What is in this leaflet
This leaflet answers some common questions about RESOTRANS. It does not contain all the available information. It does not take the place of talking to your doctor or pharmacist.
All medicines have risks and benefits. Your doctor has weighed the risks of you taking RESOTRANS against the benefits this medicine is expected to have for you.
If you have any concerns about taking this medicine, ask your doctor or pharmacist.
Keep this leaflet while being treated. You may need to read it again.
What RESOTRANS is used for
RESOTRANS tablets are used for the treatment of long-standing constipation in adults in whom conventional medicines used to treat constipation (laxatives) fail to provide adequate relief.
RESOTRANS is not used to treat constipation due to other medical conditions including disorders which involve the over-production or under-production of hormones from the endocrine gland, disorders that involve an alteration in normal metabolism, disorders of the nervous system and constipation due to use of medicines including opioid medicines such as codeine, oxycodone and morphine.
RESOTRANS contains the active ingredient prucalopride succinate. It acts on the muscle wall of the gut, helping to restore the normal functioning of the bowel.
Your doctor may have prescribed this medicine for another reason. Ask your doctor if you have any questions about why it has been prescribed for you.
There is no evidence that this medicine is addictive.
This medicine is available only with a doctor's prescription.
Before you take RESOTRANS
When you must not take it
Do not take RESOTRANS if you have an allergy to:
- prucalopride, the active ingredient in the medicine
- any of the ingredients listed at the end of this leaflet.
RESOTRANS contains lactose. If you have been told by your doctor that you have an intolerance to some sugars, contact your doctor before taking this medicine.
Symptoms of an allergic reaction may include rash, itching or hives on the skin, shortness of breath, wheezing or difficulty breathing, swelling of the face, lips, tongue or other parts of the body.
Do not take RESOTRANS if:
- you are on kidney dialysis (a procedure used to remove waste products from the blood of a person with kidney failure)
- if you suffer from perforation or obstruction of the gut wall, or severe inflammation of the intestines
- if you had recent bowel surgery.
If you are not sure whether you should take this medicine, talk to your doctor.
Before you start to take RESOTRANS:
Tell your doctor if you have or have had any medical conditions, especially the following:
- severe kidney disease
- severe liver disease
- any other serious medical problem such as lung or heart disease, neurological or psychiatric disorders or other endocrine disorders, cancer or AIDS for which you are currently under supervision by your doctor
- a history of changes in heart rate (fast, slow or irregular) or heart disease caused by reduced blood flow in the blood vessels of the heart muscle
You must tell your doctor if you:
- are pregnant or planning to become pregnant. It is recommended not to take RESOTRANS if you are pregnant or if you intend to become pregnant, unless your doctor advises you to do so.
- are breastfeeding or wish to breastfeed. When breast-feeding, prucalopride can pass into breast milk, and although there is no evidence that this is harmful, it is better not to use this medicine while breastfeeding unless your doctor advises you to do so.
If you have not told your doctor about any of the above, tell them before you start taking RESOTRANS.
Do not take this medicine if the packaging is torn or shows signs of tampering.
Do not take this medicine beyond the expiry date (month and year) printed on the pack.
The medicine must not be given to children or adolescents (under 18 years of age).
Taking other medicines:
Tell your doctor or pharmacist if you are taking or have recently taken any other medicines, including medicines that you can buy without a prescription from a pharmacy, supermarket or health food shop.
In particular, tell your doctor if you are taking the following medicines:
- ketoconazole (an antifungal agent)
- verapamil
- cyclosporine A
- quinidine
- erythromycin (an antibiotic used to treat infections)
- medicines known to cause irregular heart beat or other heart problems
- atropine-like substances
- oral contraceptives
These medicines may be affected by RESOTRANS or may affect how well it works. You may need different amounts of your medicines, or you may need to take different medicines.
You doctor or pharmacist will have more information on medicines to be careful with or avoid while taking this medicine.
RESOTRANS does not interact with the following medicines: warfarin, digoxin and paroxetine.
How to take RESOTRANS
Follow all directions given to you by your doctor or pharmacist carefully. They may differ from the information contained in this leaflet.
How much to take
The usual dose for most patients is one 2 mg tablet once a day. If you are older than 65 years, the starting dose is one 1 mg tablet once a day, which your doctor may increase to 2 mg once a day if needed. Your doctor may also recommend a lower dose of one 1 mg tablet daily if you have severe kidney or liver disease.
How to take it
This medicine can be taken with or without food and drinks, at any time of the day.
When to take it
This medicine should be taken once a day. You must take this medicine every day for as long as your doctor prescribes it.
Your doctor may want to reassess your condition and the benefit of continued treatment after the first 4 weeks and thereafter at regular intervals.
If you forget to take it
If it is almost time for your next dose, skip the dose you missed and take your next dose when you are meant to. Otherwise, take it as soon as you remember, and then go back to taking it as you would normally.
Do not take a double dose to make up for the dose that you missed. This may increase the chance of you getting an unwanted side effect.
If you have trouble remembering to take your medicine, ask your pharmacist for some hints.
If you stop taking it
If you stop taking RESOTRANS, your constipation symptoms may come back again.
If you have taken too much (overdose)
Immediately telephone your doctor or the Poisons Information Centre for advice or go to Accident and Emergency at your nearest hospital, if you think that you or anyone else may have taken too much RESOTRANS. Do this even if there are no signs of discomfort or poisoning. You may need urgent medical attention.
Poisons Information Centre telephone numbers:
- Australia: 13 11 26
- New Zealand: 0800 POISON or 0800 764 766.
Keep these telephone numbers handy.
It is important to keep to the dose as prescribed by your doctor. If you have taken more RESOTRANS than you should, it is possible that you will get diarrhoea, headache and/or nausea. In case of diarrhoea, make sure that you drink enough water.
If you have any further questions on the use of this medicine, ask your doctor or pharmacist.
While you are taking RESOTRANS
If you experience severe diarrhoea after taking RESOTRANS, certain medicines such as the oral contraceptive pill may not work properly and the use of an extra method of contraception is recommended.
Things you must do
- Always follow your doctor's instructions carefully
- Tell your doctor immediately if you become pregnant while you are taking this medicine
- Tell your doctor immediately if you experience changes in mood or behaviour, or if your depression gets worse while you are taking this medicine
- Tell your doctor or pharmacist that you are taking this medicine if you are about to be started on any new medicines.
Things you must not do
- Do not give your medicine to anyone else, even if they have the same condition as you.
- Do not use this medicine to treat any other complaints unless your doctor tells you to.
- Do not stop taking your medicine or lower the dose without checking with your doctor.
Things to be careful of
Be careful driving or operating machinery until you know how RESOTRANS affects you. RESOTRANS has been associated with dizziness and fatigue particularly during the first day of treatment which may have an effect on driving and using machines.
If you have any of these symptoms, do not drive, operate machinery or do anything else that could be dangerous.
Side Effects
All medicines can have side effects. Sometimes they are serious, most of the time they are not. You may need medical attention if you get some side effects.
Do not be alarmed by this list of possible side effects. You may not experience any of them.
Ask your doctor or pharmacist to answer any questions you may have.
Tell your doctor if you experience any of the following and they worry you:
- Headache or migraine
- nausea
- weakness
- dizziness or spinning sensation (vertigo)
- fatigue
- abnormal bowel sounds
- flatulence
- general feeling of discomfort or uneasiness (malaise)
- back pain
Tell your doctor as soon as possible if you have any of the following as you may need medical attention:
- decreased appetite
- fever
- diarrhoea
- vomiting
- disturbed digestion (dyspepsia)
- increase in frequency of passing urine (pollakiuria)
- abdominal pain
Tell your doctor immediately if you notice any of the following:
- suicidal thoughts or attempts
- tremors
- pounding heart
- rectal bleeding.
Other side effects not listed above may also occur in some people. Tell your doctor if you notice any other effects.
After using RESOTRANS
Storage
Keep your tablets in their blister pack until it is time to take them.
If you take the tablet out of the blister pack, they may not keep well.
Keep RESOTRANS in a cool dry place where the temperature stays below 30°C. Do not store this medicine or any other medicines in a bathroom or near a sink. Do not leave it in the car or on window sills.
Heat and dampness can destroy some medicines.
Keep this medicine where children cannot reach it. A locked cupboard at least one-and-a-half metres above the ground is a good place to store medicines.
Disposal
If your doctor tells you to stop taking RESOTRANS or the tablets have passed their expiry date, ask your pharmacist what to do with any tablets that are left over.
Product Description
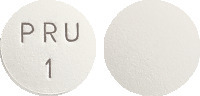
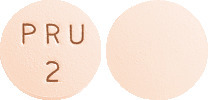
What it looks like
RESOTRANS 1 mg tablets are white to off-white, round, biconvex tablets marked PRU 1 on one side.
RESOTRANS 2 mg tablets are pink, round, biconvex shaped tablets marked PRU 2 on one side.
Ingredients
The active ingredient in RESOTRANS tablets is prucalopride succinate. The 1 mg tablet contains 1 mg of prucalopride and the 2 mg tablet contains 2 mg of prucalopride in pack sizes of 7 and 28 film-coated tablets.
The other ingredients in the 1 mg tablet are lactose monohydrate, microcrystalline cellulose, magnesium stearate, colloidal anhydrous silica and Opadry II complete film coating system 33G28707 WHITE (ARTG PI No 107234).
The other ingredients in the 2 mg tablet are lactose monohydrate, microcrystalline cellulose, magnesium stearate, colloidal anhydrous silica and Opadry II complete film coating system 33G34847 PINK (ARTG PI No 107235).
Sponsor
Amdipharm Mercury (Australia) Pty Ltd
Level 9, 76 Berry Street
North Sydney NSW 2060
Ph: 1800 627 680
Amdipharm Mercury (Australia) Pty Ltd is an ADVANZ PHARMA company
This leaflet was prepared in December 2022.
TGA registration number:
1mg tablet - AUST R 176747
2mg tablet - AUST R 176746
Published by MIMS February 2023

 A total of 564 elderly patients (≥ 65 years) with chronic constipation were treated with Resotrans in double-blind studies, with a total exposure of 63 person years. Most patients in the phase II/III double-blind placebo controlled studies were younger than 65 years. The incidence of adverse events in the < 65 years old group was 71.2% (1534 out of 2153 patients) in the Resotrans group, and 61.6% (712 out of 1155) in the placebo group. In the group of patients older than 65 years, the incidence of adverse events in the Resotrans group was 58.7% (331 out of 564) and in the placebo group 52.8% (113 out of 214). Similar to the younger age group, the most common adverse events with Resotrans treatment among the elderly (> 65 years) groups were gastrointestinal disorders and headache. No clinically meaningful increase of adverse events was observed in Resotrans treated groups as compared to placebo group.
A total of 564 elderly patients (≥ 65 years) with chronic constipation were treated with Resotrans in double-blind studies, with a total exposure of 63 person years. Most patients in the phase II/III double-blind placebo controlled studies were younger than 65 years. The incidence of adverse events in the < 65 years old group was 71.2% (1534 out of 2153 patients) in the Resotrans group, and 61.6% (712 out of 1155) in the placebo group. In the group of patients older than 65 years, the incidence of adverse events in the Resotrans group was 58.7% (331 out of 564) and in the placebo group 52.8% (113 out of 214). Similar to the younger age group, the most common adverse events with Resotrans treatment among the elderly (> 65 years) groups were gastrointestinal disorders and headache. No clinically meaningful increase of adverse events was observed in Resotrans treated groups as compared to placebo group. The primary efficacy endpoint was the proportion (%) of subjects that reached normalisation of bowel movements defined as an average of three or more spontaneous, complete bowel movements (SCBM) per week over the 12 week treatment period. The main secondary efficacy parameter was the proportion of patients with an average increase of ≥ 1 SCBM per week from run-in. A summary of primary efficacy data for individual pivotal studies is provided in Table 3. Both doses were statistically superior (p < 0.001) to placebo at the primary endpoint in each of the three studies, with no incremental benefit of the 4 mg over the 2 mg dose.
The primary efficacy endpoint was the proportion (%) of subjects that reached normalisation of bowel movements defined as an average of three or more spontaneous, complete bowel movements (SCBM) per week over the 12 week treatment period. The main secondary efficacy parameter was the proportion of patients with an average increase of ≥ 1 SCBM per week from run-in. A summary of primary efficacy data for individual pivotal studies is provided in Table 3. Both doses were statistically superior (p < 0.001) to placebo at the primary endpoint in each of the three studies, with no incremental benefit of the 4 mg over the 2 mg dose. Results from the analyses of proportion of patients achieving an average of ≥ 3 SCBM per week during weeks 1-4 were similar to that for the primary efficacy endpoint. Both doses were significantly superior (p < 0.001) to placebo in each of the three studies.
Results from the analyses of proportion of patients achieving an average of ≥ 3 SCBM per week during weeks 1-4 were similar to that for the primary efficacy endpoint. Both doses were significantly superior (p < 0.001) to placebo in each of the three studies. C18H26ClN3O3.C4H6O4. Molecular weight: 485.96.
C18H26ClN3O3.C4H6O4. Molecular weight: 485.96.
