What is in this leaflet
This leaflet answers some common questions about Aldomet. It does not contain all the available information.
It does not take the place of talking to your doctor or pharmacist.
All medicines have risks and benefits. Your doctor has weighed the risks of you taking Aldomet against the benefits they expect it will have for you.
If you have any concerns about taking this medicine, ask your doctor or pharmacist.
Keep this leaflet with the medicine. You may need to read it again.
What it is used for
Aldomet lowers high blood pressure, which doctors call hypertension.
Everyone has blood pressure. This pressure helps get your blood all around your body. Your blood pressure may be different at different times of the day, depending on how busy or worried you are. You have hypertension (high blood pressure) when your blood pressure stays higher than is needed, even when you are calm and relaxed.
There are usually no symptoms of hypertension. The only way of knowing that you have hypertension is to have your blood pressure checked on a regular basis. If high blood pressure is not treated it can lead to serious health problems. You may feel fine and have no symptoms, but eventually hypertension can cause stroke, heart disease and kidney failure. Aldomet helps to lower your blood pressure.
Aldomet works by controlling impulses along certain nerve pathways. As a result, it relaxes and widens blood vessels so that blood passes through them more easily. This helps to lower blood pressure.
Ask your doctor if you have any questions about why Aldomet has been prescribed for you. Your doctor may have prescribed it for another purpose.
This medicine is only available with a doctor's prescription.
There is no evidence that it is addictive.
Before you take it
When you must not take it
Do not take Aldomet if:
- you have an allergy to Aldomet or any of the ingredients listed at the end of this leaflet
- you have taken Aldomet in the past and developed liver problems
- you have certain liver diseases, such as hepatitis or cirrhosis
- you are being treated for depression with medicines called monoamine oxidase inhibitors (MAOIs)
MAOIs include moclobemide, phenelzine and tranylcypromine. - the bottle shows signs of tampering
- the expiry date (EXP) printed on the pack has passed.
If you take this medicine after the expiry date has passed, it may not work.
If you are not sure whether you should start taking Aldomet, talk to your doctor.
Before you start to take it
Tell your doctor if you are pregnant, intend to become pregnant, are breast-feeding or intend to breast-feed. Your doctor will discuss the possible risks and benefits of using Aldomet during pregnancy and breast-feeding. Aldomet passes into breast milk.
Tell your doctor if you have or have had any of the following medical conditions:
- angina
- liver disease
- phaeochromocytoma or paraganglioma. (a rare tumour of the adrenal gland, which sits near the kidney), or if you are suspected of having this
- are undergoing dialysis
- porphyria. (a rare blood pigment disorder)
Tell your doctor if you are allergic to any other medicines or any foods, preservatives or dyes.
If you have not told your doctor about any of the above, tell them before you take any Aldomet.
Taking other medicines
Tell your doctor or pharmacist if you are taking any other medicines, including medicines that you buy without a prescription from a pharmacy, supermarket or health food shop.
Some medicines should not be taken with Aldomet. These include:
- medicines used to treat depression such as moclobemide, phenelzine and tranylcypromine.
Some medicines and Aldomet may interfere with each other. These include:
- other medicines for high blood pressure
- lithium, a medicine used to treat mood swings and some types of depressions
- iron supplements and multivitamins containing iron.
These medicines may be affected by Aldomet or may affect how well it works. You may need different amounts of your medicine, or you may need to take different medicines.
Your doctor or pharmacist has more information on medicines to be careful with or to avoid while taking Aldomet.
How to take it
Follow all directions given to you by your doctor carefully. They may differ from the information contained in this leaflet.
How much to take
Your doctor will tell you how many tablets you need to take each day.
This depends on your condition and whether you are taking any other medicines.
If you do not understand the instructions on the box, ask your doctor or pharmacist for help.
How to take it
Swallow the tablets whole with a glass of water or other liquid.
When to take it
Take your medicine at about the same time each day, unless your doctor tells you otherwise.
If you are taking it twice a day, take the tablets at breakfast time and dinner time - that is, about 12 hours apart.
If you are taking it three times a day, take the tablets about 8 hours apart.
Taking your tablets at the same time each day will have the best effect on your blood pressure. It will also help you remember when to take the tablets.
It does not matter whether you take Aldomet before or after food.
How long to take it
Continue taking Aldomet for as long as your doctor tells you. This medicine helps to control your high blood pressure but does not cure it. Therefore it must be taken every day.
If you forget to take it
If it is almost time for your next dose, skip the dose you missed and take your next dose when you are meant to. Otherwise, take it as soon as you remember, and then go back to taking your tablets as you would normally.
If you are not sure whether to skip the dose, talk to your doctor or pharmacist.
Do not take a double dose to make up for the dose that you missed.
If you have trouble remembering to take your tablets, ask your pharmacist for some hints.
If you take too much (overdose)
Immediately telephone your doctor or Poisons Information Centre (telephone 13 11 26) for advice, or go to Accident and Emergency at your nearest hospital if you think that you or anyone else may have taken too much Aldomet. Do this even if there are no signs of discomfort or poisoning. You may need urgent medical attention.
If you take too many tablets, you will probably feel light-headed and dizzy or you may faint. You may also feel very drowsy, weak, may have a slow heart rate, be constipated, have abdominal bloating, gas in the stomach or bowel, diarrhoea, nausea or vomiting.
While you are taking it
Things you must do
Have your blood pressure checked when your doctor says to make sure Aldomet is working.
If you feel light-headed, dizzy or faint, get up slowly when getting out of bed or standing up. You may feel light-headed or dizzy when you begin to take Aldomet or if the dose is increased. This is because your blood pressure is falling suddenly. Standing up slowly, especially when you get up from bed or chairs, will help your body get used to the change in position and blood pressure. The problem usually goes away after the first few days.
If you are about to be started on any new medicine tell your doctor and pharmacist that you are taking Aldomet.
If you plan to have surgery (even at the dentist) that needs a general anaesthetic, tell your doctor or dentist that you are taking Aldomet. Your blood pressure may drop suddenly.
If you are having blood and urine tests, tell your doctor you are taking Aldomet. Aldomet may interfere with some of these tests giving incorrect results.
If you develop fever, tell your doctor. Your doctor may need to do some blood tests to make sure Aldomet is not affecting your liver or blood.
Tell your doctor if you are to have a blood transfusion, that you are taking Aldomet or have taken it in the past few months. Aldomet may interfere with the tests used to decide which blood group you receive.
Make sure you drink enough water during exercise and hot weather when you are taking Aldomet, especially if you sweat a lot. If you do not drink enough water while taking it, you may faint or feel light-headed or sick. This is because your body doesn't have enough fluid and your blood pressure is low. If you continue to feel unwell, tell your doctor.
Things you must not do
Do not give Aldomet to anyone else, even if they have the same condition as you.
Things to be careful of
Be careful driving or operating machinery until you know how Aldomet affects you. Aldomet may cause dizziness, light headedness, drowsiness or sleepiness, especially after the first few doses and if the dose is increased. Make sure you know how you react to it before you drive a car, operate machinery, or do anything else that could be dangerous if you are dizzy or drowsy. If you drink alcohol, dizziness or drowsiness may be worse.
Things that would be helpful for your blood pressure
Some self help measures suggested below may help your condition. Talk to your doctor or pharmacist about these measures and for more information.
Alcohol - your doctor may advise you to limit your alcohol intake.
Diet - eat a healthy diet which includes plenty of fresh vegetables, fruit, bread, cereals and fish. Also eat less fat and sugar.
Exercise - regular exercise helps to reduce blood pressure and helps the heart get fitter, but it is important not to overdo it. Walking is good exercise, but try to find a route that is fairly flat.
Before starting any exercise, ask your doctor about the best kind of programme for you.
Salt - your doctor may advise you to watch the amount of salt in your diet. To reduce your salt intake you should avoid using salt in cooking or at the table.
Smoking - your doctor may advise you to stop smoking or at least cut down.
Weight - your doctor may suggest losing some weight to help lower your blood pressure. Some people may need a dietician's help to lose weight.
Side Effects
Tell your doctor or pharmacist as soon as possible if you do not feel well while you are taking Aldomet.
Aldomet helps most people with high blood pressure, but it may have unwanted side effects in a few people. All medicines can have side effects. Sometimes they are serious, most of the time they are not. You may need medical treatment if you get some of the side effects.
Ask your doctor or pharmacist to answer any questions you may have.
Tell your doctor if you notice any of the following and they worry you:
- dizziness
- light-headedness
- drowsiness
- headache
- weakness.
These are all mild side effects of Aldomet and may disappear with continued treatment. They may also occur if the dose is increased.
Tell your doctor immediately if you notice any of the following:
- fever shortly after starting to take Aldomet, for example, within the first 3 months
- yellowing of the skin and eyes, also called jaundice
- darker urine than normal due to liver problems
- pale stools
- swelling of the feet or lower legs
- nightmares, feeling strange or depressed
- signs of frequent or worrying infections such as fever, severe chills, sore throat or mouth ulcers
- bruising more easily than normal
- signs of anaemia, such as tiredness, being short of breath, and looking pale
- numbness, tingling, pain, or weakness in your hands or feet
- itchy skin rash or other skin problems
- a slow heart beat or pulse
- worsening of angina (chest pain)
- larger breasts than normal, especially in men.
These are all serious side effects. You may need urgent medical attention. Serious side effects are rare.
Other side effects not listed above may also occur in some patients. Tell your doctor if you notice anything else that is making you feel unwell.
Do not be alarmed by this list of possible side effects. You may not experience any of them.
After taking it
Storage
Keep your tablets in the bottle until it is time to take them. If you take the tablets out of the bottle they may not keep well.
Keep it in a cool dry place where the temperature stays below 30°C.
Do not store it or any other medicine in the bathroom or near a sink. Do not leave it in the car or on window sills. Heat and dampness can destroy some medicines.
Keep it where children cannot reach it. A locked cupboard at least one-and-a-half metres above the ground is a good place to store medicines.
Disposal
If your doctor tells you to stop taking the tablets or the tablets have passed their expiry date, ask your pharmacist what to do with any that are left over.
Product description
What it looks like
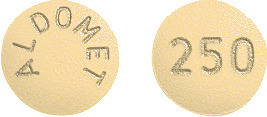
Aldomet is a yellow, round tablet with '250' marked on one side and 'ALDOMET' on the other side.
A bottle contains 100 tablets.
Ingredients
Active ingredient:
Each tablet contains 250 mg methyldopa.
Inactive ingredients:
- carnauba wax
- silica - colloidal anhydrous
- citric acid - anhydrous
- magnesium stearate
- hypromellose
- sodium calcium edetate
- propylene glycol
- ethylcellulose
- talc - purified
- guar gum
- titanium dioxide
- cellulose - powdered
- iron oxide red
- quinoline yellow aluminium lake
Aldomet does not contain lactose, sucrose, gluten or tartrazine.
Sponsor
Aspen Pharmacare Australia Pty Ltd
34-36 Chandos Street
St Leonards NSW 2065
Australian Registration Number:
AUST R 34361
Date of Revision: April 2015
Published by MIMS September 2017