What is in this leaflet
Read this leaflet carefully before taking your medicine. This leaflet answers some common questions about atenolol. It does not contain all the available information. It does not take the place of talking to your doctor or pharmacist.
The information in this leaflet was last updated on the date listed on the last page. Some more recent information on the medicine may be available. You should ensure that you speak to your pharmacist or doctor to obtain the most up to date information on the medicine.
All medicines have risks and benefits. Your doctor has weighed the risk of you taking atenolol against the benefits it is expected to have for you.
If you have any concerns about taking this medicine, ask your doctor or pharmacist.
Keep this leaflet with the medicine. You may want to read it again.
What this medicine is used for
The name of your medicine is APO-Atenolol. It contains the active ingredient, atenolol.
Atenolol is used to:
- lower high blood pressure (hypertension)
- prevent angina (chest pain or discomfort)
- treat an irregular heart beat or rhythm, also called arrhythmia
- reduce your risk of heart complications following a heart attack.
Hypertension:
All people have blood pressure. This pressure helps to push blood all around your body. Your blood pressure changes during the day, depending on how busy you are or how you are feeling.
You have hypertension (high blood pressure) when your blood pressure stays higher than is needed, even when you are calm and relaxed. Regular blood pressure checks are the only way of knowing that you have hypertension. There are usually no symptoms and you may feel fine. If hypertension is not treated, serious health problems such as stroke, heart disease and kidney failure may occur.
Atenolol helps to lower your blood pressure.
Angina:
Angina is a pain or uncomfortable feeling in the chest, often spreading to the arms or neck and sometimes to the shoulders and back. This may be because there is not enough blood and oxygen getting to the heart. The pain of angina is usually brought on by exercise or stress, but can also occur at rest.
Atenolol helps prevent angina. It is not used to relieve a sudden attack of angina.
Irregular heart beat (arrhythmia):
Irregular heartbeat, also known as arrhythmia, means that there is a disturbance of the heart's normal rhythm or beat. Arrhythmias may be caused by a number of factors, including some heart diseases, an overactive thyroid gland, or chemical imbalances.
Atenolol helps restore your heart's normal rhythm.
Reducing heart complications after heart attack:
After a heart attack, you may have complications such as an irregular heart beat or an increased chance of having another heart attack.
Atenolol helps to prevent these complications from occurring.
Ask your doctor if you have any questions about why this medicine has been prescribed for you. Your doctor may have prescribed this medicine for another reason.
How it works
This medicine contains atenolol. Atenolol belongs to a group of medicines called beta-blockers. It decreases the heart's need for blood and oxygen and therefore reduces the amount of work the heart has to do. It widens the blood vessels in the body, causing blood pressure to fall. It also helps the heart to beat more regularly.
There is no evidence that this medicine is addictive.
It is available only with a doctor's prescription.
This medicine is not expected to affect your ability to drive a car or operate machinery, but make sure you know how it affects you before driving.
There is not enough information to recommend the use of this medicine for children.
Before you take this medicine
When you must not take it
Do not take this medicine if:
- you have or have had asthma (difficulty breathing, wheezing and coughing), bronchitis or other lung problems in the past.
- you have the following conditions:
- a history of allergic problems, including hayfever. Symptoms of an allergic reaction may include skin rash, itchiness, shortness of breath, swelling of the face, lips or tongue, muscle pain or tenderness or joint pain
- a very slow heart beat (less than 45-50 beats per minute)
- a severe blood vessel disorder causing poor circulation in the arms and legs
- certain other problems with your heart
- phaeochromocytoma (a rare tumour of the adrenal gland), which is not being treated with other medicines
- low blood pressure (hypotension)
- too much acid in your blood (metabolic acidosis).
- you are receiving:
- certain anaesthetics for medical or dental procedures
- emergency treatment for shock or low blood pressure
- any other beta blocker medicines
- you have an allergy or have had a hypersensitivity reaction to atenolol or any of the ingredients mentioned at the end of this leaflet, or any other beta blocker medicine
- you are pregnant or breast feeding, or if there is a chance that this may occur.
Your doctor will discuss the possible risks and benefits of using atenolol during pregnancy and breast feeding. Atenolol passes into breast milk and may therefore affect the breast-fed baby.
If you are not sure whether any of these apply to you, check with your doctor.
Do not use this product if the packaging is torn or shows signs of tampering
Do not use this product after the expiry date (EXP) printed on the pack. The medicine may not work as well after this date.
Do not use this product if the tablets change in appearance, colour or taste.
If it has expired or is damaged or does not seem quite right, return it to your pharmacist for disposal.
If you are not sure whether you should start taking atenolol, talk to your doctor.
Before you start to take it
Tell your doctor if you have allergies to:
- any other medicines including eye drops, or other beta-blocker medicines.
- any other substances, including foods, preservatives or dyes.
- insect stings
Atenolol may make allergies worse or make them harder to treat.
Tell your doctor if you have or have had any medical conditions, especially the following:
- heart problems
- diabetes
- an overactive thyroid (hyperthyroidism).
- kidney problems
- circulation problems
- phaeochromocytoma, which is being treated with other medicines
- a particular type of angina called prinzmetal angina or variant angina.
- any medical condition affecting your blood vessels.
Tell your doctor if you plan to become pregnant or breast-feed.
If you have not told your doctor about any of the above, tell them before you start taking atenolol.
Taking other medicines
Tell your doctor or pharmacist if you are taking any other medicines, including any that you buy without a prescription from your pharmacy, supermarket or health food shop.
The medicines below may be affected by atenolol, or may affect how well it works. It is especially important that you tell your doctor if you are taking any of the following:
- other beta-blocker medicines, including beta-blocker eye drops
- medicines used to treat high blood pressure or angina, or example verapamil, diltiazem, nifedipine, clonidine
- medicines to treat heart problems, such as disopyramide, quinidine, digoxin, amiodarone, guanethidine
- insulin and tablets used to treat diabetes
- certain medicines used to treat arthritis, pain, or inflammation, for example indomethacin or ibuprofen
- cold remedies
- medicines commonly used during surgery or in emergency situations (e.g. dopamine, adrenaline, noradrenaline and certain anaesthetics.
You may need to use different amounts of your medicine, or you may need to take different medicines.
Your doctor and pharmacist have more information on medicines to be careful with or avoid while taking atenolol.
Ask your doctor or pharmacist if you are not sure if you are taking any of these medicines.
How to take this medicine
Follow all directions given to you by your doctor or pharmacist carefully. They may differ from the information contained in this leaflet.
If you do not understand the instructions on the label, ask your doctor or pharmacist for help.
How much to take
Your doctor or pharmacist will tell you how many tablets you will need to take each day and how long to take them for. This depends on your condition and whether or not you are taking any other medicines.
Hypertension:
The usual dose is from 50mg (1 tablet) up to 200mg (4 tablets) of atenolol daily. If your dose is 100mg or less, take it once a day. If you need to take more than 100mg (2 tablets), take half of your atenolol in the morning and the other half in the evening.
Angina or Irregular Heart Beat:
The usual dose is from 50mg (1 tablet) up to 100mg (2 tablets) taken as a single dose or half the dose in the morning and half at night.
Heart attack:
The usual dose is 50mg (1 tablet) of atenolol daily.
Certain people e.g. the elderly or those with kidney problems, may require a lower dose.
How to take it
Swallow the tablet(s) with a little fluid.
To break atenolol tablets into two equal halves place on a flat surface and press down on either side of break line with thumb and forefinger.
Your atenolol tablets may be provided in a calendar pack which is designed to remind you when to take this medication. To do this, take your first dose from the position marked "First Day". On the following day take the first tablet which is labelled with the appropriate day. When you have taken all doses in this pack, take your next atenolol prescription in the same way.
When to take it
Take your medicine at the same time every day. Taking your medicine at the same time each day will have the best effect. It will also help you remember when to take it.
It does not matter if you take it before or after food.
How long to take it for
Take your medicine every day.
Keep taking it until your doctor tells you to stop.
It helps to treat high blood pressure, irregular heartbeat, and heart attacks and prevent angina but does not cure it.
Make sure you have enough tablets to last over weekends and holidays.
Do not stop taking this medicine without checking with your doctor.
Your doctor may want you to gradually reduce the amount of atenolol you are taking. This should take place over a period of about 2 weeks before stopping completely. Do not stop suddenly as this may worsen your condition.
If you forget to take it
If you forget to take one or more doses of atenolol, and it is almost time for your next dose, skip the dose you missed and take your next dose when you are meant to. Otherwise, take it as soon as you remember, and then go back to taking your medicine as you would normally.
Do not take a double dose to make up for the dose that you missed. Do not take any more than your doctor prescribed for you. This may increase the chance of you getting an unwanted side effect.
If you are not sure what to do, ask your doctor or pharmacist.
If you have trouble remembering to take your medicine, ask your pharmacist for some hints.
If you take too much (overdose)
Immediately telephone your doctor or the Poisons Information Centre (Tel: 13 11 26 for Australia) or go to the Accident and Emergency Department at the nearest hospital, if you think that you or anyone else may have taken too much atenolol.
Do this even if there are no signs of discomfort or poisoning. You may need urgent medical attention.
If you take too much atenolol, you may faint, feel dizzy or light-headed, wheeze or have difficulty breathing. You may also have a very slow heart beat.
While you are taking this medicine
Things you must do
Always follow your doctor's instructions carefully.
Keep all of your doctor's appointments so that your progress can be checked.
Tell any other doctors, dentists and pharmacists who are treating you that you are taking atenolol.
Tell your doctor immediately if you become pregnant while taking atenolol.
If you are about to start taking a new medicine, remind your doctor and pharmacist that you are taking atenolol.
If you are going to have surgery (even at the dentist), tell your surgeon, anaesthetist or dentist that you are taking atenolol. Atenolol may affect some of the medicines used during surgery, or may cause your blood pressure to drop suddenly.
If you have to have any medical tests while you are taking atenolol, tell your doctor. Atenolol may affect the results of some tests.
Drink lots of water when exercising and during hot weather when taking atenolol, especially if you sweat a lot. If you do not drink enough water while taking atenolol, you may feel faint, light-headed or sick. The recommended healthy minimum water intake is 6-8 glasses a day.
Tell your doctor immediately if you have an allergic reaction to foods, medicines or insect stings. Atenolol can cause allergic reactions to be worse and harder to treat.
If you have diabetes, check your blood sugar level regularly and report any changes to your doctor. Atenolol may affect your diabetes. It may hide the symptoms of low blood sugar levels, such as a fast heart beat. It may also take longer for your blood sugar level to get back to normal even if you follow the usual treatment for diabetes. Your diabetic medicines may have to be changed or the doses
If you keep having angina attacks, or have more of them whilst taking atenolol, tell your doctor. Atenolol is used to help prevent angina, so your angina attacks should become less severe and occur less often.
Things you must not do
Do not stop taking your medicine, or lower the dosage, without checking with your doctor.
Do not take any new medicines with atenolol, unless your doctor has told you to.
Do not take your medicine to treat any other complaints unless your doctor or pharmacist tells you to.
Do not give this medication to anyone else, even if their symptoms seem similar to yours.
Things to be careful of
Be careful driving or operating machinery until you know how atenolol affects you. As with other beta blocker medicines, atenolol may cause dizziness, faintness, fatigue or light-headedness in some people. Make sure you know how you react to atenolol before you drive a car, operate machinery, or do anything else that could be dangerous if you are dizzy or light-headed. If you have any of these symptoms stop driving, operating machinery or performing dangerous tasks.
If you drink alcohol, dizziness or light-headedness may be worse.
If this problem gets worse or continues, talk to your doctor.
To help your body get used to the change in blood pressure, the following hints may be useful:
- Stand up slowly when getting up from a chair or bed. This will allow your body get used to the change in position and blood pressure.
- If you feel dizzy, sit or lie down until you feel better.
- If you feel faint, sit down and put your head between your knees.
Be careful not to over-exercise when you first start taking atenolol. Atenolol helps prevent angina resulting from physical activity and exercise. You may be tempted to exercise too much. Talk to your doctor about how much exercise you can do.
Dress warmly during cold weather, especially if you will be outside for a long time (for example, when playing or watching sport in winter). Atenolol, like other beta-blocker medicines, may make you more sensitive to cold temperatures, especially if you have circulation problems. Beta-blockers tend to decrease blood circulation in the skin, fingers and toes.
Things that would be helpful for your blood pressure
The suggestions below may help your condition. Talk to your doctor or pharmacist about these measures and for more information.
Alcohol:
Your doctor may advise you to limit your alcohol intake.
Weight:
Your doctor may suggest losing some weight to help lower your blood pressure and help lessen the amount of work your heart has to do. Some people may need a dietician's help to lose weight.
Diet:
Eat a healthy low-fat diet which includes plenty of fresh vegetables, fruit, bread, cereals and fish. Also eat less fat and sugar.
Salt:
Your doctor may advise you to watch the amount of salt in your diet. To reduce your salt intake avoid using salt in cooking or at the table.
Side effects
Tell your doctor or pharmacist as soon as possible if you do not feel well while you are taking atenolol.
All medicines may have some unwanted side effects. Sometimes they are serious, but most of the time they are not. Your doctor has weighed the risks of using this medicine against the benefits he/she expects it will have for you.
Ask your doctor or pharmacist to answer any questions you may have.
Following is a list of possible side effects. Do not be alarmed by this list. You may not experience any of them.
Tell your doctor or pharmacist if you notice any of the following and they worry you:
- stomach upsets such as diarrhoea, constipation, abdominal pain or heartburn (indigestion).
- dry mouth, change in taste sensation
- dizziness, headache or buzzing or ringing in the ears, difficulty hearing
- slow or irregular heartbeat
- dry eyes, problems with vision
- runny or blocked nose
- difficulty sleeping, nightmares, vivid dreams
- skin reactions (e.g. rash, itching, worsening of psoriasis)
- cold fingers and toes
- increased hair loss.
- tingling, "pins and needles"
- sexual problems.
- weakness, fatigue, lack of energy
- feeling generally unwell
The above list includes the more common side effects. Mostly, these are mild.
Tell your doctor immediately if you notice any of the following:
- confusion or disorientation
- depression or mood changes or a worsening of these
- unusual thoughts, hallucinations (seeing, feeling or hearing things that are not there).
- dizziness or light-headedness (sometimes with fainting), especially on standing up, which may be due to low blood pressure.
- coldness, burning, numbness or pain in the arms and/or legs.
- irritated eyes (red, runny, itchy or dry), visual disturbances (e.g. blurred vision).
- difficulty in speaking.
- unsteadiness when walking.
These may be serious side effects. You may need urgent medical attention. Serious side effects are rare.
If any of the following happen, STOP taking atenolol, and tell your doctor immediately, or go to Accident and Emergency at your nearest hospital:
- shortness of breath, sometimes with tiredness, weakness and reduced ability to exercise, swelling of the feet or legs due to fluid build up
- unusual bruising or bleeding
- chest pain, changes in heart rate (fast, slow or irregular), palpitations
- chest tightness, wheezing, rattly breathing
- yellowing of the skin and/or eyes (jaundice)
- signs of a serious allergic reaction such as shortness of breath, wheezing or troubled breathing, swelling of the face, lips, mouth, throat or tongue which may cause difficulty in swallowing or breathing, or swelling of other parts of the body
These are very serious side effects. You may need urgent medical attention or hospitalisation. These side effects are very rare.
Other side effects not listed above may occur in some patients.
Tell your doctor or pharmacist if you notice anything that is making you feel unwell.
Storage and disposal
Storage
Keep atenolol in the original packaging until you need to take it. If you take the tablets out of their original packaging, they may not keep well.
Keep your tablets in a cool, dry place where the temperature will stay below 25°C.
Do not store the tablets or any other medicines in the bathroom or near a sink.
Do not leave the tablets in the car on hot days or on windowsills. Heat and dampness can destroy some medicines.
Keep the tablets where children cannot reach them. A locked cupboard at least one-and-a-half metres above the ground is a good place to store medicines.
Disposal
If your doctor or pharmacist tells you to stop taking this medicine or if it has passed its expiry date, ask your pharmacist what to do with any medicine that is left over.
Where to go for further information
Pharmaceutical companies are not in a position to give people an individual diagnosis or medical advice. Your doctor or pharmacist is the best person to give you advice on the treatment of your condition.
Product description
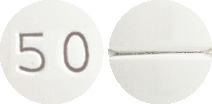
What APO-Atenolol looks like
50 mg tablets: white to off white, circular biconvex film coated tablets with "50" embossed on one side and break line on other side.
Blister packs or bottles containing 30 tablets.
*Not all pack sizes and/or types may be available.
Ingredients
Active Ingredient:
Each tablet contains 50mg of atenolol.
It also contains the following inactive ingredients:
- magnesium stearate
- maize starch
- sodium lauryl sulphate
- colloidal anhydrous silica
- sodium starch glycollate type A
- magnesium carbonate hydrate
- Hypromellose
- macrogol 6000
- titanium dioxide
- purified talc
Australian Registration Numbers
New formulation
APO-Atenolol 50 mg tablets (blister): AUST R 214939
APO-Atenolol 50 mg tablets (bottle): AUST R 214940
Sponsor
Apotex Pty Ltd
16 Giffnock Avenue
Macquarie Park NSW 2113
APO and APOTEX are registered trade marks of Apotex Inc.
This leaflet was prepared in
December 2020
Published by MIMS January 2021

 Molecular Formula: C14H22N2O3.
Molecular Formula: C14H22N2O3.