SUMMARY CMI
PULMICORT®
Consumer Medicine Information (CMI) summary
The full CMI on the next page has more details. If you are worried about using this medicine, speak to your doctor or pharmacist.
1. Why am I using Pulmicort?
Pulmicort contains the active ingredient budesonide. Pulmicort is inhaled into the lungs for the treatment of asthma. Pulmicort may also be used to treat croup in infants and children.
For more information, see Section 1. Why am I using Pulmicort? in the full CMI.
2. What should I know before I use Pulmicort?
Do not use if you have ever had an allergic reaction to any medicine containing budesonide or any of the ingredients listed at the end of the CMI.
Talk to your doctor if you have any other medical conditions, take any other medicines, or are pregnant or plan to become pregnant or are breastfeeding.
For more information, see Section 2. What should I know before I use Pulmicort? in the full CMI.
3. What if I am taking other medicines?
Some medicines may interfere with Pulmicort and affect how it works.
A list of these medicines is in Section 3. What if I am taking other medicines? in the full CMI.
4. How do I use Pulmicort?
- Pulmicort comes in two different forms: the Turbuhaler or Respules (containing nebulising suspension) for use in a nebuliser.
- Follow all directions given to you by your doctor or pharmacist.
More instructions can be found in Section 4. How do I use Pulmicort? in the full CMI.
5. What should I know while using Pulmicort?
| Things you should do |
|
| Things you should not do |
|
| Looking after your medicine |
|
For more information, see Section 5. What should I know while using Pulmicort? in the full CMI.
6. Are there any side effects?
All medicines can have side effects. If you do experience any side effects, most of them are minor and temporary. These include sore, yellowish, raised patches in the mouth (thrush), hoarse voice, dry mouth, unpleasant taste in your mouth, cough, thirsty, headache, light-headedness, tiredness, nausea, diarrhoea, weight gain, or skin rash. However, some side effects may need medical attention. These include severe allergic reactions such as difficulty breathing, swelling of the face, lips or tongue, severe rash or mood changes such as depression). Serious side effects are rare.
For more information, including what to do if you have any side effects, see Section 6. Are there any side effects? in the full CMI.
FULL CMI
PULMICORT®
Active ingredient(s): budesonide
Consumer Medicine Information (CMI)
This leaflet provides important information about using Pulmicort. You should also speak to your doctor or pharmacist if you would like further information or if you have any concerns or questions about using Pulmicort.
Where to find information in this leaflet:
1. Why am I using Pulmicort?
2. What should I know before I use Pulmicort?
3. What if I am taking other medicines?
4. How do I use Pulmicort?
5. What should I know while using Pulmicort?
6. Are there any side effects?
7. Product details
1. Why am I using Pulmicort?
Pulmicort contains the active ingredient budesonide. This belongs to a family of medicines called corticosteroids, which are used to reduce inflammation in many parts of the body.
Pulmicort is inhaled into the lungs for the treatment of asthma. Asthma is a disease where the airways of your lungs become narrow and inflamed (red and swollen), making it difficult to breathe. This may be due to an allergy to house dust mites, smoke, air pollution or other things that irritate your lungs.
Pulmicort acts directly on your airways to reduce inflammation. This helps to improve your condition and to prevent asthma attacks from occurring. It is a preventer and needs to be taken regularly.
Pulmicort Respules may also be used to treat croup in infants and children.
2. What should I know before I use Pulmicort?
Warnings
Do not use Pulmicort if:
- you are allergic to budesonide, or any of the ingredients listed at the end of this leaflet. Always check the ingredients to make sure you can use this medicine.
Check with your doctor if you:
- have any allergies to any other medicines or foods.
- have, or have had, any of the following medical conditions, as it may not be safe for you to take Pulmicort:
- liver problems
- tuberculosis (TB) - currently have an infection. If you take Pulmicort while you have an infection, the medicine may hide some of the signs of an infection. This may make you think, mistakenly, that you are better or that it is not serious.
- have any other medical conditions.
During treatment, you may be at risk of developing certain side effects. It is important you understand these risks and how to monitor for them. See additional information under Section 6. Are there any side effects?
Pregnancy and breastfeeding
Check with your doctor if you are pregnant or intend to become pregnant.
Talk to your doctor if you are breastfeeding or intend to breastfeed.
Your doctor will advise you of the risks and benefits of using Pulmicort during pregnancy and while breastfeeding.
3. What if I am taking other medicines?
Some medicines may interfere with Pulmicort and affect how it works. These include:
- other corticosteroid medicines, such as tablets, asthma inhalers, nasal sprays, or eye/nose drops.
- medicines used to treat fungal infections (such as ketoconazole, itraconazole).
These medicines may be affected by Pulmicort, or may affect how well it works. You may need different amounts of your medicine, or you may need to use a different medicine. Your doctor or pharmacist will advise you.
Check with your doctor or pharmacist if you are not sure about what medicines, vitamins or supplements you are taking and if these affect Pulmicort.
Your doctor and pharmacist may have more information on medicines to be careful with or avoid while using Pulmicort.
4. How do I use Pulmicort?
How to use Pulmicort
Pulmicort comes in two different forms:
- The Turbuhaler; or
- Respules (containing nebulising suspension) for use in a nebuliser.
Each package of Pulmicort contains an instruction for use leaflet that tells you the correct way to use it. Please read it carefully.
If you are not sure how to use the Turbuhaler or Respules, ask your doctor or pharmacist.
How much to take
Pulmicort Turbuhaler
ASTHMA - Adult dose
The dose can range from 400 to 2400 micrograms per day, in divided doses (either 2, 3 or 4 times a day).
If you take 400 micrograms or less a day, you may take this as a single daily dose in the morning or evening.
When your asthma is under control, your doctor may tell you to use a lower dose. The usual maintenance dose is 100 to 400 micrograms per day. This may be given as a once or twice daily dose.
ASTHMA - Children's dose
Children are usually considered to be aged 12 years or less, but check with your doctor if you are at all worried about the dose that has been prescribed for your child.
Children should be 5 years or older before they use the Turbuhaler.
The dose can range from 200 to 800 micrograms per day, in divided doses (either 2, 3 or 4 times a day).
When your child's asthma is under control, the doctor may prescribe a lower dose for your child. The usual maintenance dose is 100 to 400 micrograms per day. This may be given as a once or twice daily dose.
Pulmicort Respules
ASTHMA - Adult dose
The dose can range from 1 to 2 mg twice a day.
When your asthma is under control, your doctor may tell you to use a lower dose. The usual maintenance dose is 0.5 to 1 mg twice a day.
ASTHMA - Children's dose
Children are usually considered to be aged 12 years or less, but check with your doctor if you are at all worried about the dose that has been prescribed for your child.
The dose can range from 0.5 to 1 mg twice a day.
When your child's asthma is under control, the doctor may prescribe a lower dose for your child. The usual maintenance dose is 0.25 to 0.5 mg twice a day.
CROUP
Pulmicort Respules can also be used to treat croup in infants and children. It will be given as one 2 mg dose of budesonide.
If you forget to use Pulmicort
Pulmicort should be used regularly at the same time each day. If you miss your dose at the usual time, use it as soon as you remember, and then go back to using your medicine as you would normally.
Do not take a double dose to make up for the dose you missed. This may increase the chance of you getting an unwanted side effect.
If you are not sure what to do, ask your doctor or pharmacist. If you have trouble remembering to use your medicine, ask your pharmacist for some hints.
If you use too much Pulmicort
If you think that you/your child have used too much Pulmicort, you/your child may need urgent medical attention.
You should immediately:
- phone the Poisons Information Centre
(by calling 13 11 26), or - contact your doctor, or
- go to the Emergency Department at your nearest hospital.
You should do this even if there are no signs of discomfort or poisoning.
5. What should I know while using Pulmicort?
Things you should do
Follow all directions given to you by your doctor or pharmacist carefully. They may differ from the information contained in this leaflet.
Your doctor should give you a personal Asthma Action Plan to help manage your asthma. This plan will include medicines to take regularly to control your asthma, eg Pulmicort Turbuhaler, as well as reliever medicines to use when you have sudden attacks of breathlessness eg Bricanyl® (terbutaline) Turbuhaler.
If you are using more inhalations of your reliever medicine or you are wheezing or breathless more than usual, please contact your doctor so that your condition can be checked. This is important to ensure your breathing problem is controlled properly.
Continue using Pulmicort for as long as your doctor tells you to, even if you feel better. Pulmicort helps control your condition. Therefore you must use it every day.
See your doctor regularly to make sure that your asthma is not getting worse. Your doctor may change your dose of Pulmicort (up or down) depending on your condition.
If you become pregnant while using Pulmicort, tell your doctor or pharmacist.
Be sure to rinse your mouth out with water after every time you use Pulmicort. If you do not rinse your mouth, you are more likely to develop thrush in the mouth.
Be sure to wash your face after each use of Pulmicort Respules. If you do not wash your face you might get irritation of the skin.
Remind any doctor, dentist or pharmacist you visit that you are using Pulmicort.
Things you should not do
- Do not stop using Pulmicort for your asthma without checking with your doctor.
- Do not use Pulmicort to treat any other complaints unless your doctor tells you to.
- Do not give Pulmicort to anyone else, even if they have the same condition as you.
Looking after your medicine
Follow the instructions for use leaflet in the carton on how to take care of your medicine properly.
Storage
Keep your Pulmicort Turbuhaler in a cool dry place where the temperature stays below 30 degrees C, with the cover firmly in place.
Keep your Pulmicort Respules protected from light by keeping them in the foil envelopes and in a cool dry place where the temperature stays below 30 degrees C. Do not refrigerate or freeze.
Do not store Pulmicort:
- in the bathroom or near a sink, or
- in the car or on window sills.
Keep it where young children cannot reach it.
Cleaning
The Turbuhaler must be wiped with a clean dry tissue and must never get wet.
Full instructions on the right way to use and clean the Turbuhaler are inside the pack.
When to discard your medicine
Unused, unopened Respules should be discarded 3 months after opening the foil pack.
Getting rid of any unwanted medicine
If you no longer need to use this medicine or it is out of date, take it to any pharmacy for safe disposal.
Do not use this medicine after the expiry date.
6. Are there any side effects?
All medicines can have side effects. If you do experience any side effects, most of them are minor and temporary. However, some side effects may need medical attention.
See the information below and, if you need to, ask your doctor or pharmacist if you have any further questions about side effects.
Less serious side effects
| Less serious side effects | What to do |
Mouth and throat-related:
| These are less likely to happen if you rinse your mouth out after every time you use Pulmicort. Speak to your doctor if you have any of these less serious side effects and they worry you. |
Nose and throat-related:
| Speak to your doctor if you have any of these less serious side effects and they worry you. |
| Speak to your doctor if you notice any of these. You may need urgent medical attention. |
Serious side effects
| Serious side effects | What to do |
Allergic Reaction:
| Call your doctor straight away, or go straight to the Emergency Department at your nearest hospital if you notice any of these serious side effects. You may need urgent medical attention. Serious side effects are rare. |
| Potential eye problem: Any issues with your eyes such as blurred vision or other problems with your eyesight. | Speak to your doctor if you notice any of these. Your doctor may need to send you to an ophthalmologist (eye doctor) to check that you don't have eye problems such as cataracts (clouding of the eye lens), glaucoma (increased pressure in your eyeballs) or other rare eye conditions reported with corticosteroids use. |
Other side effects
Adrenal glands
Your adrenal glands may be affected by taking high doses of corticosteroids over a long period of time or if you change from or use high doses of oral corticosteroids. Your doctor may do tests to check how the adrenal glands are working.
Your doctor may also tell you to take additional oral corticosteroids during period of stress such as trauma, surgery and infection.
Growth
Corticosteroids taken into the lungs for long periods (eg 12 months) may affect how children grow. In rare cases, some children may be sensitive to the growth effects of corticosteroids, so the doctor may monitor a child's height.
Tell your doctor or pharmacist if you notice anything else that may be making you feel unwell.
Other side effects not listed here may occur in some people.
Reporting side effects
After you have received medical advice for any side effects you experience, you can report side effects to the Therapeutic Goods Administration online at www.tga.gov.au/reporting-problems. By reporting side effects, you can help provide more information on the safety of this medicine.
Always make sure you speak to your doctor or pharmacist before you decide to stop taking any of your medicines.
7. Product details
This medicine is only available with a doctor's prescription.
What Pulmicort contains
| Active ingredient (main ingredient) | budesonide |
| Other ingredients (inactive ingredients) | Pulmicort Respules:
|
Do not take this medicine if you are allergic to any of these ingredients.
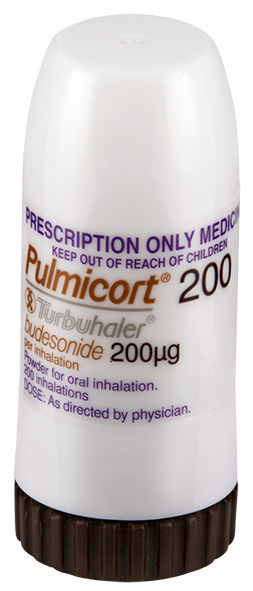
What Pulmicort looks like
Pulmicort Turbuhaler
Pulmicort Turbuhaler is a plastic inhaler containing the medicine as a dry powder. The inhaler has a light-brown turning grip. The colour of the cover is white.
Pulmicort Turbuhaler is registered in the following presentations*:
- 100 micrograms per inhalation: Each Turbuhaler contains 200 inhalations of the medicine. [AUST R 10063]
- 200 micrograms per inhalation: Each Turbuhaler contains 200 inhalations of the medicine. [AUST R 10065]
- 400 micrograms per inhalation: Each Turbuhaler contains 50 (sample) or 200 inhalations of the medicine. [AUST R 10064]
*not all registered presentations might be available in Australia
Pulmicort Respules
Pulmicort Respules nebulising suspension for inhalation is a white to off-white suspension in single dose plastic units.
Pulmicort Respules is registered in the following presentations*:
- 0.5 mg per 2 mL [AUST R 10072]
- 1 mg per 2 mL [AUST R 10071]
Each box contains 30 Respules with 5 or 10 Respules in each silver foil pack.
*not all registered presentations might be available in Australia
Who distributes Pulmicort
AstraZeneca Pty Ltd
ABN 54 009 682 311
66 Talavera Road
MACQUARIE PARK NSW 2113
Telephone: 1800 805 342
This leaflet was prepared on 23 February 2022.
®Pulmicort, Respules and Turbuhaler are registered trade marks of the AstraZeneca group of companies.
© AstraZeneca, 2022
Doc ID-000221037 v5.0
Published by MIMS April 2022



 If oropharyngeal candidiasis develops, it may be treated with appropriate anti-fungal therapy whilst still continuing with Pulmicort therapy. The incidence of candidiasis can generally be held to a minimum by having patients rinse their mouth with water after each inhalation.
If oropharyngeal candidiasis develops, it may be treated with appropriate anti-fungal therapy whilst still continuing with Pulmicort therapy. The incidence of candidiasis can generally be held to a minimum by having patients rinse their mouth with water after each inhalation.
