What is in this leaflet
This leaflet answers some common questions about DILTIAZEM AN. It does not contain all the available information.
It does not take the place of talking to your doctor or pharmacist.
All medicines have risks and benefits. Your doctor has weighed the risks of you taking DILTIAZEM AN against the benefits they expect it will have for you.
If you have any concerns about taking this medicine, ask your doctor or pharmacist.
Keep this leaflet with the medicine.
You may need to read it again.
What DILTIAZEM AN is used for
The name of your medicine is DILTIAZEM AN. It contains the active ingredient called diltiazem hydrochloride.
DILTIAZEM AN belongs to a group of medicines called calcium channel blockers or calcium antagonists. They work by opening up blood vessels, which lowers blood pressure and lets more blood and oxygen reach the heart. They do not change the amount of calcium in your blood or bones.
DILTIAZEM AN is used to prevent angina.
Angina is a pain or uncomfortable sensation in the chest, often spreading to the arms or neck and sometimes to the shoulders and back. The pain of angina is due to a shortage of oxygen to the heart.
Your doctor may have prescribed DILTIAZEM AN for another reason. Ask your doctor if you have any questions about why DILTIAZEM AN has been prescribed for you.
There is no evidence that DILTIAZEM AN is addictive.
This medicine is available only with a doctor’s prescription.
Before You Take DILTIAZEM AN
When you must not take it
Do not use DILTIAZEM AN if:
- you have an allergy to diltiazem hydrochloride or any of the ingredients listed at the end of this leaflet
Symptoms of an allergic reaction to these medicines may include:
- asthma, wheezing or shortness of breath
- swelling of the face, lips or tongue which may cause difficulty in swallowing or breathing
- hives, itching or skin rash
- fainting - you are pregnant, or intend to become pregnant.
DILTIAZEM AN may affect your developing baby if you take it during pregnancy. - you are breast-feeding or intend to breast-feed.
DILTIAZEM AN passes into breast milk and may affect your baby.
Do not use DILTIAZEM AN if the packaging is torn or shows signs of tampering.
Do not use DILTIAZEM AN if the expiry date (EXP) printed on the pack has passed.
If you take this medicine after the expiry date has passed, it may not work (as well).
If you are not sure whether you should start using DILTIAZEM AN, contact your doctor.
Do not give these medicines to a child.
The safety and effectiveness of these medicines have not been established in children.
Before you start to use it
Tell your doctor if:
- you have allergies to
- any other medicines
- any other substances such as foods, preservatives or dyes.
- you are pregnant or intend to become pregnant.
DILTIAZEM AN should not be used during pregnancy. - you are breast-feeding or planning to breast-feed.
Your doctor will discuss the risks and benefits of using DILTIAZEM AN during breastfeeding. A decision will have to be made whether to discontinue breastfeeding or discontinue therapy taking into consideration the importance of the medicine. - you have, or have had, the following medical conditions:
- Abnormal heart beat rhythm
- hypotension (low blood pressure)
- Heart attack or other heart-related complications
- Impaired renal (kidney) or hepatic (liver) function
- Diabetes
Taking other medicines
Tell your doctor if you are taking any other medicines, including any that you buy without a prescription from your pharmacy, supermarket or health food shop.
Some medicines may interfere with DILTIAZEM AN. These include:
- Dantrolene (a muscle relaxant)
- Some other medicines for your heart or high blood pressure (eg. beta blockers, digoxin, amiodarone, nitrates)
- Cyclosporin, which you may have been given after an operation or because of rheumatoid arthritis
- Rifampicin (an antibiotic)
- Cimetidine or ranitidine (for ulcers or reflux)
- Diazepam (for depression, alcohol withdrawal or anxiety)
- Carbamazepine (for bipolar disorder or epilepsy)
- Lithium (for bipolar disorder)
- Theophylline (for asthma and other breathing problems)
- Certain drugs used to treat prostate problems
- Inhaled anaesthetic agents such as halothane, isoflurane, enflurane (for surgery)
- Drugs used to lower your blood cholesterol (including simvastatin, lovastatin)
- Benzodiazepines or medicines used as sedatives or to treat anxiety such as midazolam, triazolam
- Corticosteroids such as methylprednisolone, prednisone, cortisone
- Antiarrhythmics or medicines used to treat irregular heart beats
These medicines may be affected by DILTIAZEM AN, or may affect how well it works. You may need to take different amounts of your medicine, or you may need to take different medicines. Your doctor will advise you.
Your doctor and pharmacist may have more information on medicines to be careful with or avoid while taking DILTIAZEM AN.
How to take DILTIAZEM AN
How much to take
DILTIAZEM AN is usually taken 3 - 4 times a day. Take the prescribed dose as directed by your doctor.
A lower dosage may be required in elderly patients (over 65 years old).
Follow all directions given to you by your doctor and pharmacist carefully. They may differ from the information contained in this leaflet.
If you do not understand the instructions on the box, ask your doctor or pharmacist for help.
How to take it
Swallow the tablets whole with a glass of water.
When to take it
Take DILTIAZEM AN tablets at the same time each day as directed by your doctor.
How long to take it
Take DILTIAZEM AN for as long as your doctor tells you to.
Do not stop taking DILTIAZEM AN suddenly because this can bring on an attack of angina.
If you forget to take it
If it is almost time for your next dose, skip the dose you missed and take your next dose when you are meant to. Otherwise, take it as soon as you remember, and then go back to taking your tablets as you would normally.
Do not take a double dose to make up for the dose you have missed.
If you are not sure what to do, ask your doctor or pharmacist.
If you have trouble remembering when to take your medicine, ask your pharmacist for hints.
If you take too much (overdose)
Immediately telephone your doctor or Poisons Information Centre (telephone 13 11 26), or go to casualty at your nearest hospital, if you think that you or anyone else may have taken too much DILTIAZEM AN. Do this even if there are no signs of discomfort or poisoning. You may need urgent medical attention.
If you take too much DILTIAZEM AN, you may feel dizzy and light-headed, feel pain in your left arm or chest or notice your heart beating very slowly. If any of these occur you should get medical attention immediately.
While you are taking DILTIAZEM AN
Things you must do
Use DILTIAZEM AN exactly as your doctor has prescribed.
If you do not follow your doctor's instructions, you may not get relief from your attacks of angina.
Tell your doctor if you continue to have angina attacks or if they become more frequent while you are using DILTIAZEM AN.
Tell all doctors, dentists and pharmacists who are treating you that you are taking DILTIAZEM AN.
Tell your doctor or pharmacist that you are taking DILTIAZEM AN if you are about to be started on any new medicines.
Things you must not do
Do not use it to treat any other complaints unless your doctor says to.
Do not give this medicine to anyone else, even if their symptoms seem similar to yours.
As mentioned previously, do not suddenly stop taking your medicine since this can cause severe angina for a day or two.
Things to be careful of
Be careful driving or operating machinery until you know how DILTIAZEM AN affects you.
DILTIAZEM AN may cause dizziness and fainting in some patients, especially when you first start to use it. Make sure you know how you react to DILTIAZEM AN before you drive a car, operate machinery, or do anything else that could be dangerous if this happens to you.
Be careful not to overdo physical activities when you first start using DILTIAZEM AN.
You may feel better when you start taking it, but you will need time to improve your physical fitness.
Get up slowly when getting out of bed or standing up if you feel light-headed, dizzy or faint.
If this is a problem and it gets worse or continues, talk to your doctor.
Side Effects
Tell your doctor or pharmacist as soon as possible if you do not feel well while you are using DILTIAZEM AN.
DILTIAZEM AN helps most people with angina, but it may have unwanted effects in a few people.
All medicines can have side effects. Sometimes they are serious, most of the time they are not. You may need medical treatment if you get some of the side effects.
Ask your doctor or pharmacist any questions you may have.
Tell your doctor if you notice any of the following and they worry you:
- swelling or flushing (feeling hot suddenly)
- headache
- nausea, vomiting, constipation, diarrhoea, indigestion, gastric pain
- dizziness
- confusion, hallucinations, abnormal dreams, mental depression or mood changes
- trouble sleeping
- nervousness, tremor
- ringing or other persistent noise in the ears
- loss of memory
- dry mouth
- loss of appetite
- weight increase
- increased sensitivity to the sun
- unusual movements or uncontrollable movements
- rash or an itchy, burning or prickly sensation
- small round, raised itchy areas on the skin
- weakness or tiredness
These are the more common side effects of DILTIAZEM AN. These side effects are usually mild.
If any of the following happen, stop taking DILTIAZEM AN and tell your doctor immediately or go to casualty at your nearest hospital:
- you feel continuously light headed or dizzy
- you notice your heart beating irregularly, slowly or very quickly
- you feel pain, which may be severe, in your left arm and chest
- you have blisters and bleeding in the lips, eyes, mouth, nose or genitals
- you have skin reactions such as red, painful or itchy spots, blisters or peeling of the skin.
These are very serious side effects. You may need urgent medical attention or hospitalisation. These side effects are rare.
Other side effects not listed above may also occur in some patients. Tell your doctor if you notice anything else that is making you feel unwell.
Ask your doctor or pharmacist if you don’t understand anything in this list.
Do not be alarmed by this list of possible side effects. You may not experience any of them.
After taking DILTIAZEM AN
Storage
Keep your tablets in their blister pack until it is time to take them.
If you take the tablets out of their blister pack they may not keep well.
Keep DILTIAZEM AN in a cool, dry place where it stays below 25°C. Do not store it, or any other medicine, in a bathroom or near a sink. Do not leave it in the car or on window sills.
Heat and dampness can destroy some medicines.
Keep this medicine where young children cannot reach it.
A locked cupboard at least one-and-a half metres above the ground is a good place to store medicines.
Disposal
If your doctor tells you to stop taking DILTIAZEM AN, or the tablets have passed their expiry date, ask your pharmacist what to do with any tablets left over.
Product description
What it looks like
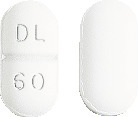
DILTIAZEM AN 60 mg tablets are white, film coated, capsule shaped and scored with one face embossed DL/60.
DILTIAZEM AN 60 mg tablets are available in blister packs (AUST R 184100) and bottle packs (AUST R 184098) of 90 tablets.
Ingredients
DILTIAZEM AN tablets contain 60 mg of the active ingredient diltiazem hydrochloride.
Other Ingredients:
- dried aluminium hydroxide
- hydrogenated castor oil
- lactose
- magnesium stearate
- methacrylic acid copolymer
- Opadry white Y-1-7000B (hypromellose, titanium dioxide, macrogol 400, indigo carmine CI73015)
- purified talc
DILTIAZEM AN does not contain sucrose, gluten, tartrazine or any other azo dyes.
Name and Address of the Sponsor
Amneal Pharma Australia Pty Ltd
12 River St
South Yarra, Vic, 3141
Australia
Date of Preparation
May 2015
Doc ID: 56.AN.M.2.0