box or the blister pack they may not keep well.
Keep it in a cool dry place where the temperature stays below 30°C.
Do not store it or any other medicine in the bathroom or near a sink.
Do not leave it in the car on hot days.
Heat and dampness can destroy some medicines.
Keep it where children cannot reach it. A locked cupboard at least one and a half metres above the ground is a good place to store medicines.
Disposal
If your doctor tells you to stop taking the capsules or the capsules have passed their use by date, ask your pharmacist what to do with any that are left over.
Product description
What it looks like
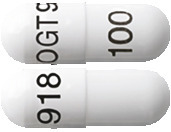
ZAVESCA are white, hard capsules with “OGT 918” printed in black on the cap and “100” printed in black on the body.
ZAVESCA is in blister packs of 90 capsules.
The Australian Registration Number is AUST R 122957
Ingredients
Each capsule contains 100 mg miglustat as the active ingredient.
ZAVESCA also contains the following inactive ingredients:
- sodium starch glycollate
- povidone
- magnesium stearate
- empty hard gelatin capsules size 4 white Op. 44.000/44.000 pure bovine (ARTG PI No 108031)
- OPACODE monogramming ink S-1-277002 black (ARTG PI No 107581), OPACODE monogramming ink S-1-27794 black (ARTG PI No 12104) or TekPrint SW-9008 Black Ink (ARTG PI No 2328)
Sponsor
JANSSEN-CILAG Pty Ltd
1-5 Khartoum Road
Macquarie Park NSW 2113 Australia
Telephone: 1800 226 334
NZ Office: Auckland New Zealand
Telephone: 0800 800 806
This leaflet was prepared in February 2022.
Published by MIMS April 2022

 Temporary dose reduction may be necessary in some patients because of diarrhoea.
Temporary dose reduction may be necessary in some patients because of diarrhoea.
 Bone manifestations of type 1 Gaucher disease were evaluated in 3 open label clinical studies (studies 1, 3 and 4) in patients treated with miglustat 100 mg t.i.d. for up to 2 years (n = 72). In a pooled analysis of uncontrolled data, bone mineral density Z-scores at the lumbar spine and femoral neck increased by more than 0.1 units from baseline in 27/47 (57%) and 28/43 (65%) of the patients with longitudinal bone density measurements. There were no events of bone crisis, avascular necrosis or fracture during the treatment period.
Bone manifestations of type 1 Gaucher disease were evaluated in 3 open label clinical studies (studies 1, 3 and 4) in patients treated with miglustat 100 mg t.i.d. for up to 2 years (n = 72). In a pooled analysis of uncontrolled data, bone mineral density Z-scores at the lumbar spine and femoral neck increased by more than 0.1 units from baseline in 27/47 (57%) and 28/43 (65%) of the patients with longitudinal bone density measurements. There were no events of bone crisis, avascular necrosis or fracture during the treatment period. A qualitative examination of the main sequences scatter plots and visual comparison of the regression slopes for the plots of saccades from 26 patients who provided useable data at both baseline and month 12 (or last visit) showed in the Zavesca group, 15/19 patients (79%) were stable or improved (7 improved, 8 no change), 2 deteriorated, and 2 had ambiguous results while in the no treatment group, 2/7 patients (29%) were stable or improved (1 improved, 1 with no change), 3 deteriorated, and 2 had ambiguous results.
A qualitative examination of the main sequences scatter plots and visual comparison of the regression slopes for the plots of saccades from 26 patients who provided useable data at both baseline and month 12 (or last visit) showed in the Zavesca group, 15/19 patients (79%) were stable or improved (7 improved, 8 no change), 2 deteriorated, and 2 had ambiguous results while in the no treatment group, 2/7 patients (29%) were stable or improved (1 improved, 1 with no change), 3 deteriorated, and 2 had ambiguous results. Secondary efficacy endpoints: swallowing function, motor disability, and cognitive ability were also assessed. Swallowing function was assessed on a rating scale, evaluating the patient's ability to swallow water and food substances of varying consistencies. The observed relative risk for any deterioration of swallowing function up to month 12 with Zavesca vs. no treatment was 0.4 (95% CI 0.13, 1.22, p = 0.17).
Secondary efficacy endpoints: swallowing function, motor disability, and cognitive ability were also assessed. Swallowing function was assessed on a rating scale, evaluating the patient's ability to swallow water and food substances of varying consistencies. The observed relative risk for any deterioration of swallowing function up to month 12 with Zavesca vs. no treatment was 0.4 (95% CI 0.13, 1.22, p = 0.17).
 Molecular formula: C10H21NO4.
Molecular formula: C10H21NO4.