What is in this leaflet
Read this leaflet carefully before taking DAKLINZA. This leaflet answers some common questions about DAKLINZA.
It does not contain all the available information.
It does not take the place of talking to your doctor or pharmacist.
All medicines have risks and benefits. Your doctor has weighed the risks of you taking DAKLINZA against the benefits they expect it will have for you.
If you have any concerns about taking this medicine, ask your doctor or pharmacist.
Keep this leaflet with the medicine. You may need to read it again.
What DAKLINZA is used for
DAKLINZA is a trade name (manufacturer's name) for the medicine, daclatasvir. DAKLINZA is a direct acting antiviral agent (DAA) against the hepatitis C virus (HCV). DAKLINZA is an inhibitor of NS5A, which is a protein that is required to form new HCV particles.
You should not take DAKLINZA alone to treat chronic (lasting a long time) hepatitis C infection in adults. DAKLINZA should only be used together with other antiviral medicines such as sofosbuvir, or asunaprevir (SUNVEPRA), or together with SUNVEPRA, peginterferon alfa, and ribavirin.
How DAKLINZA Works
DAKLINZA (in combination with other medicines) works by stopping the HCV from multiplying and infecting liver cells. After you stop taking DAKLINZA, your doctor will monitor your blood for HCV. If HCV is still not detected in your blood at least 12 weeks after stopping treatment, you have what is called a sustained virologic response (SVR), also referred to as virologic cure.
It is not known if DAKLINZA is safe and effective in children under 18 years of age.
Ask your doctor if you have any questions about why DAKLINZA has been prescribed for you.
DAKLINZA is not addictive. This medicine is available only with a doctor's prescription.
Before you take DAKLINZA
It is important that you check the information below before you take DAKLINZA.
When you must not take DAKLINZA
DAKLINZA is sometimes used with peginterferon alfa and ribavirin. Peginterferon alfa and ribavirin may cause birth defects or death of your unborn baby. If you are pregnant or planning to become pregnant, or your sexual partner is pregnant or plans to become pregnant, do not take these medicines. You or your sexual partner should not become pregnant while taking peginterferon alfa and ribavirin, and for 6 months after treatment ends.
-
Two effective forms of birth control must be used, one by each partner, male and female, during treatment and for the 6 months after treatment with peginterferon alfa and ribavirin.
Talk with your doctor about forms of birth control that may be used during this time. - Females must have a negative pregnancy test before starting treatment with peginterferon alfa and ribavirin, every month while being treated, and every month for 6 months after your treatment ends.
If you or your female sexual partner becomes pregnant while taking, or within 6 months after you stop taking, peginterferon alfa and ribavirin, tell your doctor right away.
Do not take DAKLINZA if you have an allergy to it or to any other ingredients in the formulation listed at the end of this leaflet.
Do not take DAKLINZA if you are currently taking any of these medicines:
- carbamazepine
- dexamethasone (when administered by injection or taken by mouth)
- oxcarbazepine
- phenobarbital
- phenytoin
- rifabutin
- rifampicin
- St. John's wort (Hypericum perforatum) or a product that contains St. John's wort
If you are not sure if any of these medicines are in the products you are taking, talk to your doctor or pharmacist.
Do not use DAKLINZA after the expiry date printed on the back of the pack. If this medicine is taken after the expiry date has passed, it may not work as well.
Do not take DAKLINZA if the packaging is torn or shows signs of tampering.
Before you start to take DAKLINZA
Tell your doctor if you:
- have a current or previous infection with the hepatitis B virus
- have liver problems other than hepatitis C infection
- have had, or are intending to have, a liver transplant
- have diabetes
- have any other medical condition
DAKLINZA should not be used during pregnancy.
Tell your doctor if you are pregnant or intend to become pregnant. It is not known if DAKLINZA will harm your unborn baby.
If you can become pregnant, continue the use of effective contraception for 5 weeks after the end of your treatment with DAKLINZA.
If you are also taking ribavirin, you must follow the contraception instructions under "When you must not take DAKLINZA" above.
Tell your doctor or pharmacist if you are breast-feeding or plan to breast-feed. It is recommended that you do not breast-feed while taking DAKLINZA. It is not known if DAKLINZA passes into breast milk.
If you have not told your doctor about any of the above, tell them before you use DAKLINZA.
As DAKLINZA should only be used together with other antiviral medicines such as sofosbuvir, or SUNVEPRA, or together with SUNVEPRA, peginterferon alfa, and ribavirin, please read the Consumer Medicine Information for the other products prescribed by your doctor before starting DAKLINZA.
Taking other medicines
Be sure to inform your doctor of all medications you are taking including prescribed drugs, over the counter products, natural therapies, vitamin supplements and recreational drugs.
DAKLINZA and other medicines may affect each other. This can cause you to have too much or not enough DAKLINZA or other medicines in your body, which may affect the way DAKLINZA or your other medicines work, or may cause side effects.
Medicines for other conditions:
Tell your doctor if you are taking or starting to take medicines that contain:
- amiodarone
- atazanavir. You may need a lower dose of DAKLINZA (30 mg).
- boceprevir or telaprevir. You may need a lower dose of DAKLINZA (30 mg).
- clarithromycin, erythromycin. You may need a lower dose of DAKLINZA (30 mg).
- dabigatran
- digoxin
- diltiazem, verapamil
- efavirenz, etravirine, or nevirapine. You may need a higher dose of DAKLINZA (90 mg).
- elvitegravir, cobicistat, emtricitabine, or tenofovir disoproxil fumarate. You may need a lower dose of DAKLINZA (30 mg).
- fluconazole, ketoconazole, itraconazole, posaconazole, or voriconazole. You may need a lower dose of DAKLINZA (30 mg).
- rosuvastatin, atorvastatin, fluvastatin, simvastatin, pitavastatin, or pravastatin
- warfarin and other similar medicines called vitamin K antagonists used to thin the blood
Your doctor will be able to advise you about the most appropriate medications to treat your condition. It is important that you tell your doctor or pharmacist about the medicines you are taking, even if they are not listed in this leaflet.
They will be able to provide you with more information than is contained within this leaflet on the medicines you need to be careful with, or should avoid while taking DAKLINZA.
How to take DAKLINZA
DAKLINZA should be given only when prescribed by your doctor. Follow all directions given to you by your doctor or pharmacist carefully. They may differ from the information contained in this leaflet.
How much to take
Take DAKLINZA exactly as your doctor tells you to take it. Do not change your dose unless your doctor tells you to.
Do not stop taking DAKLINZA without first talking with your doctor. If you think there is a reason to stop taking DAKLINZA, talk with your doctor before doing so.
How to take it
Swallow the tablet whole with a drink such as a glass of water.
When to take DAKLINZA
Take DAKLINZA once each day with or without food.
How long to take it
Continue taking DAKLINZA for as long as your doctor tells you to.
Do not stop taking DAKLINZA unless your doctor tells you to - even if you feel better.
If you forget to take it
If you miss a dose of DAKLINZA and less than 20 hours have passed since you were to take the missed dose, take the missed dose as soon as possible. Take the next dose at your regular time.
If you miss a dose of DAKLINZA and more than 20 hours have passed since you were to take the missed dose, skip the missed dose. Take the next dose at your regular time.
Do not take 2 doses of DAKLINZA at the same time to make up for the missed dose.
If you take too much (overdose)
Immediately call your doctor or the Poisons Information Centre on 131126 in Australia, or go to the Accident and Emergency Centre at your nearest hospital if you or anyone else takes too much DAKLINZA. Do this even if there are no signs of discomfort or poisoning.
While you are using DAKLINZA
Things you must do
- If you become pregnant while taking DAKLINZA, tell your doctor immediately.
- If you are about to start taking any new medicines, tell your doctor and pharmacist that you are taking DAKLINZA. DAKLINZA and the other medicine may interfere with each other.
- If you are taking DAKLINZA together with SUNVEPRA, your doctor may perform additional tests that will determine how well your liver is working. Please read the Consumer Medicine Information for SUNVEPRA.
Things you must not do
- Do not give DAKLINZA to anyone else, even if they have the same condition as you.
- Do not use DAKLINZA to treat any other complaints unless your doctor tells you to.
- Do not stop taking DAKLINZA without checking with your doctor.
Things to be careful of
Be careful driving or operating machinery until you know how DAKLINZA affects you.
Make sure that you visit your doctor regularly throughout your entire course of treatment with DAKLINZA.
Side effects
Tell your doctor or pharmacist as soon as possible if you do not feel well while you are taking DAKLINZA. All medicines can have side effects. Sometimes they are serious, most of the time they are not. You may need medical treatment if you get some of the side effects
Ask your doctor or pharmacist to answer any questions you may have.
The most common side effects when DAKLINZA is taken in combination with SUNVEPRA include:
- headache
- tiredness
- diarrhoea
- nasal congestion (blocked nose)
- nausea
The most common side effects when DAKLINZA is taken in combination with sofosbuvir (some patients in studies of this regimen also received ribavirin) include:
- tiredness
- headache
- nausea
- joint pain
- diarrhoea
The most common side effects when DAKLINZA is taken in combination with SUNVEPRA, peginterferon alfa, and ribavirin include:
- tiredness
- headache
- itching
- unusual weakness
- flu-like symptoms
- insomnia
- rash
- anaemia
- cough
- dry skin
- diarrhoea
- nausea
- hair loss
- irritability
- fever
- muscle aches
If any of the following happen, tell your doctor immediately, or go to the Accident and Emergency Centre at your nearest hospital:
- allergic reaction - swelling of the face, lips, or throat which makes breathing difficult
If you have these side effects, you may have had a serious reaction to DAKLINZA. You may need urgent medical attention or hospitalisation.
This is not a complete list of side effects, other side effects not listed above may also occur in some patients.
Tell your doctor if you notice anything that is making you feel unwell.
Do not be alarmed by this list of possible side effects. You may not experience any of them or only some of them.
After using DAKLINZA
Storage
Store DAKLINZA tablets in a cool dry place where the temperature stays below 30°C.
Keep your tablets in the original container until it is time to take them.
Do not store DAKLINZA or any other medicine in the bathroom or near the kitchen sink. Do not leave it in the car. Heat and dampness can destroy some medicines.
Keep DAKLINZA tablets where children cannot reach them. A locked cupboard at least one-and-a-half metres above the ground is a good place to store medicines.
Disposal
If your doctor tells you to stop taking DAKLINZA tablets, or the tablets have passed their expiry date, ask your pharmacist what to do with any that are left over.
Product description
What it looks like
DAKLINZA tablets come in three strengths:
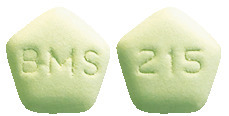
- DAKLINZA 60 mg tablets are light green biconvex pentagonal debossed with "BMS" on one side and "215" on the other side. Available in packs of 7 and 28 tablets.
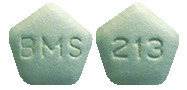
- DAKLINZA 30 mg tablets are green biconvex pentagonal debossed with "BMS" on one side and "213" on the other side. Available in packs of 7 and 28 tablets.
Ingredients
Each capsule contains:
Active ingredients:
- DAKLINZA 60 mg tablets - 60 mg of daclatasvir as daclatasvir dihydrochloride per tablet
- DAKLINZA 30 mg tablets - 30 mg of daclatasvir as daclatasvir dihydrochloride per tablet
Other ingredients:
lactose, microcrystalline cellulose, croscarmellose sodium, silicon dioxide, magnesium stearate, and OPADRY Green.
Opadry Green contains hypromellose, titanium dioxide, Macrogol 400, indigo carmine aluminum lake, and iron oxide yellow.
DAKLINZA tablets do not contain gluten or sucrose.
Registration Numbers
DAKLINZA 60 mg - AUST R 222742
DAKLINZA 30 mg - AUST R 222743
Sponsored by
Bristol-Myers Squibb Australia Pty Ltd,
4 Nexus Court, Mulgrave,
Victoria 3170, Australia
This information in no way replaces the advice of your doctor or pharmacist.
Date of Preparation: March 2020
V7.0 27 March 2020
Published by MIMS May 2020


 In a pooled analysis of 629 patients who received daclatasvir/ sofosbuvir with or without ribavirin in phase 2 and 3 studies, 44 patients (19 with genotype 1a, 2 with genotype 1b, 2 with genotype 2, and 21 with genotype 3) qualified for resistance analysis due to virologic failure or early study discontinuation and having HCV RNA greater than 1,000 IU/mL. Postbaseline NS5A and NS5B sequencing (assay cut-off of 20%) were available for 44/44 and 39/44 patients, respectively.
In a pooled analysis of 629 patients who received daclatasvir/ sofosbuvir with or without ribavirin in phase 2 and 3 studies, 44 patients (19 with genotype 1a, 2 with genotype 1b, 2 with genotype 2, and 21 with genotype 3) qualified for resistance analysis due to virologic failure or early study discontinuation and having HCV RNA greater than 1,000 IU/mL. Postbaseline NS5A and NS5B sequencing (assay cut-off of 20%) were available for 44/44 and 39/44 patients, respectively.





 Among subjects who had failed prior therapy, SVR rate was the same (82%) among the 84 subjects with prior partial response and the 119 subjects with prior null response. Response was rapid (95% of subjects had HCV RNA < LLOQ at week 4). There were no differences in antiviral response due to race, gender, IL28B allele, presence or absence of cirrhosis, or age in any of the treatment populations. SVR rates were consistently high across all categories of baseline viral load. Among subjects 65 and older, 88% (117/133) achieved SVR and among subjects 75 years or older, 100% (10/10) achieved SVR.
Among subjects who had failed prior therapy, SVR rate was the same (82%) among the 84 subjects with prior partial response and the 119 subjects with prior null response. Response was rapid (95% of subjects had HCV RNA < LLOQ at week 4). There were no differences in antiviral response due to race, gender, IL28B allele, presence or absence of cirrhosis, or age in any of the treatment populations. SVR rates were consistently high across all categories of baseline viral load. Among subjects 65 and older, 88% (117/133) achieved SVR and among subjects 75 years or older, 100% (10/10) achieved SVR. In the nonresponder cohort, 78% of prior partial responders and 81% of prior null responders achieved SVR. In the intolerant/ ineligible cohort, 94% of subjects who were intolerant and 86% of those who were ineligible achieved SVR. Response was rapid (96% of subjects had HCV RNA < LLOQ at week 4). Within the prior nonresponder and interferon intolerant/ ineligible populations, there were no differences in antiviral response due to gender, baseline HCV RNA level, IL28B allele, presence or absence of cirrhosis or age. Among subjects 65 years and older, 91% (81/89) achieved SVR and among subjects 75 years or older, 100% (4/4) achieved SVR.
In the nonresponder cohort, 78% of prior partial responders and 81% of prior null responders achieved SVR. In the intolerant/ ineligible cohort, 94% of subjects who were intolerant and 86% of those who were ineligible achieved SVR. Response was rapid (96% of subjects had HCV RNA < LLOQ at week 4). Within the prior nonresponder and interferon intolerant/ ineligible populations, there were no differences in antiviral response due to gender, baseline HCV RNA level, IL28B allele, presence or absence of cirrhosis or age. Among subjects 65 years and older, 91% (81/89) achieved SVR and among subjects 75 years or older, 100% (4/4) achieved SVR. Response was rapid (98% of subjects had HCV RNA < LLOQ at week 4). There were no differences in antiviral response due to gender, age, baseline HCV RNA level, presence or absence of baseline polymorphisms, IL28B allele status, or presence or absence of cirrhosis in any of the treatment populations.
Response was rapid (98% of subjects had HCV RNA < LLOQ at week 4). There were no differences in antiviral response due to gender, age, baseline HCV RNA level, presence or absence of baseline polymorphisms, IL28B allele status, or presence or absence of cirrhosis in any of the treatment populations.



