What is quality improvement?
- Quality improvement (QI) involves making changes to your practice to achieve optimal safety and health outcomes for patients.
- The changes should be consistent with best practice standards, particularly for clinical conditions.
- QI can target any part of the health care service provided by your practice, from day-to-day operations such as scheduling appointments, through to the clinical knowledge and performance of health professionals.
- QI often involves activities that gather qualitative or quantitative clinical information about your practice and its health professionals. This information then helps to decide how to make changes.
- Patient clinical care data is a key source of quantitative clinical information.
- This data can be collected and analysed compared to best practice standards to give health professionals feedback about their performance as part of a clinical audit.
What are interventions?
Interventions are activities and actions that help address clinical problems and achieve quality improvement in your practice.
Each intervention is designed to address specific, different causes of clinical problems. Matching the correct intervention to the causes of the clinical problem can increase the chances of achieving successful quality improvement.
What is a clinical audit?
A clinical audit is one of the most effective quality improvement interventions. It gives health professionals in your practice a summary of their past and current performance compared to best practice standards. The comparison is based on data that is usually measured over a specific number of months or years.1-3
A clinical audit is a process or cycle made up of steps that work through auditing data, feedback to health professionals and implementing change. Alternative names for clinical audit found in the literature are ‘clinical performance feedback’ and ‘audit and feedback’.1,3
How to do a clinical audit
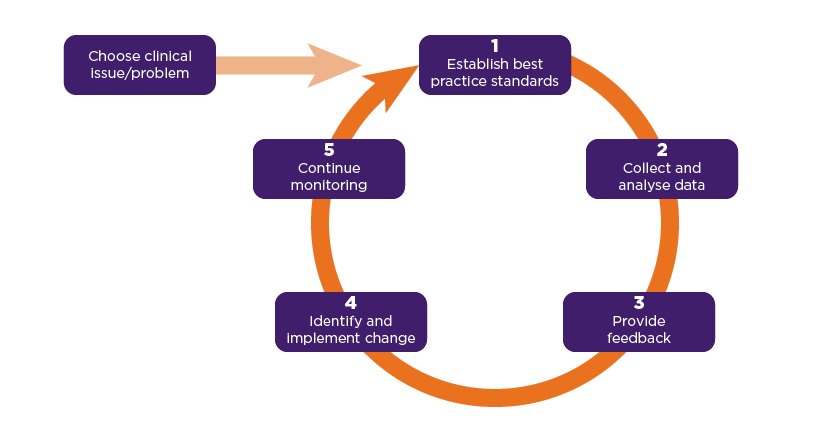
The clinical audit process has commonly accepted components. Once the clinical issue or problem has been identified, the process is usually described as a cycle that includes five steps.1,4,5
- Establish best practice standards
- Collect and analyse data
- Provide feedback
- Identify and implement change
- Continue monitoring
After these five steps, the cycle starts again at Step 1, in an iterative process of quality improvement.
Clinical audit cycle1,5
Each of the five steps of the clinical audit cycle has its own key components. You may find it helpful to look at Chronic non-cancer pain: opioids prescribing, an example of a clinical audit developed by NPS MedicineWise, at the same time as reading about the five steps.
Step 1. Establish best practice standards based on the evidence
- Identify key guidelines and recommendations
- With members of your practice, decide which parts of best practice standards and performance are the highest priorities based on your practice population
- Identify guideline recommendations that are in the health professional’s control to change. Sometimes an issue can be really important, but outside your control
- Identify improvement measures for collecting and analysing data about patients
Step 2. Collect and analyse data that relate to the best practice standards
- Identify how the data can be most efficiently and accurately collected and analysed (eg, can you draw a report from your system?, do you need to collect data?)
- Measure baseline data for performance before providing feedback
- Choose comparator performance that reinforces desired change/best practice standard (eg, colleagues’ performance, regional performance)
Step 3. Provide feedback about the data to the health professionals
- Provide feedback as soon as possible and at a frequency informed by the number of new patient cases (eg, a less common condition may require a longer reporting period)
- Guide the health professionals' reflection when receiving the feedback – include positive messaging as well as negative
Step 4. Identify and implement changes in performance
- With members of your practice, identify what needs to be done, based on the data (eg, education, process change, patient follow-up)
- Focus on best practice standards that are in the health professionals' control to change
- Identify barriers that block implementation of change and what can be done to overcome them
Step 5. Continue monitoring through further data collection and analysis
- Be iterative and learn from the previous steps to improve the data collection and analysis
Types of clinical audit
Different types of clinical audit can be done. Here are some elements to consider when thinking about the type of clinical audit your practice will benefit from:5
- Your audience: Is the feedback targeted to each individual health professional separately, or to a group or team such as a medical practice? Sometimes you will want to work on your overall practice performance, and other times individuals will want to reflect on their individual prescribing.
- Data availability: Is it based on medical records or on self-reporting by health professionals? You may want to select an audit that will have low administrative burden.
- Additional interventions: Does the clinical audit need other activities to help drive change? For example, do you also need to deliver educational or patient resources?
- Delivery mechanism: Will the feedback be delivered verbally, via paper or online, such as by email or the desktop clinical information system (CIS)? Often you can use multiple methods, which the literature suggests will increase your likelihood of success.
- Operating considerations: What is the budget and timeframe? How can you plan for multiple rounds of clinical audit to show the health professionals how they are going?
- Business considerations: How does the clinical audit fit within the broader business model, or clinical strategy? For example, do you have clinical meetings every month or quarter? How can you align clinical audits with this to create a self-sustaining system?
- Incentives: Is the clinical performance that is being addressed part of a mandated requirement such as by the Department of Health? For example, how can you use this QI Hub to support your Practice Incentives Program (PIP) Quality Improvement (QI) work?
Examples
NPS MedicineWise regularly provides clinical audits (called Practice Reviews) as part of its programs for quality use of medicines and tests (QUMT). The audience for these clinical audits is made up of individual GPs. Here are some examples:
When to do a clinical audit
A clinical audit has the benefit of providing objective data on discrepancies between past and current performance and best practice standards. It also enables comparisons between peers. This can provide motivation for health professionals to act if they are not performing according to best practice standards.5
A clinical audit is suitable for your practice if:5
- the clinical issue/problem relates to health professionals overestimating their performance or underestimating the issue/problem
- there is a clear best practice standard and data based on an improvement measure for the clinical issue/problem that can be collected and analysed
- the health professionals receiving feedback are empowered to implement change required to achieve improvement. For example, if senior prescribers are setting an underperforming standard, junior prescribers may feel less empowered and under pressure to comply with them.
Motivation alone may not be enough to lead to improvement. Clear and agreed standards for performance are necessary, but if the standards are too aggressive, the task may seem unreasonable or impossible. This will reduce motivation. For example, if the standard is to reduce prescribing from 50% to 2%, health professionals may lose motivation to change at all.5
How effective is clinical audit?
A 2012 Cochrane reviewed 140 studies of clinical audit (‘audit and feedback’ was the term used). Most of the studies were with doctors, some were with nurses or pharmacists. The clinical performance ranged across different areas, including proper use of treatments or laboratory tests and improving the overall management of patients with chronic disease such as heart disease or diabetes.3
After excluding studies at high risk of bias, an analysis of 49 studies found moderate quality evidence for a 4.3% absolute increase (interquartile range (IQR) 0.5% to 16.0%) in health professionals’ compliance with standards (‘desired practice’).3
At first glance 4.3% may seem like a low impact. However, when applied to a large group of health professionals, the benefits can be substantial, such as adverse drug events avoided for patients or millions of dollars saved for the health budget.5
A 2016 review identified a practical list of 15 suggestions that are believed to be associated with optimising effectiveness of clinical audit. These suggestions are intended to provide practical guidance when planning and designing clinical audits.6
Further information
- Ivers N, Jamtvedt G, Flottorp S, et al. Audit and feedback: effects on professional practice and healthcare outcomes. Cochrane Database Syst Rev 2012
- Brehaut JC, Colquhoun HL, Eva KW, et al. Practice feedback interventions: 15 suggestions for optimizing effectiveness. Ann Intern Med. 2016 Mar 15;164(6):435-41.
References
- Royal Australian College of General Practitioners. QI&CPD Program: 2017–19 triennium handbook for general practitioners. East Melbourne: Royal Australian College of General Practitioners, 2016, (accessed November 11 2019).
- Ivers NM, Sales A, Colquhoun H, et al. No more 'business as usual' with audit and feedback interventions: towards an agenda for a reinvigorated intervention. Implement Sci 2014;9:14.
- Ivers N, Jamtvedt G, Flottorp S, et al. Audit and feedback: effects on professional practice and healthcare outcomes. Cochrane Database Syst Rev 2012:CD000259.
- University Hospitals Bristol Clinical Audit Team. What is clinical audit? Bristol, UK: University Hospitals Bristol, 2009, (accessed November 11 2019).
-
London J. A practical guide to audit and feedback. In: Weekes L, ed. Improving sse of medicines and medical tests in primary care. Singapore: Springer Nature, 2019.
- Brehaut JC, Colquhoun HL, Eva KW, et al. Practice feedback interventions: 15 suggestions for optimizing effectiveness. Ann Intern Med 2016;164:435-41.
Best practice standards, improvement measures and data
The performance of health professionals can be compared to best practice standards for clinical conditions.
For each clinical condition listed below, you will find information about:
- Best practice standards
- Improvement measures of performance
- How to collect patient clinical data
- How to use data collected
- Where to find resources
- CPD options
Opioids for chronic non-cancer pain

Opioids have a limited role in chronic non-cancer pain management. They should only be trialled if first-line therapies including non-pharmacological treatments and non-opioid medicines haven't achieved enough improvement, and the benefits of opioids outweigh the harms for the patient.
Asthma

Asthma is a common, chronic respiratory disease. Management, which aims to relieve symptoms and prevent them from recurring, includes ongoing treatment with preventer medicines, regular medical review and support for people with asthma to self-manage their treatment and behaviours.
Heart failure

Heart failure has a poor prognosis, including a high rate of hospitalisation and mortality. Early diagnosis, classification of heart failure, optimal pharmacological management, self-management and patient education can help patients stay out of hospital and lead better, longer lives.