What is in this leaflet
This leaflet answers some common questions about CORTIMENT. It does not contain all the available information. It does not take the place of talking to your doctor or pharmacist.
All medicines have risks and benefits. Your doctor has weighed the risks of you taking CORTIMENT against the benefits they expect it will have for you.
If you have any concerns about taking this medicine, ask your doctor or pharmacist.
Keep this leaflet with the medicine. You may need to read it again.
What CORTIMENT is used for
CORTIMENT tablets are indicated in adults for induction of remission in patients with mild to moderate active ulcerative colitis (UC) where 5-ASA treatment is not sufficient or not tolerated.
CORTIMENT contains the active ingredient, budesonide. Budesonide belongs to a group of medicines called corticosteroids, which are used to help reduce inflammation.
CORTIMENT is used to treat inflammation of the large intestine (colon), which is an area commonly affected in UC. The tablets are designed to release the active ingredient, budesonide in a controlled manner along the colon.
Ask your doctor if you have any questions about why this medicine has been prescribed for you. Your doctor may have prescribed it for another reason.
CORTIMENT is available only with a doctor's prescription.
There is not enough information to recommend the use of this medicine for patients under the age of 18 years.
Before you take CORTIMENT
When you must not take it
Do not take CORTIMENT if you have an allergy to:
- any medicine containing budesonide
- any of the ingredients listed at the end of this leaflet
- peanut oil.
Some of the symptoms of an allergic reaction may include:
- rash, itching or hives on the skin
- shortness of breath, wheezing or difficulty breathing
- swelling of the face, lips, tongue or other parts of the body.
Do not take CORTIMENT if you are allergic to peanut oil or soy. CORTIMENT contains lecithin (of Soya origin).
Do not give CORTIMENT to children. CORTIMENT is intended for use by adult patients (older than 18 years). They are not recommended for children.
Do not take CORTIMENT after the expiry date printed on the pack or if the packaging is torn or shows signs of tampering. The expiry date refers to the last day of that month.
If it has expired or is damaged, return it to your pharmacist for disposal.
If you are not sure whether you should start taking this medicine, talk to your doctor.
Before you start to take it
Tell your doctor if you have allergies to any other medicines, foods, preservatives or dyes.
Tell your doctor if you have or have had any of the following medical conditions:
- infection (including viral, bacterial and/or fungal infections)
- tuberculosis
- high blood pressure
- diabetes
- osteoporosis
- stomach ulcer
- elevated eyeball pressure (glaucoma) or cataract
- family history of diabetes or glaucoma
- liver problems
- mental health problems such as depression
- scheduled to undergo surgery or are experiencing any other stresses.
Tell your doctor if you have NOT had chicken pox or measles or if you have been in contact with people with chicken pox or measles. These infections may be more serious if you get them while taking CORTIMENT. Your doctor may want to vaccinate you for them before you start on CORTIMENT.
Tell your doctor or pharmacist if you are pregnant or plan to become pregnant or are breast-feeding. Your doctor or pharmacist can discuss with you the risks and benefits involved.
If you have not told your doctor about any of the above, tell him/her before you start taking CORTIMENT.
Taking other medicines
Tell your doctor or pharmacist if you are taking any other medicines, including any that you get without a prescription from your pharmacy, supermarket or health food shop.
CORTIMENT and some medicines may interfere with each other. These include:
- other corticosteroid medicines such as prednisolone, dexamethasone or cortisone
- cholesterol-lowering medicines, antacids or medicines used to treat itch caused by liver problems (e.g. cholestyramine)
- medicines used to treat fungal infections (e.g. ketoconazole or itraconazole)
- some medicines that contain oestrogens, such as oral contraceptives or hormone replacement therapies
- medicines used to treat heart failure (e.g. cardiac glycosides such as digoxin)
- medicines used to treat high blood pressure and fluid build-up (e.g. diuretics)
- medicine used to treat HIV infections (e.g. HIV protease inhibitors)
- medicine used to treat epilepsy (e.g. carbamazepine).
These medicines may be affected by CORTIMENT or may affect how well it works. You may need different amounts of your medicines, or you may need to take different medicines.
Your doctor and pharmacist have more information on medicines to be careful with or avoid while taking this medicine.
How to take CORTIMENT
Follow all directions given to you by your doctor or pharmacist carefully. They may differ from the information contained in this leaflet.
How much to take
Adults:
Take one CORTIMENT 9 mg tablet in the morning with or without food.
How to take it
Swallow the tablet whole with a glass of water. Do not chew, crush or break the tablets.
When to take it
Take your medicine in the morning at about the same time each day. Taking it at the same time each day will have the best effect. It will also help you remember when to take it.
It does not matter if you take this medicine before or after food.
How long to take it
Continue taking your medicine for as long as your doctor tells you, even if you start feeling better.
Usually you will use this medicine daily for a maximum of eight weeks.
If you forget to take it
If it is almost time for your next dose, skip the dose you missed and take your next dose when you are meant to.
Otherwise, take the missed dose as soon as you remember, and then go back to taking your medicine as you would normally.
Do not take a double dose to make up for the dose that you missed.
If you are not sure what to do, ask your doctor or pharmacist.
If you have trouble remembering to take your medicine, ask your pharmacist for some hints.
If you take too much (overdose)
Immediately telephone your doctor or the Poisons Information Centre (telephone 13 11 26) for advice, or go to Accident and Emergency at the nearest hospital, if you think that you or anyone else may have taken too much CORTIMENT. Do this even if there are no signs of discomfort or poisoning. You may need urgent medical attention.
While you are taking CORTIMENT
Things you must do
If you are about to be started on any new medicine, remind your doctor and pharmacist that you are taking CORTIMENT.
Tell any other doctors, dentists, and pharmacists who treat you that you are taking this medicine.
If you are going to have surgery, tell the surgeon or anaesthetist that you are taking this medicine. It may affect other medicines used during surgery.
If you become pregnant while taking this medicine, tell your doctor immediately.
If you are about to have any blood tests, tell your doctor that you are taking this medicine. It may interfere with the results of some tests.
Keep all of your doctor's appointments so that your progress can be checked. Your doctor may do some tests from time to time to make sure the medicine is working and to prevent unwanted side effects.
Things you must not do
Do not eat grapefruit or drink grapefruit juice while you are taking CORTIMENT. Grapefruit juice, but no other fruit juices, can affect budesonide levels in the body. This may increase the chances of getting unwanted side effects.
Do not stop taking CORTIMENT without discussing it with your doctor first.
If you suddenly stop taking your medicine, you may become ill.
Do not use it to treat any other complaints unless your doctor tells you to.
Do not give this medicine to anyone else, even if they have the same condition as you.
Things to be careful of
Be careful driving or operating machinery until you know how CORTIMENT affects you. It is unlikely that CORTIMENT will affect your ability to drive and use machines. Care is required because this type of medicine may sometimes cause dizziness or fatigue.
Side effects
Tell your doctor or pharmacist as soon as possible if you do not feel well while you are taking CORTIMENT.
Like all medicines, this medicine can cause side effects, although not everybody gets them.
Do not be alarmed by the following lists of side effects. You may not experience any of them.
Ask your doctor or pharmacist to answer any questions you may have.
If you have an allergic reaction, contact your doctor immediately. Signs may include hives or swelling of the face, lips, mouth, tongue and throat. This can make it difficult to breathe.
Tell your doctor or pharmacist if you notice any of the following and they worry you:
- reflux or heartburn
- muscle pain, muscle cramps
- stomach pain
- dizziness
- fast or irregular heart beats
- blurred vision
- skin rash or itchiness
- heavy or irregular menstruation in women
- muscle weakness or fatigue, thirst or a tingling sensation
- dry mouth
- Cushing-like symptoms such as round face, acne, weight gain and a tendency to bruise easily
- nausea (feeling sick) or headache
- high temperature, sore throat,runny nose, cough and chills
- reduced response to infection
- change in behaviour such asnervousness, trouble sleeping, mood swings or depression.
The above list includes the more common side effects of your medicine. They are usually mild and short-lived.
Tell your doctor as soon as possible if you notice any of the following:
- sleepiness or drowsiness
- bloating, stomach pain or discomfort
- indigestion
- pain in the your limbs
- swelling in your legs
- tremor.
The above list includes serious side effects that may require medical attention. Serious side effects are rare.
If any of the following happen, tell your doctor immediately or go to Accident and Emergency at your nearest hospital:
- a sudden serious allergic reaction (called anaphylaxis) which can lead to breathing difficulties
- fatigue
- swelling of the hands, ankles or feet.
The above list includes very serious side effects. You may need urgent medical attention or hospitalisation. These side effects are very rare.
Medicines like CORTIMENT tablets (corticosteroids) may affect the normal production of steroid hormones in your body. The effects include:
- increased bone fragility (osteoporosis)
- glaucoma (high eyeball pressure)
- effect on the adrenal gland (small gland near the kidney).
Psychological problems may develop when taking steroids like CORTIMENT. Discuss it with your doctor if you have experienced symptoms of psychological problems while on CORTIMENT. This is particularly important if you are depressed and may be thinking about committing suicide. In very rare cases, psychological problems have developed when high doses of corticosteroids were taken for a long time.
Your doctor may also tell you to take additional oral corticosteroids during periods of stress such as trauma and surgery.
Tell your doctor or pharmacist if you notice anything else that is making you feel unwell. Other side effects not listed above may occur in some patients.
After taking CORTIMENT
Storage
Keep your tablets in the pack until it is time to take them. If you take the tablets out of the pack they may not keep well.
Keep your tablets in a cool dry place where the temperature stays below 30°C.
Do not store CORTIMENT or any other medicine in the bathroom or near a sink. Do not leave it on a window sill or in the car. Heat and dampness can destroy some medicines.
Keep it where children cannot see or reach it. A locked cupboard at least one-and-a-half metres above the ground is a good place to store medicines.
Disposal
If your doctor tells you to stop taking this medicine or the expiry date has passed, ask your pharmacist what to do with any medicine that is left over.
Product description
What it looks like
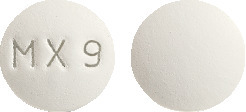
CORTIMENT prolonged-release tablets are white to off-white, round, double convex tablets with a film coating, and 'MX9' engraved on one side of the tablet. The tablets are supplied in blister packs with aluminium press-through foil in a cardboard carton.
CORTIMENT is supplied in packs of 10 and 30 tablets.
Ingredients
CORTIMENT prolonged-release tablets contain 9 mg of budesonide as the active ingredient, and the following inactive ingredients.
Tablet core
- stearic acid [E570]
- lecithin (of Soya origin) [E322]
- microcrystalline cellulose [E460]
- hyprolose [E463]
- lactose monohydrate
- silicon dioxide [E551]
- magnesium stearate [E470b].
Film coating
- methacrylic acid copolymer
- talc - purified [E553b]
- titanium dioxide [E171]
- triethyl citrate.
One tablet contains 50 mg lactose. CORTIMENT prolonged-release tablets contain lecithin (of Soya origin).
Sponsor
CORTIMENT is supplied in Australia by:
Ferring Pharmaceuticals Pty Ltd
Suite 2, Level 1, Building 1
20 Bridge Street
Pymble NSW 2073
Australia
Toll Free: 1800 337 746
www.ferring.com.au
AUST R 225849
CORTIMENT 9 mg budesonide prolonged-release tablets
This leaflet was prepared in August 2019.
#37597v7
CORTIMENT, and FERRING are registered trademarks of Ferring B.V.
Published by MIMS October 2019

 Adverse drug reactions reported for the therapeutic class are presented in Table 2.
Adverse drug reactions reported for the therapeutic class are presented in Table 2. Most of the adverse events mentioned can also be expected for other treatments with glucocorticoids.
Most of the adverse events mentioned can also be expected for other treatments with glucocorticoids. Statistical difference versus placebo was reached for Cortiment 9 mg for both studies and the difference versus placebo was 10.4% and 12.9% respectively.
Statistical difference versus placebo was reached for Cortiment 9 mg for both studies and the difference versus placebo was 10.4% and 12.9% respectively.
