What is in this leaflet
Read this leaflet carefully before taking your medicine.
This leaflet answers some common questions about adefovir. It does not contain all the available information. It does not take the place of talking to your doctor or pharmacist.
The information in this leaflet was last updated on the date listed on the last page. More recent information on this medicine may be available.
Ask your doctor or pharmacist:
- if there is anything you do not understand in this leaflet,
- if you are worried about taking your medicine, or
- to obtain the most up-to-date information.
You can also download the most up to date leaflet from www.apotex.com.au.
All medicines have risks and benefits. Your doctor has weighed the risks of you using this medicine against the benefits they expect it will have for you.
Pharmaceutical companies cannot give you medical advice or an individual diagnosis.
Keep this leaflet with your medicine. You may want to read it again.
What this medicine is used for
The name of your medicine is APO-Adefovir tablets. It contains the active ingredient adefovir dipivoxil.
It is used to treat chronic hepatitis B in patients 12 years of age or older.
Ask your doctor if you have any questions about why this medicine has been prescribed for you. Your doctor may have prescribed this medicine for another reason.
This medicine is available only with a doctor's prescription.
How it works
Adefovir belongs to a group of medicines called antiviral medicines.
Hepatitis B is caused by infection with the hepatitis B virus (HBV) which can damage the liver. Adefovir reduces the amount of the virus in your body, by lowering the ability of the virus to multiply and infect new liver cells and can improve the inflammation and scar tissue caused by the hepatitis B virus in your liver. Lowering the amount of virus in your body may reduce the chance of developing cirrhosis, liver failure and liver cancer.
We do not know how long adefovir may help treat your hepatitis. Sometimes viruses change in your body and medicines no longer work. This is called drug resistance.
There is no evidence that this medicine is addictive.
Use in children
This medicine should not be used in children under 12 years of age.
Before you take this medicine
When you must not take it
Do not take this medicine if:
- You are hypersensitive to, or have had an allergic reaction to, adefovir, adefovir dipivoxil or any of the ingredients listed at the end of this leaflet.
Symptoms of an allergic reaction may include: cough, shortness of breath, wheezing or difficulty breathing; swelling of the face, lips, tongue, throat or other parts of the body; rash, itching or hives on the skin; fainting; or hay fever-like symptoms.
If you think you are having an allergic reaction, do not take any more of the medicine and contact your doctor immediately or go to the Accident and Emergency department at the nearest hospital. - The expiry date (EXP) printed on the pack has passed.
- The packaging is torn, shows signs of tampering or it does not look quite right.
Before you start to take it
Before you start taking this medicine, tell your doctor if:
- You have allergies to:
- any other medicines
- any other substances, such as foods, preservatives or dyes.
- You have or have had any medical conditions, especially the following:
- kidney problems
If you have reduced function of your kidneys or are at risk of having reduced function then adefovir may damage your kidneys. While taking this medicine you will require regular tests of your kidney function and may require a smaller dose of this medicine than patients with normal kidney function. - unrecognised or untreated HIV infection.
Adefovir may reduce the effectiveness of some drugs used to treat HIV. There is limited experience in treating individuals with both chronic hepatitis B infection and HIV. Your doctor should offer to test your blood to see if you have HIV infection before you start treatment with this medicine.
- You are over the age of 65.
- You are currently pregnant or you plan to become pregnant.
The safe use of adefovir in human pregnancy has not been demonstrated. For this reason, it is important that women of childbearing age receiving treatment with adefovir use an effective method of contraception to avoid becoming pregnant. Do not take this medicine whilst pregnant until you and your doctor have discussed the risks and benefits involved.
- You are currently breastfeeding or you plan to breast-feed.
It is not known whether adefovir is excreted in human breast milk. Consequently, nursing mothers should stop breastfeeding during treatment with this medicine.
- You are planning to have surgery or an anaesthetic.
- You are currently receiving or are planning to receive dental treatment.
- You are taking or are planning to take any other medicines. This includes vitamins and supplements that are available from your pharmacy, supermarket or health food shop.
Some medicines may interact with adefovir.
These medicines should not be administered with adefovir:
- VIREAD (tenofovir disoproxil fumarate)
- TRUVADA (tenofovir disoproxil fumarate/emtricitabine combination tablet),
- ATRIPLA (tenofovir disoproxil fumarate/ emtricitabine/efavirenz combination tablet)
- STRIBILD (tenofovir disoproxil fumarate/emtricitabine/elvitegravir/cobicistat)
- EVIPLERA (tenofovir disoproxil fumarate/emtricitabine/ rilpivirine combination tablet).
- tenofovir alafenamide tablet
If you are taking this, you may need a different dose or you may need to take different medicines.
Other medicines not listed above may also interact with adefovir.
How to take this medicine
Follow carefully all directions given to you by your doctor. Their instructions may be different to the information in this leaflet.
How much to take
Your doctor will tell you how much of this medicine you should take. This will depend on your condition and whether you are taking any other medicines.
Do not stop taking your medicine or change your dosage without first checking with your doctor.
Adults, adolescents and children:
The recommended dose is one 10mg tablet taken once daily.
Doses greater than 10mg daily should not be taken.
If you have reduced function of your kidneys, you may require a lower dose. You may be prescribed another HBV medicine to take with this medicine. Check with your doctor if you have any questions.
This medicine is absorbed rapidly. Do not take another dose of this medicine if vomiting has occurred unless advised to do so by your doctor.
How to take it
Swallow tablet with water.
When to take it
Take this medicine at the same time each day. Taking it at the same time each day will have the best effect and will also help you remember when to take it.
It does not matter if you take it with or without food. Food does not affect how this medicine works.
How long to take it for
This medicine helps to control your condition, but does not cure it, you will need to take this medicine every day.
Continue taking your medicine for as long as your doctor tells you.
It is very important to continue taking this medicine because the amount of virus in your blood may increase if the medicine is stopped for even a short period of time. The virus may develop resistance to adefovir, become harder to treat and may result in very severe hepatitis and serious liver problems.
Make sure you have enough to last over weekends and holidays.
If you forget to take it
If it is almost time to take your next dose, skip the missed dose and take your next dose at the usual time. Otherwise, take it as soon as you remember and then go back to taking your medicine as you would normally.
Do not take a double dose to make up for missed doses. This may increase the chance of you experiencing side effects.
If you have trouble remembering to take your medicine, ask your pharmacist for some hints to help you remember.
If you take too much (overdose)
If you think that you or anyone else may have taken too much of this medicine, immediately telephone your doctor or the Poisons Information Centre (Tel: 13 11 26 in Australia) for advice. Alternatively, go to the Accident and Emergency department at your nearest hospital.
Do this even if there are no signs of discomfort or poisoning. You may need urgent medical attention.
While you are taking this medicine
Things you must do
Tell your doctor that you are taking this medicine if:
- you are about to be started on any new medicine
- you are pregnant or are planning to become pregnant
- you are breastfeeding or are planning to breast-feed
- you are about to have any blood tests
- you are going to have surgery or an anaesthetic or are going into hospital
- for any reason you have not taken your medicine exactly as prescribed.
Tell any other doctors, dentists and pharmacists who are treating you that you take this medicine.
Things you must not do
Do not:
- Stop taking this medicine or change the dose without first checking with your doctor.
- Give this medicine to anyone else, even if their symptoms seem similar to yours.
- Take your medicine to treat any other condition unless your doctor tells you to.
Things to be careful of
Be careful when driving or operating machinery until you know how this medicine affects you.
This medicine does not reduce the risk of passing HBV to others through sexual contact or blood contamination. Therefore, it is important to continue to take appropriate precautions to prevent passing HBV to others.
Hepatic flares
It is extremely important that you do not stop taking this medicine without your doctor's advice. Some patients with hepatitis B infection may have a "flare-up" of Hepatitis B if they stop taking this medicine, where the disease suddenly returns in a worse way than before. This flare-up may lead to liver failure and possibly liver transplantation or death.
Renal impairment
Long-term treatment with adefovir dipivoxil may increase the risk of renal impairment. While the overall risk of renal impairment in patients with adequate renal function is low, this is of special importance in patients both at risk of or having underlying renal dysfunction, and also in patients receiving medicinal products that may affect renal function.
After stopping this medicine, tell your doctor immediately about any new, unusual, or worsening symptoms that you notice after stopping treatment.
After you stop taking this medicine, you doctor will still need to check your health and take blood tests to check your liver for several months.
Possible side effects
Tell your doctor as soon as possible if you do not feel well while you are taking adefovir or if you have any questions or concerns.
Do not be alarmed by the following lists of side effects. You may not experience any of them. All medicines can have side effects. Sometimes they are serious but most of the time they are not.
Tell your doctor if you notice any of the following:
- Weakness
- Headache
- Nausea
- Flatulence
- Diarrhoea
- Problems with digestion
- Stomach pain
If you experience any of the following, stop taking your medicine and contact your doctor immediately or go to the Accident and Emergency department at your nearest hospital.
These are very serious side effects and you may need urgent medical attention or hospitalisation:
- Serious Liver Problems (hepatotoxicity)
- Your skin or the white part of your eyes turns yellow (jaundice)
- Your urine turns dark
- Your bowel movements (stools) turn light in colour
- Nausea
- Stomach pains
These side effects may be due to a condition called hepatotoxicity with liver enlargement and fat deposits in the liver (steatosis) which sometimes occurs in patients taking antiviral medicines. - Lactic Acidosis
- You feel very weak or tired.
- You have unusual (not normal) muscle pain.
- You have trouble breathing.
- You have stomach pain with nausea and vomiting.
- You feel cold, especially in your arm and legs.
- You feel dizzy or lightheaded.
- You have a fast or irregular heartbeat.
These side effects may be due to a condition called lactic acidosis (build-up of an acid in the blood). Lactic acidosis can be a medical emergency and may need to be treated in the hospital.
Other side effects not listed above may occur in some patients.
Allergic reactions
If you think you are having an allergic reaction to adefovir, do not take any more of this medicine and tell your doctor immediately or go to the Accident and Emergency department at your nearest hospital.
Symptoms of an allergic reaction may include some or all of the following:
- cough, shortness of breath, wheezing or difficulty breathing
- swelling of the face, lips, tongue, throat or other parts of the body
- rash, itching or hives on the skin
- fainting
- hay fever-like symptoms.
Storage and disposal
Storage
Keep your medicine in its original packaging until it is time to take it. If you take your medicine out of its original packaging it may not keep well.
Keep your medicine in a cool dry place where the temperature will stay below 25°C.
Do not store your medicine, or any other medicine, in the bathroom or near a sink. Do not leave it on a window sill or in the car. Heat and dampness can destroy some medicines.
Keep this medicine where children cannot reach it. A locked cupboard at least one-and-a-half metres above the ground is a good place to store medicines.
Disposal
If your doctor tells you to stop taking this medicine or it has passed its expiry date, your pharmacist can dispose of the remaining medicine safely.
Product description
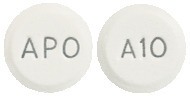
What APO-Adefovir tablets looks like
10mg Tablets:
White to off-white, round, flat-faced bevelled edge tablet. Engraved "APO" on one side, "A10" on the other side.
Available in bottles (white, round HDPE bottle with white PP 'Lift N Peel' child-resistant cap and desiccant) of 30 tablets.
Ingredients
Each tablet contains 10 mg of adefovir as the active ingredient.
It also contains the following inactive ingredients:
- Lactose monohydrate
- pregelatinized maize starch
- Croscarmellose sodium
- Magnesium stearate
- Purified talc
This medicine is gluten-free, sucrose-free, tartrazine-free and free of other azo dyes.
Australian Registration Numbers
APO-Adefovir 10mg Tablet:
AUST R 212048.
Sponsor
Arrotex Pharmaceuticals Pty Ltd
15-17 Chapel St,
Cremorne VIC 3121
http://arrotex.com.au/.
This leaflet was last updated in February 2023.
Published by MIMS April 2023

 The pharmacokinetics of adefovir has not been evaluated in non-haemodialysis patients with creatinine clearance < 10 mL/min, therefore, no dosing recommendation is available for these patients.
The pharmacokinetics of adefovir has not been evaluated in non-haemodialysis patients with creatinine clearance < 10 mL/min, therefore, no dosing recommendation is available for these patients. Patients who received adefovir dipivoxil beyond week 48 in study 438 reported adverse reactions similar in nature and severity to those reported in the first 48 weeks of treatment. With increased adefovir exposure, the incidence of adverse events related to treatment increased only slightly.
Patients who received adefovir dipivoxil beyond week 48 in study 438 reported adverse reactions similar in nature and severity to those reported in the first 48 weeks of treatment. With increased adefovir exposure, the incidence of adverse events related to treatment increased only slightly. With extended treatment in 125 HBeAg negative patients (up to 240 weeks duration), 4 patients had confirmed increases in serum creatinine of at least 0.5 mg/dL from baseline with 1 patient discontinuing from the study due to the elevated serum creatinine concentration. No patients had confirmed serum phosphorus levels of ≤ 2.0 mg/dL.
With extended treatment in 125 HBeAg negative patients (up to 240 weeks duration), 4 patients had confirmed increases in serum creatinine of at least 0.5 mg/dL from baseline with 1 patient discontinuing from the study due to the elevated serum creatinine concentration. No patients had confirmed serum phosphorus levels of ≤ 2.0 mg/dL. Histological improvement was observed more frequently in patients treated with adefovir dipivoxil than in those treated with placebo after 48 weeks of treatment.
Histological improvement was observed more frequently in patients treated with adefovir dipivoxil than in those treated with placebo after 48 weeks of treatment. Blinded, ranked assessments of both necroinflammatory activity and fibrosis at baseline and at week 48 demonstrated that patients treated with adefovir dipivoxil had improved necroinflammation and fibrosis compared to patients treated with placebo.
Blinded, ranked assessments of both necroinflammatory activity and fibrosis at baseline and at week 48 demonstrated that patients treated with adefovir dipivoxil had improved necroinflammation and fibrosis compared to patients treated with placebo.
 At week 96, 50/70 (71%) of patients receiving continued treatment with adefovir dipivoxil achieved a reduction in viral load to nondetectable levels (< 1000 copies/mL), and 47/64 (73%) of patients had normalisation of ALT levels. In most patients who stopped treatment with adefovir dipivoxil, HBV DNA and ALT levels returned towards baseline and there was a reversion of histological improvement.
At week 96, 50/70 (71%) of patients receiving continued treatment with adefovir dipivoxil achieved a reduction in viral load to nondetectable levels (< 1000 copies/mL), and 47/64 (73%) of patients had normalisation of ALT levels. In most patients who stopped treatment with adefovir dipivoxil, HBV DNA and ALT levels returned towards baseline and there was a reversion of histological improvement.

 Monotherapy with adefovir resulted in a progressive loss of YMDD mutations through 48 weeks; 7 patients (37%) in this treatment group had reverted to wild type HBV at week 48. Continuation of lamivudine therapy, either as monotherapy or in combination with adefovir resulted in the maintenance of YMDD mutations with only one patient in the combination treatment arm reverting to HBV without YMDD mutations through 48 weeks of treatment. Loss of YMDD mutations in the adefovir-treated patients was not associated with serum HBV DNA increases or ALT flares. There was no evidence of the development of adefovir-associated resistance mutations in the HBV polymerase during 48 weeks of treatment with adefovir either alone or in combination with lamivudine.
Monotherapy with adefovir resulted in a progressive loss of YMDD mutations through 48 weeks; 7 patients (37%) in this treatment group had reverted to wild type HBV at week 48. Continuation of lamivudine therapy, either as monotherapy or in combination with adefovir resulted in the maintenance of YMDD mutations with only one patient in the combination treatment arm reverting to HBV without YMDD mutations through 48 weeks of treatment. Loss of YMDD mutations in the adefovir-treated patients was not associated with serum HBV DNA increases or ALT flares. There was no evidence of the development of adefovir-associated resistance mutations in the HBV polymerase during 48 weeks of treatment with adefovir either alone or in combination with lamivudine.
 A four hour period of haemodialysis removed approximately 35% of the adefovir dose. The effect of peritoneal dialysis on adefovir removal has not been evaluated.
A four hour period of haemodialysis removed approximately 35% of the adefovir dose. The effect of peritoneal dialysis on adefovir removal has not been evaluated. In several clinical studies (HBeAg positive, HBeAg negative, pre- and post-liver transplantation with lamivudine resistant HBV and lamivudine resistant HBV/HIV coinfected patients), genotypic analyses were conducted on HBV isolates from 379 of a total of 629 adefovir dipivoxil patients with detectable levels of HBV DNA at week 48. No HBV DNA polymerase mutations associated with resistance to adefovir were identified when patients were genotyped at baseline and at week 48. After 96, 144, 192 and 240 weeks of treatment with adefovir dipivoxil, resistance surveillance was performed for 293, 221, 116 and 64 patients, respectively. Two novel conserved site mutations were identified in the HBV polymerase gene (rtN236T and rtA181V), which conferred clinical resistance to adefovir dipivoxil. Resistance to adefovir dipivoxil is delayed and infrequent. The cumulative probabilities of developing these adefovir-associated resistance mutations in all patients treated with adefovir dipivoxil were 0% at 48 weeks and approximately 2%, 7%, 14% and 25% after 96, 144, 192 and 240 weeks, respectively. These cumulative probabilities combine results in patients receiving adefovir dipivoxil as monotherapy and in combination with lamivudine.
In several clinical studies (HBeAg positive, HBeAg negative, pre- and post-liver transplantation with lamivudine resistant HBV and lamivudine resistant HBV/HIV coinfected patients), genotypic analyses were conducted on HBV isolates from 379 of a total of 629 adefovir dipivoxil patients with detectable levels of HBV DNA at week 48. No HBV DNA polymerase mutations associated with resistance to adefovir were identified when patients were genotyped at baseline and at week 48. After 96, 144, 192 and 240 weeks of treatment with adefovir dipivoxil, resistance surveillance was performed for 293, 221, 116 and 64 patients, respectively. Two novel conserved site mutations were identified in the HBV polymerase gene (rtN236T and rtA181V), which conferred clinical resistance to adefovir dipivoxil. Resistance to adefovir dipivoxil is delayed and infrequent. The cumulative probabilities of developing these adefovir-associated resistance mutations in all patients treated with adefovir dipivoxil were 0% at 48 weeks and approximately 2%, 7%, 14% and 25% after 96, 144, 192 and 240 weeks, respectively. These cumulative probabilities combine results in patients receiving adefovir dipivoxil as monotherapy and in combination with lamivudine. Chemical Name: 9-[2[[bis[(pivaloyloxy)-methoxy]phosphinyl]methoxy]ethyl]adenine.
Chemical Name: 9-[2[[bis[(pivaloyloxy)-methoxy]phosphinyl]methoxy]ethyl]adenine.