SUMMARY CMI
NOTEN®
Consumer Medicine Information (CMI) summary
The full CMI on the next page has more details. If you are worried about using this medicine, speak to your doctor or pharmacist.
1. Why am I using NOTEN?
NOTEN contains the active ingredient atenolol. NOTEN is used to lower high blood pressure, which is called hypertension, prevent angina, treat irregular heart rhythm or beat called arrhythmias and treat heart attacks, or reduce your risk of heart complications following a heart attack. For more information, see Section 1. Why am I using NOTEN? in the full CMI.
2. What should I know before I use NOTEN?
Do not use if you have ever had an allergic reaction to NOTEN or any of the ingredients listed at the end of the CMI.
Talk to your doctor if you have any other medical conditions, take any other medicines, or are pregnant or plan to become pregnant or are breastfeeding. For more information, see Section 2. What should I know before I use NOTEN? in the full CMI.
3. What if I am taking other medicines?
Some medicines may interfere with NOTEN and affect how it works.
A list of these medicines is in Section 3. What if I am taking other medicines? in the full CMI.
4. How do I use NOTEN?
- Follow all directions given to you by your doctor or pharmacist carefully.
- If you do not understand the instructions on the pack, ask your doctor or pharmacist for help.
More instructions can be found in Section 4. How do I use NOTEN? in the full CMI.
5. What should I know while using NOTEN?
| Things you should do |
|
| Things you should not do |
|
| Driving or using machines |
|
| Looking after your medicine |
|
For more information, see Section 5. What should I know while using? in the full CMI.
6. Are there any side effects?
Common side effects include stomach upsets such as diarrhea, constipation, abdominal pain or heartburn, dry mouth, change in taste sensation, dizziness, headache or buzzing or ringing in the ears, slow or irregular heartbeat, dry eyes, problems with vision, runny or blocked nose, difficulty sleeping, nightmares, skin reactions, cold fingers and toes, increased hair loss, tingling 'pins and needles' or walking unsteadily or sexual problems. Serious side effects include confusion or disorientation, depression or mood changes or a worsening of these, unusual thoughts, hallucinations, light-headedness or fainting which may be due to low blood pressure or yellowing of the skin and/or eyes. Very serious side effects include allergic reaction. For more information, including what to do if you have any side effects, see Section 6. Are there any side effects? in the full CMI.
FULL CMI
NOTEN®
Active ingredient(s): atenolol
Consumer Medicine Information (CMI)
This leaflet provides important information about using NOTEN. You should also speak to your doctor or pharmacist if you would like further information or if you have any concerns or questions about using NOTEN.
Where to find information in this leaflet:
1. Why am I using NOTEN?
2. What should I know before I use NOTEN?
3. What if I am taking other medicines?
4. How do I use NOTEN?
5. What should I know while using NOTEN?
6. Are there any side effects?
7. Product details
1. Why am I using NOTEN?
NOTEN contains the active ingredient atenolol. NOTEN is belongs to a group of medicines called beta-blockers.
It works by affecting the body's response to certain nerve impulses, especially in the heart. As a result, it decreases the heart's need for blood and oxygen and therefore reduces the amount of work the heart has to do. It widens the blood vessels in the body, causing blood pressure to fall. It also helps the heart to beat more regularly.
NOTEN is used to:
- lower high blood pressure, which is called hypertension
- prevent angina
- treat irregular heart rhythm or beat called arrhythmias treat heart attacks, or reduce your risk of heart complications following a heart attack
2. What should I know before I use NOTEN?
Warnings
Do not use NOTEN if:
- you are allergic to atenolol, or any of the ingredients listed at the end of this leaflet.
- any of the ingredients listed at the end of this leaflet.
- any other beta-blocker medicines.
- Always check the ingredients to make sure you can use this medicine
- you have or have had asthma (difficulty in breathing, wheezing and coughing), bronchitis or other lung problems in the past.
- a history of allergic problems, including hay fever.
Symptoms of an allergy may include rash, itching, watery eyes or sneezing. - a very slow heartbeat, less than 45 to 50 beats per minute
- a severe blood vessel disorder causing poor circulation in the arms and legs
- certain other heart conditions, such as heart failure
- phaeochromocytoma (a rare tumour of the adrenal gland) that is not being treated with other medicines
- low blood pressure, also called hypotension
- too much acid in your blood (metabolic acidosis)
- you are receiving certain anaesthetics for medical or dental procedures
- you are receiving emergency treatment for shock or very low blood pressure
Check with your doctor if you:
- have any other medical conditions. These include heart problems, diabetes, an overactive thyroid gland (called hyperthyroidism), kidney problems and any blood vessel disorders causing poor blood circulation in the arms and legs
- take any medicines for any other condition
- you have allergies to any other medicines (including eye drops), foods, preservatives, dyes or insect stings
During treatment, you may be at risk of developing certain side effects. It is important you understand these risks and how to monitor for them. See additional information under Section 6. Are there any side effects?
Pregnancy and breastfeeding
Check with your doctor if you are pregnant or intend to become pregnant.
Talk to your doctor if you are breastfeeding or intend to breastfeed.
3. What if I am taking other medicines?
Tell your doctor or pharmacist if you are taking any other medicines, including any medicines, vitamins or supplements that you buy without a prescription from your pharmacy, supermarket or health food shop.
Some medicines may interfere with NOTEN and affect how it works.
- other beta-blocker medicines
- medicines used to treat high blood pressure, angina or an irregular heartbeat, such as verapamil or clonidine
- medicines used to treat other heart problems
- insulin and other medicines used to treat diabetes
- medicines used to treat arthritis, pain or inflammation such as indometacin or ibuprofen
- medicines commonly used during surgery or in emergency situations such as adrenaline (epinephrine), noradrenaline (norepinephrine) and certain anaesthetics
Check with your doctor or pharmacist if you are not sure about what medicines, vitamins or supplements you are taking and if these affect NOTEN.
4. How do I use NOTEN?
How much to take
- Follow the instructions provided and use NOTEN until your doctor tells you to stop.
- If you do not understand the instructions on the label, ask your doctor or pharmacist for help
- Hypertension - The usual dose is from 50 mg (1 tablet) up to 200 mg (4 tablets) daily. If your dose is 100 mg or less, you may take it once a day. If you need to take more than 100 mg (2 tablets), take half of your dose in the morning and the other half at night.
- Angina or arrhythmia (irregular heart beat) - The usual dose is from 50 mg daily (1 tablet) as a single dose up to 100 mg (2 tablets) either as a single dose or a divided dose given as 1 tablet in the morning and 1 tablet at night.
- Heart attack - The usual dose is 50 mg (1 tablet) daily. Certain people such as the elderly or those with kidney problems may require a lower dose.
When to take NOTEN
- NOTEN should be used at the same time everyday
- It does not matter if you take NOTEN before or after food.
- Continue taking your medicine for as long as your doctor tells you to
How to take NOTEN
- Swallow NOTEN whole with a glass of water
If you forget to use NOTEN
NOTEN should be used regularly at the same time each day.
If it is less than six hours from when you missed your dose, take it as soon as you remember, and then go back to taking your tablets at the same time you would normally.
If it is more than six hours since your last dose, skip the dose you missed and take your next dose when you would normally.
Do not take a double dose to make up for the dose you missed.
If you are not sure what to do, ask your doctor or pharmacist.
If you use too much NOTEN
If you think that you have used too much NOTEN, you may need urgent medical attention.
You should immediately:
- phone the Poisons Information Centre
(Australia telephone 13 11 26) for advice, or - contact your doctor, or
- go to the Emergency Department at your nearest hospital.
You should do this even if there are no signs of discomfort or poisoning.
5. What should I know while using NOTEN?
Things you should do
Keep all of your doctor's appointments so that your progress can be checked
If you are about to be started on any new medicine, tell your doctor and pharmacist that you are taking NOTEN.
Tell any other doctors, dentists and pharmacists who treat you that you are taking this medicine.
Make sure you drink enough water in hot weather and during exercise while you are taking NOTEN, especially if you sweat a lot
Call your doctor straight away if you:
- become pregnant while taking this medicine, tell your doctor immediately
- have an allergic reaction to any foods, medicines or insect stings, tell your doctor immediately
- going to have surgery, tell your surgeon or dentist that you are taking this medicine
- have diabetes, check your blood sugar level regularly and report any changes to your doctor
- have angina and continue to have angina attacks or have more of them while you are taking this medicine
- If you feel light-headed, dizzy or faint when getting out of bed or standing up, get up slowly
- have to have any medical tests
Things you should not do
- Do not stop using this medicine suddenly
- Do not stop taking your medicine or lower the dose without checking with your doctor
- Do not take NOTEN to treat any other complaints unless your doctor tells you to
- Do not take NOTEN to treat any other complaints unless your doctor tells you to
- Do not take any new medicines with NOTEN unless your doctor has told you to
Things to be careful of
- Be careful not to over exercise when you first start taking NOTEN
- Dress warmly during cold weather, especially if you will be outside for a long time (for example, when playing or watching sports in winter).
Driving or using machines
Be careful before you drive or use any machines or tools until you know how NOTEN affects you.
NOTEN may cause dizziness, tiredness, light headedness or faintness in some people
Looking after your medicine
- Keep your tablets in the pack until it is time to take them
- Keep your tablets in a cool dry place where the temperature stays below 25°C
Follow the instructions in the carton on how to take care of your medicine properly.
Store it in a cool dry place away from moisture, heat or sunlight; for example, do not store it:
- in the bathroom or near a sink, or
- in the car or on window sills.
Keep it where young children cannot reach it.
Getting rid of any unwanted medicine
If you no longer need to use this medicine or it is out of date, take it to any pharmacy for safe disposal.
Do not use this medicine after the expiry date.
6. Are there any side effects?
All medicines can have side effects. If you do experience any side effects, most of them are minor and temporary. However, some side effects may need medical attention.
See the information below and, if you need to, ask your doctor or pharmacist if you have any further questions about side effects.
Less serious side effects
| Less serious side effects | What to do |
| Speak to your doctor if you have any of these less serious side effects and they worry you. |
Serious side effects
| Serious side effects | What to do |
| Call your doctor as soon as possible if you have any of these serious side effects |
Very serious side effects
| Very Serious side effects | What to do |
| Call your doctor straight away, or go straight to the Emergency Department at your nearest hospital if you notice any of these serious side effects. |
Tell your doctor or pharmacist if you notice anything else that may be making you feel unwell.
Other side effects not listed here may occur in some people.
Reporting side effects
After you have received medical advice for any side effects you experience, you can report side effects to the Therapeutic Goods Administration online at www.tga.gov.au/reporting-problems. By reporting side effects, you can help provide more information on the safety of this medicine.
Always make sure you speak to your doctor or pharmacist before you decide to stop taking any of your medicines.
7. Product details
This medicine is only available with a doctor's prescription.
What NOTEN contains
| Active ingredient (main ingredient) | atenolol |
| Other ingredients (inactive ingredients) | lactose monohydrate maize starch povidone microcrystalline cellulose colloidal anhydrous silica hydrogenated vegetable oil crospovidone sodium starch glycollate purified talc magnesium stearate. |
| Potential allergens | sulfites sugars as lactose |
Do not take this medicine if you are allergic to any of these ingredients.
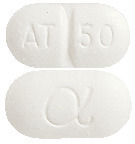
What NOTEN looks like
NOTEN tablets are a 10.5 mm x 5.5 mm white, normal convex, oblong tablet marked with AT/50 and α on the reverse. (AUST R 46250).
Who distributes NOTEN
Alphapharm Pty Ltd trading as Viatris
Level 1, 30 The Bond
30-34 Hickson Road
Millers Point NSW 2000
www.viatris.com.au
Phone: 1800 274 276
This leaflet was prepared in August 2023.
NOTEN® is a Viatris company trade mark
NOTEN_cmi\Aug23/00
Published by MIMS October 2023

 Chemical name: 2-[4-[(2RS)-2-hydroxy-3-[(1-methylethyl)amino]propoxy]phenyl]acetamide.
Chemical name: 2-[4-[(2RS)-2-hydroxy-3-[(1-methylethyl)amino]propoxy]phenyl]acetamide.