What is in this leaflet
Read this leaflet carefully before taking your medicine.
This leaflet answers some common questions about pravastatin. It does not contain all the available information. It does not take the place of talking to your doctor or pharmacist.
Ask your doctor or pharmacist:
- if there is anything you do not understand in this leaflet,
- if you are worried about taking your medicine, or
- to obtain the most up-to-date information
All medicines have risks and benefits. Your doctor has weighed the risks of you using this medicine against the benefits they expect it will have for you.
Keep this leaflet with your medicine. You may want to read it again.
What PRAVASTATIN AN is used for
The name of your medicine is PRAVASTATIN AN. It contains the active ingredient, pravastatin sodium.
It is used, together with changes in the diet, to treat:
- people who have high blood cholesterol levels
- people who have had a heart attack (even if their blood cholesterol levels are normal)
- people who have had an episode of unstable angina
In these people pravastatin can reduce the risk of having a stroke, reduce the risk of further heart disease, or reduce the possibility of needing a bypass operation.
It is also used to treat children and adolescent patients aged 8 years and older who have heterozygous familial hypercholesterolaemia (an inherited disorder which produces high blood cholesterol levels). This is in combination with diet and lifestyle changes.
Ask your doctor if you have any questions about why this medicine has been prescribed for you. Your doctor may have prescribed this medicine for another reason.
This medicine is available only with a doctor's prescription.
How it works
Pravastatin lowers high blood cholesterol levels (doctors call this hypercholesterolaemia. It is more effective if it is taken with a cholesterol lowering diet.
If you have had a heart attack, an episode of unstable angina or you have too much cholesterol in your blood, then you have an increased risk of a blood clot forming in your blood vessels and causing a blockage. Blood vessels that become blocked in this way can lead to further heart disease, angina or stroke.
Pravastatin is used on a long term basis, where you take it every day.
There is no evidence that this medicine is addictive.
Use in children
Pravastatin can be in used in children and adolescents aged 8 years and over, if they need treatment for heterozygous familial hypercholesterolaemia (a genetic disorder causing high cholesterol levels).
There is not enough information to recommend the use of this medicine in children less than 8 years of age.
Before you take PRAVASTATIN AN
When you must not take it
Do not take this medicine if:
- you are pregnant or there is a chance that you could become pregnant (i.e. not using adequate contraception).
Pravastatin may affect your developing baby if you take it during pregnancy. - you are breast-feeding.
Pravastatin can pass into human breast milk and may affect a baby being breast-fed. - you have liver disease or unexplained high levels of liver enzymes called serum transaminases
- it has passed the expiry date (EXP) printed on the pack.
- the packaging is torn, shows signs of tampering or it does not look quite right.
- you have had an allergic reaction to pravastatin or any of the ingredients listed at the end of this leaflet.
Symptoms of an allergic reaction may include cough, shortness of breath, wheezing or difficulty breathing; swelling of the face, lips, tongue, throat or other parts of the body, rash itching or hives on the skin, fainting or hayfever-like symptoms.
If you think you are having an allergic reaction, contact your doctor immediately or go to the Accident and Emergency department at the nearest hospital.
Before you start to take it
Before you start taking this medicine, tell your doctor if:
- You have allergies to:
- any other medicines
- any other substances, such as foods, preservatives or dyes.
- You have or have had any medical conditions, especially the following:
- liver problems
- kidney problems
- thyroid problems or any type of hormonal disorder
- central nervous system vascular lesions, especially if this happened after taking a different type of cholesterol lowering drug (a doctor will have told you this)
- allergies
- homozygous familial hypercholesterolaemia (a doctor will have told you this)
- increased triglycerides in your blood (a doctor will have told you this)
- muscle problems (including pain, tenderness or weakness), especially if this happened after taking a different cholesterol lowering drug.
- You are currently pregnant or breast-feeding or plan to become pregnant or breastfeed. You should also check with your doctor about your contraceptive use, to ensure you don't become pregnant accidentally.
- You drink alcohol every day; or if you have, or have had, any problems with drug or alcohol dependence.
- You have had an organ (e.g. kidney or heart) transplant.
- You have recently been vaccinated or plan to get a vaccination.
- You are planning to have surgery.
- You are currently receiving or are planning to receive dental treatment.
- You are taking or are planning to take any other medicines.
This includes vitamins and supplements that are available from your pharmacy, supermarket or health food shop.
Some medicines may interact with pravastatin. These include:
- other medicines used to lower cholesterol, for example, gemfibrozil, nicotinic acid (niacin), cholestyramine and colestipol
- cyclosporin, used to suppress the immune system
- ketoconazole, used to treat certain fungal infections
- spironolactone, a diuretic, used to reduce water in the body
- cimetidine, used to treat ulcers or acid indigestion
- erythromycin, used to treat bacterial infections
- antacids.
If you are taking any of these you may need a different dose or you may need to take different medicines.
Other medicines not listed above may also interact with pravastatin.
How to take PRAVASTATIN AN
Follow carefully all directions given to you by your doctor or pharmacist. Their instructions may be different to the information in this leaflet.
How much to take
Your doctor or pharmacist will tell you how much of this medicine you should take. This will depend on your condition and whether you are taking any other medicines.
The dose for lowering cholesterol in adults is 10-80 mg daily.
To reduce the possibility of a stroke or heart attack in all patients with high blood cholesterol or who have had a heart attack and have normal blood cholesterol, the dose is 40 mg daily.
If you are over 65 and/or have liver or kidney disease or you are taking cyclosporin, you may be prescribed a lower dose.
In children with heterozygous familial hypercholesterolaemia, the recommended dose is 20 mg once daily for children 8-13 years of age and 40 mg once daily in adolescents 14-18 years of age.
Do not stop taking your medicine or change your dosage without first checking with your doctor.
How to take it
Swallow the tablets whole with a glass of water.
When to take it
Take your medicine once a day, in the evening before bed-time.
For best results, take your medicine on an empty stomach, usually two or more hours after your last meal.
Take your medicine at about the same time each day. Taking it at the same time each day will have the best effect and will also help you remember when to take it.
How long to take it for
Continue taking your medicine for as long as your doctor tells you.
Make sure you have enough to last over weekends and holidays.
If you forget to take it
If it is almost time to take your next dose, skip the missed dose and take your next dose at the usual time. Otherwise take it as soon as you remember and then go back to taking your medicine as you would normally.
Do not take a double dose to make up for missed doses.
This may increase the chance of unwanted side effects.
If you have trouble remembering to take your medicine, ask your pharmacist for some hints.
If you take too much (overdose)
If you think that you or anyone else may have taken too much of this medicine, immediately telephone your doctor or the Poisons Information Centre (Tel: 13 11 26 for Australia) for advice. Alternatively go to the Accident and Emergency Department at your nearest hospital.
Do this even if there are no signs of discomfort or poisoning. You may need urgent medical attention.
While you are using PRAVASTATIN AN
Things you must do
Tell your doctor immediately if you experience any unexplained muscle pain, tenderness or weakness.
Stop taking your medicine and tell your doctor or go to a hospital immediately if you have dark or brown urine, together with the symptoms above.
Tell your doctor immediately if you have a dry cough, problems breathing, have a temperature, lose weight and/or generally feel tired.
These may be signs of a potentially fatal condition called interstitial lung disease.
Tell your doctor that you are taking this medicine if:
- you are about to be started on any new medicine
- you plan to have any vaccinations or immunisations
- you become pregnant or plan to breastfeed (stop taking it and tell your doctor immediately)
- you are about to have any blood tests
- you are going to have surgery.
Your doctor may occasionally do tests to make sure the medicine is working and to prevent side effects. Go to your doctor regularly for a check-up.
Tell any other doctors, dentists, and pharmacists who are treating you that you are taking this medicine.
Things you must not do
Do not:
- give this medicine to anyone else, even if their symptoms seem similar to yours
- take your medicine to treat any other complaints unless your doctor or pharmacist tells you to
- stop taking your medicine, or change the dosage, without checking with your doctor.
Things to be careful of
Be careful while driving or operating machinery until you know how this medicine affects you.
Pravastatin generally does not interfere with your ability to drive or operate machinery. However, as with many other medicines, this medicine may cause dizziness in some people. Make sure you know how you react to this medicine before you drive a car or operate machinery.
Avoid drinking large quantities of alcohol. Drinking large amounts of alcohol may increase the chance of this medicine causing liver problems.
Changes to lifestyle that may help reduce the chance of coronary heart disease
Lowering high cholesterol can help reduce your chances of having coronary heart disease (CHD). However, your chances of having CHD may be increased by several other factors including high blood pressure, cigarette smoking, diabetes, excess weight, family history of CHD, being a male and being a woman who has reached menopause.
Some self-help measures suggested below may help your condition and help reduce your chances of having CHD. Talk to your doctor, pharmacist, or dietician about these measures and for more information:
- Diet - continue the low fat diet recommended by your doctor, dietician, or pharmacist.
- Weight - your doctor may advise you to lose weight if you are overweight.
- Exercise - make exercise a part of your routine - walking is good.
Ask your doctor for advice before starting exercise. - Smoking - your doctor may advise you to stop smoking or at least cut down.
Side Effects
Tell your doctor or pharmacist as soon as possible if you do not feel well while you are taking pravastatin or if you have any questions or concerns.
Do not be alarmed by the following lists of side effects. You may not experience any of them. All medicines can have side effects. Sometimes they are serious but most of the time they are not.
Tell your doctor or pharmacist if you notice any of the following and they worry you. This list includes the more common side effects. Mostly, these are mild:
- constipation, diarrhoea, flatulence (wind)
- stomach upset or pain, feeling or being sick (nausea or vomiting)
- headache
- dizziness
- feeling unusually tired or weak
- unable to sleep, nightmares
- hair loss or change in hair condition, itchy or dry skin
- muscle cramps
- forgetfulness
- swollen breasts
- sexual problems
- mild skin rash
- loss of appetite
- weight loss
- numbness
- anxiety
- problems with sight (e.g. cataracts) or with moving the eye
- problems with hearing
- joint pain
- strange taste
- problems with face muscles
- trembling
- giddiness
Tell your doctor as soon as possible if you notice any of the following.
These may be serious side effects. You may need medical attention. Most of these side effects are rare.
Muscle problems (myopathy)
Medications such as pravastatin can impair the production of certain proteins involved in muscle metabolism and function. This can result in aching muscles, muscle tenderness, stiffness or weakness.
On rare occasions, muscle problems can be serious including muscle breakdown resulting in kidney damage.
Other possible side effects which you should tell your doctor about straight away:
- signs of a potentially fatal condition called interstitial lung disease: dry cough, problems breathing, temperature, losing weight and/or generally feel tired
- tingling in the hands or feet , or numbness
- sharp pain in the upper stomach (pancreatitis)
- feeling depressed
- yellowing of the skin or eyes, and/or pale stools, dark urine (jaundice), also called jaundice
- signs of anaemia, such as tiredness, being short of breath and looking pale
- fever, flushing and/or generally feeling unwell
- frequent, unexplained infections such as fever, severe chills, sore throat or mouth ulcers
- bleeding or bruising more easily than normal
- severe skin rash, itchiness
- sunburn type rash after only a short time in the sun
- pinkish, itchy swellings on the skin, also called hives or nettle rash
If you experience any of the following, stop taking your medicine and contact your doctor immediately or go to Accident and Emergency at your nearest hospital.
These are very serious side effects and are usually very rare. You may need urgent medical attention or hospitalisation.
- shortness of breath
- severe skin rash which may involve blistering and/or peeling of large amounts of skin
- brown or dark coloured urine, with severe muscle aching all through the body, and muscle weakness (due to muscle breakdown)
- mousy odour to the breath, problems with balance and walking, tremor and impaired speech, confusion, unconsciousness
Other side effects not listed above may occur in some patients.
Allergic reactions
If you think you are having an allergic reaction to pravastatin, tell your doctor immediately or go to the Accident and Emergency department at your nearest hospital.
Symptoms of an allergic reaction may include some or all of the following:
- cough, shortness of breath, wheezing or difficulty breathing
- swelling of the face, lips, tongue, or other parts of the body
- rash, itching or hives on the skin
- fainting
- hay fever-like symptoms
After using PRAVASTATIN AN
Storage
Keep your medicine in its original packaging until it is time to take it. If you take your medicine out of its original packaging it may not keep well.
Keep your medicine in a cool dry place where the temperature will stay below 25°C.
Do not store your medicine, or any other medicine, in the bathroom or near a sink. Do not leave it on a window sill or in the car.
Heat and dampness can destroy some medicines.
Keep this medicine where children cannot reach it.
A locked cupboard at least one-and a-half metres above the ground is a good place to store medicines.
Disposal
If your doctor or pharmacist tells you to stop taking this medicine or it has passed its expiry date, your pharmacist can dispose of the remaining medicine safely.
Product description
What PRAVASTATIN AN looks like
PRAVASTATIN AN 10, 20, 40, & 80 (10, 20, 40 & 80 mg pravastatin sodium) are presented in pack size of 30 tablets in blister and 30 & 100 tablets in bottle pack.
PRAVASTATIN AN 10 mg
Yellow, capsule shaped, biconvex, mottled uncoated tablets with notched sides at double bisect, debossed with ‘Y’ on one side and ‘60’ on the other side.
Blister pack AUST R 191713
Bottle pack AUST R 191705
PRAVASTATIN AN 20 mg
Yellow, capsule shaped, biconvex, mottled uncoated tablets with notched sides at double bisect, debossed with ‘Y’ on one side and ‘61’ on the other side.
Blister pack AUST R 191714
Bottle pack AUST R 191716
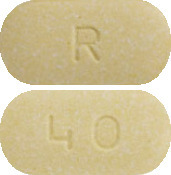
PRAVASTATIN AN 40 mg
Yellow, capsule shaped, biconvex, mottled uncoated tablets debossed with ‘Y’ on one side and ‘58’ on the other side.
Blister pack AUST R 191718
Bottle pack AUST R 191702
PRAVASTATIN AN 80 mg
Yellow, oval shaped, biconvex, mottled uncoated tablets debossed with ‘Y’ on one side and ‘38’ on the other side.
Blister pack AUST R 191706
Bottle pack AUST R 191694
Ingredients
Active ingredient
Pravastatin Sodium
Inactive ingredients
- lactose
- microcrystalline cellulose
- croscarmellose sodium
- magnesium stearate
- heavy magnesium oxide
- iron oxide yellow C177492
Name and Address of the Sponsor
Amneal Pharma Australia Pty Ltd
12 River Street
South Yarra 3141
Australia
Date of Approval
13 November 2013.





 In a pooled analysis of two multicenter, double blind, placebo controlled studies in patients with primary hypercholesterolemia, treatment with pravastatin at a daily dose of 80 mg increased HDL-C and significantly decreased total-C, LDL-C, and TG from baseline after 6 weeks. The efficacy results of the individual studies were consistent with the pooled data. Mean percent changes from baseline after 6 weeks of treatment were: total-C (-27%), LDL-C (-37%), HDL-C (+3%) and TG (-19%), with placebo subtracted changes for LDL-C and TG of -36% and -20% respectively.
In a pooled analysis of two multicenter, double blind, placebo controlled studies in patients with primary hypercholesterolemia, treatment with pravastatin at a daily dose of 80 mg increased HDL-C and significantly decreased total-C, LDL-C, and TG from baseline after 6 weeks. The efficacy results of the individual studies were consistent with the pooled data. Mean percent changes from baseline after 6 weeks of treatment were: total-C (-27%), LDL-C (-37%), HDL-C (+3%) and TG (-19%), with placebo subtracted changes for LDL-C and TG of -36% and -20% respectively. The effect on the combined endpoint of coronary heart disease death or nonfatal myocardial infarction was evident as early as six months after beginning pravastatin therapy.
The effect on the combined endpoint of coronary heart disease death or nonfatal myocardial infarction was evident as early as six months after beginning pravastatin therapy.

 In the Long-term Intervention with Pravastatin in Ischemic Disease (LIPID) study, the effect of pravastatin 40mg daily was assessed in 9014 men and women with normal to elevated serum cholesterol levels (baseline total-C = 4.0-7.0 mmol/L; mean total-C = 5.66 mmol/L; mean total-C/HDL-C ratio = 5.9), and who had experienced either a myocardial infarction or had been hospitalised for unstable angina pectoris in the preceding 3-36 months. Patients with a wide range of baseline levels of triglycerides were included (≤ 5.0 mmol/L) and enrollment was not restricted by baseline levels of HDL cholesterol. At baseline, 82% of patients were receiving aspirin, 76% were receiving antihypertensive medication, and 41% had undergone myocardial revascularisation. Patients in this multicentre, double blind, placebo controlled study participated for a mean of 5.6 years (median = 5.9 years). Treatment with pravastatin significantly reduced the risk for CHD death by 24% (p = 0.0004). The risk for coronary events (either CHD death or nonfatal MI) was significantly reduced by 24% (p < 0.0001) in the pravastatin treated patients. The risk for fatal or nonfatal myocardial infarction was reduced by 29% (p < 0.0001). Pravastatin reduced both the risk for total mortality by 23% (p < 0.0001) and cardiovascular mortality by 25% (p < 0.0001). The risk for undergoing myocardial revascularisation procedures (coronary artery bypass grafting or percutaneous transluminal coronary angioplasty) was significantly reduced by 20% (p < 0.0001) in the pravastatin treated patients. Pravastatin also significantly reduced the risk for stroke by 19% (p = 0.0477). Treatment with pravastatin significantly reduced the number of days of hospitalisation per 100 person years of follow-up by 15% (p < 0.001). The prespecified subgroup (age, sex, hypertensives, diabetics, smokers, lipid subgroups) analyses were conducted using the combined end point of CHD and nonfatal MI. The study was not powered to examine results within each subgroup but formal testing for heterogeneity of treatment effect was undertaken across each of the subgroups and no significant heterogeneity was found (p ≥ 0.08) i.e. a consistant treatment effect was seen with pravastatin therapy across all patient subgroups and event parameters. Among patients who qualified with a history of myocardial infarction, pravastatin significantly reduced the risk for total mortality by 25% (p = 0.0016); for CHD mortality by 23% (p = 0.004); for CHD events by 22% (p = 0.002) and for fatal or nonfatal MI by 25% (p = 0.0008). Among patients who qualified with a history of hospitalisation for unstable angina pectoris, pravastatin significantly reduced the risk for total mortality by 26% (p = 0.0035; for CHD mortality by 26% (p = 0.0358); for CHD events by 29% (p = 0.0001) and for fatal or nonfatal MI by 37% (p = 0.0003). (See Table 5.)
In the Long-term Intervention with Pravastatin in Ischemic Disease (LIPID) study, the effect of pravastatin 40mg daily was assessed in 9014 men and women with normal to elevated serum cholesterol levels (baseline total-C = 4.0-7.0 mmol/L; mean total-C = 5.66 mmol/L; mean total-C/HDL-C ratio = 5.9), and who had experienced either a myocardial infarction or had been hospitalised for unstable angina pectoris in the preceding 3-36 months. Patients with a wide range of baseline levels of triglycerides were included (≤ 5.0 mmol/L) and enrollment was not restricted by baseline levels of HDL cholesterol. At baseline, 82% of patients were receiving aspirin, 76% were receiving antihypertensive medication, and 41% had undergone myocardial revascularisation. Patients in this multicentre, double blind, placebo controlled study participated for a mean of 5.6 years (median = 5.9 years). Treatment with pravastatin significantly reduced the risk for CHD death by 24% (p = 0.0004). The risk for coronary events (either CHD death or nonfatal MI) was significantly reduced by 24% (p < 0.0001) in the pravastatin treated patients. The risk for fatal or nonfatal myocardial infarction was reduced by 29% (p < 0.0001). Pravastatin reduced both the risk for total mortality by 23% (p < 0.0001) and cardiovascular mortality by 25% (p < 0.0001). The risk for undergoing myocardial revascularisation procedures (coronary artery bypass grafting or percutaneous transluminal coronary angioplasty) was significantly reduced by 20% (p < 0.0001) in the pravastatin treated patients. Pravastatin also significantly reduced the risk for stroke by 19% (p = 0.0477). Treatment with pravastatin significantly reduced the number of days of hospitalisation per 100 person years of follow-up by 15% (p < 0.001). The prespecified subgroup (age, sex, hypertensives, diabetics, smokers, lipid subgroups) analyses were conducted using the combined end point of CHD and nonfatal MI. The study was not powered to examine results within each subgroup but formal testing for heterogeneity of treatment effect was undertaken across each of the subgroups and no significant heterogeneity was found (p ≥ 0.08) i.e. a consistant treatment effect was seen with pravastatin therapy across all patient subgroups and event parameters. Among patients who qualified with a history of myocardial infarction, pravastatin significantly reduced the risk for total mortality by 25% (p = 0.0016); for CHD mortality by 23% (p = 0.004); for CHD events by 22% (p = 0.002) and for fatal or nonfatal MI by 25% (p = 0.0008). Among patients who qualified with a history of hospitalisation for unstable angina pectoris, pravastatin significantly reduced the risk for total mortality by 26% (p = 0.0035; for CHD mortality by 26% (p = 0.0358); for CHD events by 29% (p = 0.0001) and for fatal or nonfatal MI by 37% (p = 0.0003). (See Table 5.)
 The safety and efficacy of pravastatin doses above 40 mg daily have not been studied in children. The long-term efficacy of pravastatin therapy in childhood to reduce morbidity and mortality in adulthood has not been established.
The safety and efficacy of pravastatin doses above 40 mg daily have not been studied in children. The long-term efficacy of pravastatin therapy in childhood to reduce morbidity and mortality in adulthood has not been established.
 There was no statistically significant difference in the change in lens opacity between the control and pravastatin treatment groups during this time interval.
There was no statistically significant difference in the change in lens opacity between the control and pravastatin treatment groups during this time interval.