What is in this leaflet
This leaflet answers some common questions about Tranalpha.
It does not contain all the available information. It does not take the place of talking to your doctor or pharmacist.
All medicines have benefits and risks. Your doctor has weighed the risks of you taking Tranalpha against the benefits expected for you.
If you have any concerns about taking this medicine, talk to your doctor or pharmacist.
Keep this leaflet with your medicine. You may need to read it again.
What Tranalpha is used for
Tranalpha is used to treat:
- high blood pressure (hypertension)
- some heart conditions
There are usually no symptoms of hypertension. The only way of knowing that you have hypertension is to have your blood pressure checked on a regular basis. If high blood pressure is not treated it can lead to serious health problems. You may feel fine and have no symptoms, but eventually hypertension can lead to serious health problems, including stroke, heart disease and kidney failure. Tranalpha helps to lower your blood pressure.
Ask your doctor if you have any questions about why Tranalpha has been prescribed for you. Your doctor may have prescribed Tranalpha for another purpose.
How Tranalpha works
Tranalpha belongs to a group of medicines called angiotensin converting enzyme (ACE) inhibitors.
ACE inhibitors lower blood pressure by widening and relaxing your blood vessels, making it easier for the heart to pump blood around the body.
Widening of the blood vessels also increases the supply of blood and oxygen to the heart. By increasing the supply of oxygen to your heart, your heart does not have to work as hard.
Tranalpha is available only with a doctor's prescription.
There is no evidence that Tranalpha is addictive.
Tranalpha is not recommended for use in children as there have been no studies of its effects in children.
Before you take Tranalpha
When you must not take it
Do not take Tranalpha if you:
- are allergic (sensitive) reaction to trandolapril or medicines containing trandolapril or any of the ingredients listed at the end of this leaflet. Some of the symptoms of an allergic reaction may include skin rash, itching or hives, swelling of the face, lips, mouth, throat or other parts of the body, shortness of breath, wheezing or troubled breathing.
- have ever taken any other ACE inhibitor medicine, which caused your face, lips, tongue, throat, hands or feet to swell up, or made it hard for you to breathe.
- have had an allergic reaction to an ACE inhibitor before, you could be allergic to Tranalpha.
- you have a history of swelling of the face, lips, mouth, tongue, throat, hands or feet for no apparent reason.
Taking Tranalpha could cause this problem to happen again.
- are suffering from any obstruction that slows the flow of blood to the heart, such as narrowing of one of the valves in the heart (aortic stenosis)
- recently had severe or prolonged sickness or diarrhea
- have ever had the condition known as angioedema (a severe allergic skin condition)
- are undergoing haemodialysis or having your blood treated outside your body.
Taking Tranalpha could cause an allergic reaction.
- Are taking any of the following medications, or medications containing these ingredients:
- aliskiren (under certain conditions)
- neutral endopeptidase (NEP) inhibitors such as sacubitril and racecadotril
- sacubitril in combination with valsartan
Do not take this medicine if you are pregnant or plan to become pregnant. Tranalpha may affect your developing baby if you take it during pregnancy.
Tell your doctor if you are breastfeeding or wish to breastfeed. Tranalpha may pass into breast milk. It is recommended that you do not breastfeed while taking Tranalpha
Tranalpha must not be given to children. Safety and effectiveness in children have not been established.
Do not take this medicine after the expiry date printed on the pack or if the packaging is torn or shows signs of tampering. If it has expired or is damaged, return it to your pharmacist for disposal.
If you are not sure whether you should start taking this medicine, talk to your doctor.
Before you start to take it
Tell your doctor if you have allergies to:
- sulfites which are present in the Tranalpha capsule shell
- any other medicines
- any other substances, such as foods, preservatives or dyes.
Tell your doctor if you have allergies to any other medicines, foods, preservatives or dyes.
Tell your doctor if you have or have had any medical conditions, especially the following:
- kidney or liver problems
- regular dialysis, blood filtration or similar procedures
- high levels of potassium in your blood
- dizzy spells
- diabetes
- connective tissue disease
- are about to have surgery or general anaesthetic
- any heart conditions
If you have not told your doctor about any of the above, tell him/her before you start taking Tranalpha.
In patients of African descent, ACE inhibitors are less effective in lowering blood pressure than in Caucasian patients.
Tell your doctor if you if you have a family history of excessive swelling in the face, lips, mouth, tongue or throat.
Tell your doctor if you are following a very low salt diet.
Tell your doctor if you are about to receive desensitisation treatment for an allergy e.g. to insect stings.
Tell your doctor if you plan to become pregnant or breastfeed. Tranalpha should not be used during pregnancy or while you are breast-feeding.
Tell your doctor if you have an intolerance to any sugars. Gopten contains sugars (as lactose).
If you had not told your doctor about any of the above, tell them before you start taking Tranalpha.
Taking other medicines
Tell your doctor if you are taking any other medicines, including any that you buy with or without a prescription from a pharmacy, supermarket or health food shop.
Some medicines may be affected by Tranalpha or may affect how well it works. These include:
- any other high blood pressure medicines
- aliskiren
- neutral endopeptidase (NEP) inhibitors such as sacubitril or racecadotril
- diuretics, also known as 'fluid tablets', a medicine used to remove excess body fluids
- lithium and tricyclic antidepressants, medicines used to treat mood changes
- potassium supplements or large amounts of salt
- potassium - containing salt substitutes in your food (check the label)
- any other medication associated with increases in potassium (e.g. trimethoprim/sulfamethoxazole - an antibiotic)
- anti-inflammatory pain medicines used to treat arthritis, pain or fever
- any anti-diabetic medicine including insulin or vildagliptin (used to lower blood glucose)
- sympathomimetics which may be found in some decongestants, cough/cold remedies and asthma medicines
- antacids
- immunosuppressants, such as ciclosporin (medicines which lower the body's resistance to disease and treat or prevent organ transplant rejection)
- procainamide, (a medicine used to improve abnormal heart rhythms)
- allopurinol, (a medicine used to treat gout)
- cytostatic medicines, (medicines used to treat certain cancers)
- neuroleptic medicines, (medicines used to treat certain mental and emotional conditions)
- general anaesthetics
- injectable gold (sodium aurothiomalate), (a medicine used to treat rheumatoid arthritis).
- heparin (used to thin the blood)
These medicines may be affected by Tranalpha or may affect how well it works. Your doctor or pharmacist can tell you what to do if you are taking any of these medicines. They also have a more complete list of medicines to be careful with or avoid while taking Tranalpha.
How to take Tranalpha
How much to take
Your doctor will tell you how many capsules of Tranalpha you need to take each day. This depends on your condition and whether or not you are taking any other medicines.
The usual dosage is one or two capsules taken once daily, up to a maximum of 4 mg (two 2 mg capsules) once daily.
Dosage for older people over 65 years.
The usual starting dose for older people is less than that for younger adults. Your doctor will adjust the dose of Tranalpha, depending on how quickly your kidneys and liver can remove it from your body.
Follow all directions given to you by your doctor and pharmacist carefully. These directions may differ from the information contained in this leaflet.
If you do not understand the instructions on the box, ask your doctor or pharmacist for help.
How to take it
Swallow Tranalpha with water.
When to take it
Take Tranalpha at about the same time each day. Taking your capsules at the same time each day will have the best effect. It will also help you remember when to take the capsules.
It does not matter if you take Tranalpha before, during or after food.
If you need to take an antacid, take it at least 2 hours before or 2 hours after your dose of Tranalpha.
How long to take it for
Continue taking your medicine for as long as your doctor tells you to.
This medicine helps to control your condition, but does not cure it. It is important to keep taking your medicine even if you feel well.
If you forget to take it
If it is almost time for your next dose, skip the dose you missed and take your next dose when you are meant to.
Otherwise, take it as soon as you remember, and then go back to taking your capsules as you would normally.
Do not take a double dose to make up for the dose you missed. This may increase the chance of you getting an unwanted side effect.
If you are not sure what to do, ask your doctor or pharmacist.
If you have trouble remembering to take your medicine, ask your pharmacist for some hints.
If you take too much (overdose)
Immediately telephone your doctor or the Poisons Information Centre (telephone 13 11 26) for advice, or go to Accident and Emergency at the nearest hospital, if you think that you or anyone else may have taken too much Tranalpha. Do this even if there are no signs of discomfort or poisoning. You may need urgent medical attention.
If you take too much Tranalpha, you may feel dizzy, light-headed, weak, have palpitations or faint.
While you are taking Tranalpha
Things you must do
Have your blood pressure checked when your doctor says, to make sure Tranalpha is working.
If you become pregnant while taking Tranalpha tell your doctor immediately.
If you feel light-headed or dizzy after taking your first dose of Tranalpha, or when your dose is increased, tell your doctor immediately.
Tell your doctor if you have excessive vomiting and/or diarrhoea while taking Tranalpha. You may lose too much water and salt and your blood pressure may drop too much.
Drink plenty of water when you are using Tranalpha, especially if you sweat a lot (e.g. during hot weather or exercise). If you do not drink enough water while taking Tranalpha, you may faint or feel light-headed or sick. This is because your blood pressure is dropping suddenly. If you continue to feel unwell, tell your doctor.
Tell any other doctors, dentists and pharmacists who are treating you that you are taking Tranalpha.
If you are about to be started on any new medicines, tell your doctor, dentist or pharmacist that you are taking Tranalpha.
If you plan to have surgery that needs a general anaesthetic, tell your doctor or dentist that you are taking Tranalpha.
If you are about to have any blood tests, tell your doctor that you are taking Tranalpha. Tranalpha may interfere with the results of some tests.
Go to your doctor regularly for a check-up. Your doctor may occasionally do a blood test to check your potassium level in the blood and to see how your kidneys are working.
Things you must not do
Do not give Tranalpha to anyone else, even if they have the same condition as you.
Do not take Tranalpha to treat any other complaints unless your doctor tells you to.
Do not stop taking Tranalpha, or lower the dosage, without checking with your doctor.
Things to be careful of
If you feel light-headed, dizzy or faint, get up slowly when getting out of bed or standing up. Standing up slowly, especially when you get up from bed or chairs, will help your body get used to the change in position and blood pressure. If this problem continues or gets worse, talk to your doctor.
Be careful driving or operating machinery until you know how Tranalpha affects you. Tranalpha may cause dizziness, light-headedness or tiredness in some people. Make sure you know how you react to Tranalpha before you drive a car, operate machinery, or do anything else that could be dangerous if you are dizzy or light-headed.
If this occurs do not drive.
If you drink alcohol, dizziness or light-headedness may be worse.
Lifestyle measures that help reduce heart disease risk
By following these simple measures, you can further reduce the risk from heart disease.
- Quit smoking and avoid second-hand smoke.
- Limit alcohol intake.
- Enjoy healthy eating by:
- eating plenty of vegetables and fruit;
- reducing your saturated fat intake (eat less fatty meats, full fat dairy products, butter, coconut and palm oils, most take-away foods, commercially-baked products). - Be active. Progress, over time, to at least 30 minutes of moderate-intensity physical activity on 5 or more days each week. Can be accumulated in shorter bouts of 10 minutes duration. If you have been prescribed anti-angina medicine, carry it with you when being physically active.
- Maintain a healthy weight.
- Discuss your lifestyle and lifestyle plans with your doctor.
- For more information and tools to improve your heart health, call Heartline, the Heart Foundation's national telephone information service, on 1300 36 27 87 (local call cost).
Know warning signs of heart attack and what to do:
- Tightness, fullness, pressure, squeezing, heaviness or pain in your chest, neck, jaw, throat, shoulders, arms or back.
- You may also have difficulty breathing, or have a cold sweat or feel dizzy or light headed or feel like vomiting (or actually vomit).
- If you have heart attack warning signs that are severe, get worse or last for 10 minutes even if they are mild, call triple zero (000). Every minute counts.
Side effects
Tell your doctor or pharmacist as soon as possible if you do not feel well while you are taking Tranalpha.
Tranalpha helps most people with hypertension and some heart conditions, but it may have unwanted side effects in some people. All medicines can have side effects. Sometimes they are serious, most of the time they are not. You may need medical treatment if you get some of the side effects.
If you are over 65 years of age you may have an increased chance of getting side effects.
Ask your doctor or pharmacist to answer any questions you may have.
Tell your doctor if you notice any of the following and they worry you:
- light-headedness or dizziness
- nausea, vomiting, diarrhoea or stomach pains
- indigestion
- persistent dry cough
- headache
- unusual tiredness or weakness
- aching, tender or weak muscles not caused by exercise
- taste disturbance
These are the more common side effects of Tranalpha.
Tell your doctor immediately if you notice any of the following:
- fast or irregular heart beat, also called palpitations
- signs of worrying or frequent infections such as fever, severe chills, sore throat or mouth ulcers
- itchy skin rash or other skin problems
- symptoms of sunburn (such as redness, itching, swelling, blistering) which may occur more quickly than normal.
These may be serious side effects. You may need urgent medical attention. Serious side effects are rare.
If any of the following happen stop taking Tranalpha and tell your doctor immediately or go to Accident and Emergency at the nearest hospital:
- fainting within a few hours of taking Tranalpha
- swelling of the face, lips, mouth, tongue or throat which may cause difficulty in swallowing or breathing
- severe dizziness and confusion with visual disturbances and speech problems
- chest pain
- rapid, shallow breathing, cold clammy skin, a rapid, weak pulse, dizziness, weakness and fainting
These are very serious side effects. You may need urgent medical attention or hospitalisation. These side effects are very rare.
Do not be alarmed by this list of possible side effects. You may not experience any of them.
Other side effects not listed above may occur in some patients. Ask your doctor or pharmacist for more information about side effects. Tell your doctor promptly if you notice anything that is making you feel unwell.
If the condition persists or worsens, seek medical attention.
After taking Tranalpha
Storage
Keep your capsules in the pack until it is time to take them. If you take capsules out of the box they may not keep well.
Keep your capsules in a cool dry place where the temperature stays below 25°C.
Do not keep Tranalpha or any other medicine in the bathroom or near a sink.
Do not leave Tranalpha in the car on hot days or on window sills. Heat and dampness can destroy some medicines.
Keep it where children cannot reach it. A locked cupboard at least one-and-a-half metres above the ground is a good place to store medicines.
Disposal
If your doctor tells you to stop taking this medicine or the expiry date has passed, ask your pharmacist what to do with any medicine that is left over.
Product description
What it looks like
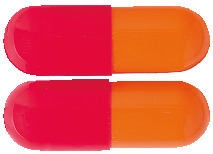
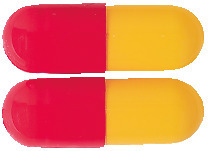
Tranalpha capsules are available in four different strengths. Each strength has a separate colour to distinguish it from the others.
- Tranalpha 0.5 mg: light scarlet & rich yellow capsules
- Tranalpha 1 mg: light scarlet & light orange capsules
- Tranalpha 2 mg: light scarlet capsules
- Tranalpha 4 mg: orange & scarlet capsules
Each pack contains 28 capsules.
Ingredients
The active ingredient in Tranalpha is trandolapril
- each Tranalpha 0.5 capsule contains 0.5 mg of trandolapril per capsule
- each Tranalpha 1 capsule contains 1 mg of trandolapril per capsule
- each Tranalpha 2 capsule contains 2 mg of trandolapril per capsule
- each Tranalpha 4 capsule contains 4 mg of trandolapril per capsule
Tranalpha also contains:
- dimeticone 350
- microcrystalline cellulose
- lactose monohydrate
- pregelatinised maize starch
- magnesium stearate
- silicon dioxide
- gelatin
- titanium dioxide
- erythrosine
- sodium lauryl sulfate (Tranalpha 0.5, Tranalpha 1 & Tranalpha 2)
- sunset yellow FCF (Tranalpha 0.5, Tranalpha 1 & Tranalpha 2)
- quinoline yellow (Tranalpha 0.5)
- iron oxide red (Tranalpha 4)
- iron oxide yellow (Tranalpha 4)
- iron oxide black (Tranalpha 4)
Tranalpha contains sugars (as lactose) and sulfites.
Tranalpha does not contain gluten, sucrose or tartrazine.
Supplier
Tranalpha is supplied by:
Alphapharm Pty Ltd
Level 1, 30 The Bond
30 - 34 Hickson Road
Millers Point NSW 2000
www.mylan.com.au
Australian registration numbers:
Australian registration numbers:
Tranalpha 0.5: AUST R 198992
Tranalpha 1: AUST R 198993
Tranalpha 2: AUST R 198994
Tranalpha 4: AUST R 198995
This leaflet was prepared on
14 November 2019.
Tranalpha_cmi\Nov19/00
Published by MIMS March 2020

 Less frequent adverse events (0.1% to 1%) possibly/probably related to treatment included: (see Table 2).
Less frequent adverse events (0.1% to 1%) possibly/probably related to treatment included: (see Table 2). In very rare cases, angioedema has occurred (see Section 4.4 Special Warnings and Precautions for Use).
In very rare cases, angioedema has occurred (see Section 4.4 Special Warnings and Precautions for Use).
 The following adverse events shown in Table 5 have been reported with ACE inhibitors as a class.
The following adverse events shown in Table 5 have been reported with ACE inhibitors as a class.
 The long-term use of trandolapril was associated with a reduction in all cause mortality (22%), largely cardiovascular mortality. Trandolapril was also associated with a 29% reduction in risk to progression of heart failure.
The long-term use of trandolapril was associated with a reduction in all cause mortality (22%), largely cardiovascular mortality. Trandolapril was also associated with a 29% reduction in risk to progression of heart failure. Chemical name: (2S, 3αR, 7αS)-1-[(S)-2-[[(1S)-1-(ethoxycarbonyl)-3-phenylpropyl]amino]propanoyl] octahydro - 1H-indole-2-carboxylic acid.
Chemical name: (2S, 3αR, 7αS)-1-[(S)-2-[[(1S)-1-(ethoxycarbonyl)-3-phenylpropyl]amino]propanoyl] octahydro - 1H-indole-2-carboxylic acid.