SUMMARY CMI
PHYSIOTENS®
Consumer Medicine Information (CMI) summary
The full CMI on the next page has more details. If you are worried about taking this medicine, speak to your doctor or pharmacist.
1. Why am I taking PHYSIOTENS?
PHYSIOTENS contains the active ingredient moxonidine. PHYSIOTENS is used to lower high blood pressure. For more information, see Section 1. Why am I taking PHYSIOTENS? in the full CMI.
2. What should I know before I take PHYSIOTENS?
Do not use if you have ever had an allergic reaction to moxonidine or any of the ingredients listed at the end of the CMI.
Talk to your doctor if you have other medical conditions, take other medicines, or are pregnant or plan to become pregnant or are breastfeeding. For more information, see Section 2. What should I know before I take PHYSIOTENS? in the full CMI.
3. What if I am taking other medicines?
Some medicines may interfere with PHYSIOTENS and affect how it works or may be affected by PHYSIOTENS.
A list of these medicines is in Section 3. What if I am taking other medicines? in the full CMI.
4. How do I take PHYSIOTENS?
- The usual starting dose is one 200 micrograms tablet once per day. Depending on how your blood pressure responds, your dosage may be increased by your doctor.
- Swallow the tablets whole with a full glass of water or another liquid. Do not chew the tablets.
More instructions can be found in Section 4. How do I take PHYSIOTENS? in the full CMI.
5. What should I know while taking PHYSIOTENS?
| Things you should do |
|
| Things you should not do |
|
| Driving or using machines |
|
| Drinking alcohol |
|
| Looking after your medicine |
|
For more information, see Section 5. What should I know while taking PHYSIOTENS? in the full CMI.
6. Are there any side effects?
Speak to your doctor if you have any of these less serious side effects and they worry you: dry mouth, headache, lack of energy, dizziness, drowsiness, feeling sick, nausea, problems sleeping, skin flushing, anxiety. Tell your doctor as soon as possible if you notice any of these symptoms: severe allergic skin reactions (rash, itching, inflamed or reddened skin), swelling of the limbs. Call your doctor straight away, or go straight to the Emergency Department at your nearest hospital if you notice any of these serious side effects: angioedema (unusual swelling of the face, eyes, lips, inside the nose, mouth or throat), shortness of breath, breathing or swallowing difficulties.
For more information, including what to do if you have any side effects, see Section 6. Are there any side effects? in the full CMI.
FULL CMI
PHYSIOTENS®
Active ingredient: moxonidine
Consumer Medicine Information (CMI)
This leaflet provides important information about using PHYSIOTENS. You should also speak to your doctor or pharmacist if you would like further information or if you have any concerns or questions about taking PHYSIOTENS.
Where to find information in this leaflet:
1. Why am I taking PHYSIOTENS?
2. What should I know before I take PHYSIOTENS?
3. What if I am taking other medicines?
4. How do I take PHYSIOTENS?
5. What should I know while taking PHYSIOTENS?
6. Are there any side effects?
7. Product details
1. Why am I taking PHYSIOTENS?
PHYSIOTENS contains the active ingredient moxonidine.
PHYSIOTENS is used to lower high blood pressure, which is sometimes called hypertension.
Everyone has blood pressure. This pressure helps to move your blood around your body. Your blood pressure may change at different times of the day. You have hypertension when your blood pressure stays higher than normal, even when you are calm or relaxed.
There are usually no symptoms of hypertension. The only way of knowing if you have hypertension is to have your blood pressure checked regularly. If high blood pressure is not treated it can lead to serious health problems, including stroke, heart disease and kidney failure.
Ask your doctor if you have any questions about why it has been prescribed for you.
Your doctor may have prescribed PHYSIOTENS for another use.
2. What should I know before I take PHYSIOTENS?
Warnings
Do not take PHYSIOTENS if:
- you are allergic to moxonidine or any of the ingredients listed at the end of this leaflet.
Always check the ingredients to make sure you can take this medicine.
- you are pregnant or think you may be pregnant.
- you are breastfeeding. PHYSIOTENS passes into breast milk. Your doctor will discuss the possible risks and benefits of taking PHYSIOTENS when breastfeeding.
- you are aged 75 years or more
- have heart problems such as heart failure or abnormal rhythm
- have severe kidney disease
Do not give PHYSIOTENS to a child under the age of 16 years.
Safety and effectiveness in children younger than 16 years have not been established.
Do not take it after the expiry date (EXP) printed on the pack or if the packaging is torn or shows signs of tampering.
If it has expired or is damaged return it to your pharmacist for disposal.
If you are not sure whether you should start taking this medicine, talk to your doctor.
Check with your doctor if you have:
- any other medical conditions or take any medicines for any other condition
- any allergies to any other medicines, foods, dyes or preservatives
- angioedema, which is unusual swelling of the face, lips or tongue
- depression
- epilepsy
- glaucoma, a disease of increased pressure in the eye
- heart problems
- kidney problems
- leg pains or cramps caused by poor blood circulation
- Parkinson's disease, a disease of the nerves which causes uncontrolled shaking and stiffness
- Raynaud's disease, where your fingers go pale and blue and are painful in the cold
During treatment, you may be at risk of developing certain side effects. It is important you understand these risks and how to monitor for them. See additional information under Section 6. Are there any side effects?
Pregnancy and breastfeeding
Check with your doctor or pharmacist if you are pregnant, intend to become pregnant, are breastfeeding or intend to breastfeed.
Your doctor or pharmacist can discuss the risks and benefits involved.
3. What if I am taking other medicines?
Tell your doctor if you are already taking medicines to lower your blood pressure.
These medicines can have a combined effect when used with PHYSIOTENS to reduce blood pressure and your doctor may need to adjust the dose you have to take.
Tell your doctor or pharmacist if you are taking any other medicines, including any medicines, vitamins or supplements that you buy without a prescription from your pharmacy, supermarket or health food shop.
Some medicines may interfere with PHYSIOTENS and affect how it works or may be affected by PHYSIOTENS. These include:
- some medicines used to treat depression called "tricyclic" medicines (such as amitriptyline and imipramine)
- sleeping tablets or other medicines which make you feel drowsy
You may need to use different amounts of your medicine, or take different medicines.
Your doctor or pharmacist has more information on medicines to be careful with or to avoid while taking PHYSIOTENS.
Check with your doctor or pharmacist if you are not sure about what medicines, vitamins or supplements you are taking and if these affect PHYSIOTENS.
4. How do I take PHYSIOTENS?
How much to take
- Your doctor or pharmacist will tell you how many tablets to take each day.
- The usual starting dose of PHYSIOTENS is one 200 micrograms tablet once per day.
- Depending on how your blood pressure responds, your dosage may be increased by your doctor to 400 micrograms after 2 weeks. After a further 2 weeks, your doctor may increase your dosage to 600 micrograms per day. You should not take 600 micrograms as one dose, it should be taken as a divided dose.
- Ask your doctor how to divide your daily dose.
- Follow the instructions provided and use PHYSIOTENS until your doctor tells you to stop.
- The medicine helps control your condition, but it does not cure it. It is important to keep taking your medicine even if you feel well.
How to take PHYSIOTENS
- Swallow the tablets whole with a full glass of water or another liquid.
- Do not chew the tablets.
When to take PHYSIOTENS
- Take PHYSIOTENS at about the same time each day.
- Taking it at the same time each day will have the best effect. It will also help you remember when to take it.
- It does not matter if you take this medicine with or without food.
If you forget to take PHYSIOTENS
If it is almost time for your next dose, skip the dose you missed and take your next dose when you are meant to.
If there is still a long time to go before your next dose, take it as soon as you remember, and then go back to taking it as you would normally.
Do not take two doses within 6 hours of each other. Do not take a double dose to make up for the dose that you missed.
This may increase the chance of getting an unwanted side effect.
If you have trouble remembering when to take your medicine, ask your pharmacist for advice.
If you take too much PHYSIOTENS
If you think that you have taken too much PHYSIOTENS, you may need urgent medical attention.
You should immediately:
- phone the Poisons Information Centre
(Australia telephone 13 11 26) for advice, or - contact your doctor, or
- go to the Emergency Department at your nearest hospital.
You should do this even if there are no signs of discomfort or poisoning.
If possible, show the doctor the pack of tablets.
5. What should I know while taking PHYSIOTENS?
Things you should do
Keep all of your doctor's appointments so that your progress can be checked.
If you are going to have surgery, tell the surgeon that you are taking this medicine.
Make sure you drink enough water during exercise and hot weather when you are taking PHYSIOTENS, especially if you sweat a lot.
If you do not drink enough water while taking PHYSIOTENS, you may faint or feel light-headed or sick. This is because your body does not have enough fluid and your blood pressure is too low.
If you feel light-headed, dizzy or faint when getting out of bed or standing up, get up slowly.
Standing up slowly, especially when you get up from bed or chairs, will help your body get used to the change in position and blood pressure. If this problem continues or gets worse, talk to your doctor.
Tell your doctor:
- if you become pregnant while you are taking this medicine
- that you are taking this medicine if you are about to have any blood tests
- if you have excessive vomiting and/or diarrhoea while taking PHYSIOTENS. This can also mean that you are losing too much water and your blood pressure may become too low.
Remind any doctor, dentist or pharmacist you visit that you are taking PHYSIOTENS.
Things you should not do
- Do not use this medicine to treat any other complaints unless your doctor or pharmacist tells you to.
- Do not give this medicine to anyone else, even if they have the same condition as you.
- Do not stop taking PHYSIOTENS suddenly, or change the dosage, without checking with your doctor.
Driving or using machines
Be careful before you drive or use any machines or tools until you know how PHYSIOTENS affects you.
PHYSIOTENS may cause drowsiness, dizziness or light-headedness in some people. If you have any of these symptoms, do not drive, operate machinery or do anything else that could be dangerous.
Drinking alcohol
You should avoid drinking alcohol when taking PHYSIOTENS.
The effect of taking alcohol with PHYSIOTENS has not been studied. Ask your doctor for advice.
Looking after your medicine
Keep your tablets in the original pack until it is time to take them. If you take the tablets out of the box they may not keep well.
Store it in a cool dry place below 25°C away from moisture, heat or sunlight.
Do not store it:
- in the bathroom or near a sink, or
- in the car or on window sills.
Keep it where young children cannot reach it. A locked cupboard at least one-and-a-half-metres above the ground is a good place to store medicines.
Getting rid of any unwanted medicine
If you no longer need to take this medicine or it is out of date, take it to any pharmacy for safe disposal.
Do not take this medicine after the expiry date.
6. Are there any side effects?
PHYSIOTENS helps most people with high blood pressure, but it may have unwanted side effects in a few people.
All medicines can have side effects. If you do experience any side effects, most of them are minor and temporary. However, some side effects may need medical attention. Do not be alarmed by this list of possible side effects. You may not experience any of them.
See the information below and, if you need to, ask your doctor or pharmacist if you have any further questions about side effects.
Less serious side effects
| Less serious side effects | What to do |
| Speak to your doctor if you have any of these less serious side effects and they worry you. This list includes the more common side effects of your medicine. They are usually mild and short-lived. |
Serious side effects
| Serious side effects | What to do |
| Tell your doctor as soon as possible if you notice any of these symptoms. This list includes serious side effects that may require medical attention. Serious side effects are rare. |
| Call your doctor straight away, or go straight to the Emergency Department at your nearest hospital if you notice any of these serious side effects. This list includes very serious side effects. You may need urgent medical attention. These side effects are rare. |
Tell your doctor or pharmacist if you notice anything else that may be making you feel unwell.
Other side effects not listed here may occur in some people.
Reporting side effects
After you have received medical advice for any side effects you experience, you can report side effects to the Therapeutic Goods Administration online at www.tga.gov.au/reporting-problems. By reporting side effects, you can help provide more information on the safety of this medicine.
Always make sure you speak to your doctor or pharmacist before you decide to stop taking any of your medicines.
7. Product details
This medicine is only available with a doctor's prescription.
What PHYSIOTENS contains
| Active ingredient (main ingredient) | PHYSIOTENS contains either 200 micrograms or 400 micrograms of moxonidine |
| Other ingredients (inactive ingredients) |
|
| Potential allergens | sugars as lactose |
Do not take this medicine if you are allergic to any of these ingredients.
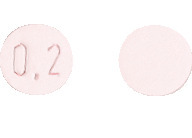
What PHYSIOTENS looks like
PHYSIOTENS 200 micrograms tablets are pale pink, round, biconvex, film-coated tablets, imprinted 0.2 on one side (AUST R 114119). Packs of 30 tablets.
PHYSIOTENS 400 micrograms tablets are dull red, round, biconvex, film-coated tablets, imprinted 0.4 on one side (AUST R 114121). Packs of 30 tablets.
Who distributes PHYSIOTENS
Viatris Pty Ltd
Level 1, 30 The Bond
30-34 Hickson Road
Millers Point NSW 2000
www.viatris.com.au
Phone: 1800 274 276
PHYSIOTENS is made in France.
PHYSIOTENS® is a Viatris company trade mark
This leaflet was prepared in February 2022.
PHYSIOTENS_cmi\Feb22/00
Published by MIMS March 2022



 The combination of hydrochlorothiazide and moxonidine was evaluated in a further placebo controlled, double blind and prospectively randomized trial. The study comprised a total of 161 randomized patients: 37 received moxonidine 400 microgram, 40 received hydrochlorothiazide 25 mg, 42 received the combination 400 microgram/25 mg and 41 received placebo, all once daily. Sitting systolic and diastolic blood pressures at trough after eight weeks treatment were statistically significantly reduced for all active treatment arms versus placebo. Furthermore, the difference of the combination for sitting diastolic blood pressure was statistically significant in favour of the combination for both monotherapies. The incidence of treatment emergent adverse events did not differ significantly between groups: 32.5% with moxonidine, 25% with HCT, 30% with the combination and 23% with placebo. See Table 3.
The combination of hydrochlorothiazide and moxonidine was evaluated in a further placebo controlled, double blind and prospectively randomized trial. The study comprised a total of 161 randomized patients: 37 received moxonidine 400 microgram, 40 received hydrochlorothiazide 25 mg, 42 received the combination 400 microgram/25 mg and 41 received placebo, all once daily. Sitting systolic and diastolic blood pressures at trough after eight weeks treatment were statistically significantly reduced for all active treatment arms versus placebo. Furthermore, the difference of the combination for sitting diastolic blood pressure was statistically significant in favour of the combination for both monotherapies. The incidence of treatment emergent adverse events did not differ significantly between groups: 32.5% with moxonidine, 25% with HCT, 30% with the combination and 23% with placebo. See Table 3.

