What is in this leaflet
This leaflet answers some common questions about Effient.
It does not contain all the available information.
It does not take the place of talking to your doctor or pharmacist.
The information in this leaflet was last updated on the date shown on the final page. More recent information on this medicine may be available. Make sure you speak to your pharmacist, nurse or doctor to obtain the most up to date information on this medicine. You can also download the most up to date leaflet from www.lilly.com.au. The updated leaflet may contain important information about this medicine and its use that you should be aware of.
All medicines have risks and benefits. Your doctor or pharmacist has weighed the risks of you taking this medicine against the benefits they expect it will have for you.
Always follow the instructions that your doctor or pharmacist give you about Effient.
If you have any concerns about taking this medicine, ask your doctor or pharmacist.
Keep this leaflet with the medicine.
You may need to read it again.
What Effient is used for
Effient is used to prevent blood cells from clotting.
It contains the active ingredient, prasugrel.
It is used by people who have had a PCI (percutaneous coronary intervention) because of unstable angina or a heart attack.
PCI is a procedure where a balloon-tipped tube is used to open a blocked artery, with or without a stent being placed in the artery.
Effient belongs to the group of medicines called antiplatelet agents.
It works by reducing the ability of blood cells to clot. By preventing blood cells from clumping, it reduces the chances of blood clots forming (a process called thrombosis), thereby decreasing or even stopping blood supply to the heart muscle.
Effient is always taken with aspirin.
Ask your doctor if you have any questions about why this medicine has been prescribed for you.
Your doctor may have prescribed this medicine for another use. If you want more information, ask your doctor.
This medicine is available only with a doctor's prescription.
Before you take Effient
When you must not take it
Do not take Effient if you have an allergy to Effient or any of the ingredients listed at the end of this leaflet:
Symptoms of an allergic reaction may include:
- shortness of breath
- wheezing or difficulty breathing
- swelling of the face, lips, tongue or other parts of the body
- rash
- itching.
If you are not sure if you have an allergy to Effient, check with your doctor.
Do not take Effient if you have had any of the following medical conditions:
- bleeding caused by a stomach ulcer
- bleeding inside your head
- stroke
- transient ischaemic attack (TIA) which resulted in a temporary paralysis, numbness, speech difficulty or other symptoms affecting your nervous system which happened suddenly and disappeared within 24 hours
- severe liver disease
Do not take Effient if:
- the packaging is torn or shows signs of tampering (or the tablets do not look quite right)
- the expiry date on the pack has passed.
If you take this medicine after the expiry date has passed, it may not work as well.
Do not give this medicine to children.
There is no experience with the use of this medicine in children.
Before you start to take it
Tell your doctor if:
- you have any allergies to any other medicines including those you have previously taken to prevent your blood from clotting, or any other substances such as foods, preservatives or dyes
- you are already taking aspirin
- you are pregnant or plan to become pregnant
Your doctor will discuss the possible risks and benefits of taking this medicine during pregnancy. - you are breast-feeding or plan to breast-feed
Effient is not recommended while you are breast-feeding. It is not known whether it passes into breast-milk. - you have or have had any of the following medical conditions:
- bleeding disorders or blood clotting problems
- a tendency to bleed as a result of a recent trauma, recent surgery (including dental surgery), recent or recurrent gastrointestinal bleeding, active peptic ulcer disease
- a history of kidney or liver problems
- a history of stroke or TIA
- weigh less than 60 kg
- are more than 75 years old
- a history of tumours or cancer - you are planning to have surgery (including dental procedures).
If you have not told your doctor or pharmacist about any of the above, tell them before you start taking Effient.
Taking other medicines
Tell your doctor or pharmacist if you are taking any other medicines, including medicines you buy without a prescription from a pharmacy, supermarket or health food shop.
You will be prescribed aspirin at a low dose with Effient. Aspirin works together with Effient.
Some medicines and Effient may interfere with each other. These are:
- medicines that "thin the blood" such as warfarin and heparin.
There are others so please check with your doctor or pharmacist
- non steroidal anti-inflammatory drugs (NSAIDs) - medicines used to treat arthritis, period pain, aches and pain
- fibrinolytics - a group of medicines used to dissolve a blood clot that has formed in an artery or a vein
- some medicines used to treat HIV (e.g. efavirenz).
- some medicines used to treat cancer (e.g. cyclophosphamide).
These medicines may be affected by Effient or may affect how well it works. You may need different amounts of your medicine or you may need to take different medicines.
Your doctor or pharmacist can tell you what to do if you are taking any of these medicines. They also have a more complete list of medicines to be careful with or avoid while taking Effient.
Ask your doctor or pharmacist if you are not sure if you are taking any of these medicines.
How to take Effient
Take this medicine only as prescribed by your doctor and follow his/her directions carefully.
These may differ from the information contained in this leaflet.
How much to take
Your doctor will tell you how many tablets to take each day.
Effient is available as a 5 and 10 mg tablet. It is usual for your doctor to start you on a single dose of six 10 mg tablets and then continue with a 10 mg or 5 mg once daily dose. Your doctor will also prescribe a daily dose of aspirin to take with this medicine.
When to take it
You should swallow the tablets with a glass of water.
The tablets can be taken before or after meals.
Do not break the tablet in half. Talk to your doctor or pharmacist if you have trouble swallowing tablets.
Take it at the same time each day.
Taking your tablets at the same time will have the best effect. It will also help you to remember when to take it.
How long to take it
Continue taking Effient for as long as your doctor recommends.
If you forget to take it
If it is almost time for your next dose, skip the dose you missed and take your next dose when you are meant to. Otherwise, take it as soon as you remember, then go back to taking your tablets as you would normally.
Do not take a double dose to make up for the dose you have missed.
This may increase the chance of you getting an unwanted side effect.
If you are not sure what to do, ask your doctor or pharmacist.
If you have trouble remembering to take your medicine, ask your pharmacist for some hints.
If you take too much (overdose)
Immediately telephone your doctor, or Poisons Information Centre (telephone in Australia: 13 11 26; in New Zealand: 0800 POISON or 0800 764 766) for advice if you think that you or anyone else may have taken too much Effient. Do this even if there are no signs of discomfort or poisoning.
You may need urgent attention.
While you are taking Effient
Things you must do
Take it every day exactly as your doctor has prescribed.
If you become pregnant while you are taking it, tell your doctor.
If you decide to breast-feed your baby, tell your doctor.
Your doctor may want to discuss this and change your medicine.
If you are about to start taking any new medicines, tell your doctor and pharmacist that you are taking Effient.
Tell all doctors, dentists and pharmacists who are treating you that you are taking Effient.
Tell your doctor, dentist or pharmacist that you are taking Effient before you have any surgery.
It may increase the risk of bleeding during an operation or some dental work. Therefore, treatment may need to be stopped before surgery.
Your doctor will decide whether to stop Effient and if so, for how long.
Ask your doctor whether there are any activities you should avoid while taking this medicine, for example, certain sports.
Sometimes after an injury, bleeding may occur inside your body without you knowing about it.
Tell your doctor immediately if you are injured while taking this medicine.
It may take longer than usual to stop bleeding while you are taking Effient.
Tell your doctor immediately if you notice the return of any of the symptoms you had before starting Effient.
Things you must not do
Do not give this medicine to anyone else, even if they have the same condition as you.
Do not stop taking this medicine without informing your doctor as it may increase the chance of a heart attack or stroke or a blood clot forming.
Things to be careful of
Be careful driving or operating machinery until you know how it affects you.
Make sure you know how you react to it before you drive a car, operate machinery or do anything else that could be dangerous if you are dizzy or light-headed. If this does occur, do not drive.
If you drink alcohol, faintness or dizziness may be worse.
Side effects
Tell your doctor or pharmacist as soon as possible if you do not feel well while you are taking Effient.
It helps most people, but it may have unwanted side effects in a few people. All medicines can have side effects. Sometimes they are serious, most of the time they are not. You may need medical treatment if you get some of the side effects.
Ask your doctor or pharmacist to answer any questions you may have.
Tell your doctor if you notice any of the following:
- rash
- nose bleeds
- cuts that take longer than usual to stop bleeding
- bleeding gums.
Tell your doctor immediately, or go to Accident and Emergency if you notice any of the following:
- signs of anaemia (being tired and looking pale)
- severe or uncontrollable bleeding, including after surgery
- coughing up blood (a sign of bleeding from the stomach)
- pink or brown urine
- red or black stools
- diarrhoea with blood, mucus, stomach pain and fever (a sign of bleeding from the intestine)
- unusual bruising (bruises that develop without known cause or grow in size)
- red or purple spots visible through your skin
- unusually heavy bleeding or bruising from cuts or wounds
- blood in the eyes
- swelling of the face, lips, mouth, tongue or throat which may cause difficulty in swallowing or breathing .
The above list includes serious side effects. You may need urgent medical attention.
Tell your doctor if you notice any other effects.
Other side effects not listed above may also occur in some people.
Do not be alarmed by this list of possible side effects.
You may not experience any of them.
After using Effient
Storage
Keep your tablets in the blister pack until it is time to take them.
If you take the tablets out of the blister pack, they may not keep well.
Keep them in a cool, dry place where it stays below 30°C. Do not store them, or any other medicine, in a bathroom or near a sink. Do not leave them in the car or on window sills.
Heat and dampness can destroy some medicines.
Keep them where children cannot reach them.
A locked cupboard at least one and a half metres above the ground is a good place to store medicines.
Disposal
If your doctor tells you to stop taking this medicine, or the tablets have passed their expiry date, ask your pharmacist what to do with any tablets left over.
Product description
What it looks like
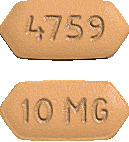
- The 5 mg tablets are yellow, double-arrow shaped, film-coated, unscored, debossed with "5 MG" on one side and "4760" on the other side.
- The 10 mg tablets are beige, double-arrow shaped, film-coated, unscored, debossed with "10 MG" on one side and with "4759" on the other side.
A box contains 6 or 28 tablets.
Ingredients
Effient contains either 5 mg or 10 mg of prasugrel (as hydrochloride) as the active ingredient.
It also contains:
- Mannitol
- Hypromellose
- Croscarmellose sodium
- Cellulose - microcrystalline
- Magnesium stearate
- Lactose
- Titanium dioxide
- Glycerol acetate
- Iron oxide yellow CI77492
- Iron oxide red CI77491.
Supplier
Supplied in Australia by:
Eli Lilly Australia Pty Limited
112 Wharf Road
WEST RYDE NSW 2114
Supplied in New Zealand by:
Eli Lilly and Company (NZ) Limited
Level 1
123 Ormiston Road
Botany South
Auckland 2016
NEW ZEALAND
AUST R Numbers
- Effient 5 mg - AUST R 150809
- Effient 10 mg - AUST R 150810
®= Registered Trademark
This leaflet was prepared in May 2013



 The mean maximum IPA after a 60 mg LD of prasugrel was 79% and 83%, respectively for 20 microM and 5 microM ADP, with at least 89% of all healthy subjects and patients with stable atherosclerosis achieving at least 50% IPA by 1 hour for both ADP concentrations. Prasugrel mediated IPA exhibits low between subject (9%) and within subject (12%) variability with both 5 microM and 20 microM ADP.
The mean maximum IPA after a 60 mg LD of prasugrel was 79% and 83%, respectively for 20 microM and 5 microM ADP, with at least 89% of all healthy subjects and patients with stable atherosclerosis achieving at least 50% IPA by 1 hour for both ADP concentrations. Prasugrel mediated IPA exhibits low between subject (9%) and within subject (12%) variability with both 5 microM and 20 microM ADP. The Kaplan Meier curve shows the primary composite endpoint of CV death, nonfatal MI, or nonfatal stroke over time in the all ACS population (see Figure 2). The all ACS event curves separated as early as 3 days and continued to diverge over the 15 month follow-up period. Prasugrel demonstrated a relative risk reduction of 18% and an absolute risk reduction of 0.9% in the primary composite endpoint from 0 to 3 days (4.7% in the prasugrel group and 5.6% in the clopidogrel group; HR 0.825; 95% CI, 0.711, 0.957; p = 0.011). Prasugrel demonstrated a relative risk reduction of 20% and an absolute risk reduction of 1.2% in the primary composite endpoint from 3 days to the end of the study (5.2% in the prasugrel group and 6.4% in the clopidogrel group; HR 0.805; 95% CI, 0.698, 0.927; p = 0.003). Primary individual outcome events showed an absolute risk reduction of 2.1% and relative risk reduction of 24.3% in nonfatal MI with prasugrel compared to clopidogrel. A 0.2% absolute risk reduction and 11.4% relative risk reduction in CV death was seen in the prasugrel group compared to clopidogrel while for nonfatal stroke, there was no difference between the prasugrel and clopidogrel treated groups (see Table 1).
The Kaplan Meier curve shows the primary composite endpoint of CV death, nonfatal MI, or nonfatal stroke over time in the all ACS population (see Figure 2). The all ACS event curves separated as early as 3 days and continued to diverge over the 15 month follow-up period. Prasugrel demonstrated a relative risk reduction of 18% and an absolute risk reduction of 0.9% in the primary composite endpoint from 0 to 3 days (4.7% in the prasugrel group and 5.6% in the clopidogrel group; HR 0.825; 95% CI, 0.711, 0.957; p = 0.011). Prasugrel demonstrated a relative risk reduction of 20% and an absolute risk reduction of 1.2% in the primary composite endpoint from 3 days to the end of the study (5.2% in the prasugrel group and 6.4% in the clopidogrel group; HR 0.805; 95% CI, 0.698, 0.927; p = 0.003). Primary individual outcome events showed an absolute risk reduction of 2.1% and relative risk reduction of 24.3% in nonfatal MI with prasugrel compared to clopidogrel. A 0.2% absolute risk reduction and 11.4% relative risk reduction in CV death was seen in the prasugrel group compared to clopidogrel while for nonfatal stroke, there was no difference between the prasugrel and clopidogrel treated groups (see Table 1). For patients who survived an on study stroke or myocardial infarction, prasugrel treated patients demonstrated a relative risk reduction of 33% and an absolute risk reduction of 4.1% in the incidence of subsequent primary endpoint events compared to clopidogrel treated patients (7.8% for prasugrel and 11.9% for clopidogrel, HR 0.67; 95% CI, 0.45, 0.98, p = 0.037).
For patients who survived an on study stroke or myocardial infarction, prasugrel treated patients demonstrated a relative risk reduction of 33% and an absolute risk reduction of 4.1% in the incidence of subsequent primary endpoint events compared to clopidogrel treated patients (7.8% for prasugrel and 11.9% for clopidogrel, HR 0.67; 95% CI, 0.45, 0.98, p = 0.037). Analyses were performed to assess the effect of demographics, baseline characteristics, and medical history on the incidence of the primary endpoint of CV death, nonfatal MI, or nonfatal stroke by patients randomised to prasugrel or clopidogrel. The treatment benefit associated with prasugrel was preserved across the major prespecified subgroups in all 3 populations (UA/NSTEMI, STEMI and all ACS) as shown in Figure 3.
Analyses were performed to assess the effect of demographics, baseline characteristics, and medical history on the incidence of the primary endpoint of CV death, nonfatal MI, or nonfatal stroke by patients randomised to prasugrel or clopidogrel. The treatment benefit associated with prasugrel was preserved across the major prespecified subgroups in all 3 populations (UA/NSTEMI, STEMI and all ACS) as shown in Figure 3.
 The secondary endpoint data for the UA/NSTEMI and STEMI populations are similar to those for the all ACS population.
The secondary endpoint data for the UA/NSTEMI and STEMI populations are similar to those for the all ACS population.

 Table 5 shows the incidence of non-CABG related bleeding by UA/NSTEMI and STEMI subgroups.
Table 5 shows the incidence of non-CABG related bleeding by UA/NSTEMI and STEMI subgroups.

 Patients ≥ 75 years of age also had a higher risk of stroke compared to those < 75 years. The incidence of stroke in patients ≥ 75 years of age treated with prasugrel was 2.89% compared to 1.43% with clopidogrel while for patients < 75 years the rate of stroke was 0.83% with prasugrel and 0.99% with clopidogrel (see Clinical Trials).
Patients ≥ 75 years of age also had a higher risk of stroke compared to those < 75 years. The incidence of stroke in patients ≥ 75 years of age treated with prasugrel was 2.89% compared to 1.43% with clopidogrel while for patients < 75 years the rate of stroke was 0.83% with prasugrel and 0.99% with clopidogrel (see Clinical Trials). In TRITON, in patients with or without a history of TIA or stroke, the incidence of stroke is shown in Table 9.
In TRITON, in patients with or without a history of TIA or stroke, the incidence of stroke is shown in Table 9.


