What is in this leaflet
This leaflet answers some common questions about Actonel.
It does not contain all the available information. It does not take the place of talking to your doctor or pharmacist.
All medicines have risks and benefits. Your doctor has weighed the risks of you taking Actonel against the benefits this medicine is expected to have for you.
If you have any concerns about taking this medicine, ask your doctor or pharmacist.
Keep this leaflet with the medicine. You may need to read it again.
What Actonel is used for
Actonel is used to treat bone disease and belongs to a group of medicines called bisphosphonates.
Actonel works directly on your bones to make them stronger and therefore less likely to break or fracture.
Actonel 5mg daily, 35mg Once-a-Week and 150mg Once-a-Month tablets are used to treat:
- osteoporosis (brittle or fragile bones that may fracture easily)
- osteoporosis caused by taking steroids
Actonel 30mg tablets are used to treat:
- Paget's disease of the bone.
These conditions are caused by changes in the way bone is normally maintained.
Understanding bone
Bone is a living tissue consisting of calcium and other minerals. Throughout life, old bone is constantly broken down and replaced with new bone. After the age of 35, bone loss may occur faster than your body can replace it. If you lose too much bone then they become weaker and are more likely to break.
Osteoporosis
Osteoporosis (brittle bone disease) is a disease that causes bones to become weaker. Weak bones break (fracture) easily.
Many patients with osteoporosis have no symptoms and may not even know that they have osteoporosis. However osteoporosis makes you more likely to break bones when you have a fall or bump. The spine, hip and wrist are the most likely bones to break, although this can happen to any bone in your body. Osteoporosis can also cause back pain, height loss and a curved back.
Osteoporosis is common in women after the menopause (change of life) and is also more likely to occur in women who have reached the menopause early. Osteoporosis can also occur in women who have not yet reached menopause, and in men.
Long term steroid treatment can also lead to osteoporosis in both men and women.
Actonel works by slowing down the process of old bone being removed. This allows the bone-forming cells time to rebuild normal bone.
Actonel also helps to rebuild bone mass. This creates stronger bone which is less likely to fracture. Therefore Actonel can help reverse the progression of osteoporosis.
Paget's disease of the bone
Paget's disease occurs when the process of bone remodelling happens too quickly and in a disordered way. The new bone that is produced is weaker than normal and the affected bones may become enlarged, deformed, painful and may fracture. The skull, spine, legs, collar bone and pelvic bone are the most commonly affected.
Do not give Actonel to children or adolescents under 18 years of age. There have been no studies of its effects in this age group.
There is no evidence that Actonel is addictive.
This medicine is available only with a doctor's prescription.
Before you take Actonel
When you must not take Actonel
Do not take Actonel if you:
- have an allergy to Actonel or any of the ingredients listed at the end of this leaflet
- are unable to stand or sit upright for at least 30 minutes
- have a condition called hypocalcaemia (a low level of calcium in the blood)
- have severe kidney problems
Do not take Actonel if you are pregnant. Actonel is not recommended for use during pregnancy, unless you and your doctor have discussed the risks and benefits involved.
Do not take Actonel if you are breastfeeding. It is not known whether Actonel passes into breast milk.
Do not take Actonel after the expiry date printed on the pack. If you take this medicine after the expiry date has passed, it may not work as well.
Do not take Actonel if the packaging is torn or shows signs of tampering.
Talk to your doctor or pharmacist if you are not sure whether you should start taking Actonel.
Before you start to take it
Tell your doctor or pharmacist if you have allergies to:
- any other medicines
- any other substances, such as foods, preservatives or dyes
Tell your doctor if you are pregnant or intend to become pregnant. Your doctor will discuss the possible risks and benefits of using Actonel during pregnancy.
Tell your doctor or pharmacist if you are breastfeeding or plan to breastfeed.
Tell your doctor if you have or have had any medical conditions, especially the following:
- disturbances of bone and mineral metabolism (for example vitamin D deficiency, parathyroid hormone abnormalities)
- problems with the tube that takes food from your mouth to your stomach (oesophagus) such as ulcers
- pain, swelling or numbness of the jaw or a "heavy jaw feeling" or loosening of a tooth
Check with your doctor or dentist to see if a dental check-up is required before starting Actonel. This is especially important if you are receiving medicines or therapy used to treat cancer or taking corticosteroids, such as prednisone or cortisone.
Tell your doctor about any of the above, before you start taking Actonel.
Taking other medicines
Tell your doctor or pharmacist if you are taking any other medicines, including any that you buy without a prescription from your pharmacy, supermarket or health food shop.
Some medicines and Actonel may interfere with each other if taken at the same time. These include:
- Antacids, medicines used to treat indigestion eg Gaviscon, Mylanta
- Other products containing calcium
- Iron supplements
Check with your doctor or pharmacist if you are not sure whether you are taking any of these products. You may need to stop taking these products or take them at a different time of day to Actonel.
You can take aspirin while you are being treated with Actonel.
Your doctor and pharmacist may have more information on medicines to be careful with while taking Actonel.
How to take Actonel
How much to take
For osteoporosis, the usual dose is one 5mg tablet each day, one Actonel 35mg tablet once a week or one 150mg tablet once a month.
For Paget's disease of the bone, the usual dose is one 30 mg tablet each day for 2 months.
Follow all directions given to you by your doctor or pharmacist.
If you do not understand the instructions on the box, ask your doctor or pharmacist for help.
How to take it
Take your Actonel tablet in the morning, at least 30 minutes before your first meal, drink or medication of the day. Actonel is most effective when your stomach is empty.
Take your Actonel tablet while sitting or standing upright. Do not lie down immediately after swallowing it. It is important to stay upright, for example, sitting, standing or walking around, for at least 30 minutes after swallowing your tablet. It is also very important to stay upright until after you have eaten your first food of the day. This will help make sure the tablet reaches your stomach quickly and helps avoid irritation to your oesophagus.
Swallow your Actonel tablet whole with a glass of plain water. Do not chew or suck the tablet. It is important to take Actonel with plain water only (120 mL), not mineral water. Mineral water and other drinks, including fruit juices, coffee and tea, will reduce the effect of Actonel.
When to take it
Take Actonel in the morning, 30 minutes to 1 hour before your first meal, drink or medication of the day.
Take your Actonel 5mg and 30mg tablet at the same time of day every day. Taking your tablets at the same time each day will have the best effect. It will also help you remember when to take the tablets.
Take your Actonel 35mg Once-a-Week tablet on the same day each week. This tablet should be taken each week. Choose a day of the week that suits you the best.
Take your Actonel 150mg Once-a-Month tablet on the same day each month. This tablet should be taken each month. Choose a day of the month that suits you the best.
If you forget to take your tablet
For Actonel 5mg and 30mg tablets:
If it is almost time for your next tablet skip the tablet you missed and take your next tablet when you are meant to.
Do not take a double dose to make up for the tablet that you missed. This may increase the chance of you getting an unwanted side effect.
For Actonel 35mg Once-a-Week tablets:
If you have forgotten to take your 35mg tablet, just take your tablet on the day you remember.
Do not take two tablets in one day to make up for the tablet you missed. Return to taking one tablet once a week, as originally scheduled on your chosen day.
For Actonel 150mg Once-a-Month tablets:
If you have forgotten to take your 150mg tablet, and your next monthly dose is more than 7 days ahead just take one tablet the next morning.
If you have forgotten to take your 150mg tablet, and your next monthly dose is within 7 days do not take it. Return to taking one tablet once a month, as originally scheduled on your chosen day.
If you are not sure what to do, ask your doctor or pharmacist.
If you have trouble remembering to take your medicine, ask your pharmacist for some hints.
How long to take it
Continue taking Actonel for as long as your doctor recommends it.
Do not stop taking Actonel without checking with your doctor or pharmacist.
If you take too much (overdose)
Immediately telephone your doctor or pharmacist or the Poisons Information Centre (13 11 26) or go to accident and emergency at your nearest hospital.
If you or somebody else has accidentally taken a large number of tablets, drink a full glass of milk or antacids. Do this even if there are no signs of discomfort or poisoning. You may need urgent medical attention.
While you are using Actonel
Things you must do
Tell any other doctors, dentists, and pharmacists who are treating you that you are taking Actonel.
If you require a dental procedure, tell your dentist that you are taking Actonel. Invasive dental procedures should be avoided where possible.
This type of medicine may cause jaw-bone problems in some people. Jaw-bone problems may include infection, and delayed healing after teeth are pulled out or other work that involves drilling into the jaw.
If you develop a toothache, jaw pain, painful exposed bone or swelling, especially following dental work, tell your doctor or dentist immediately.
Speak to your doctor and dentist about good oral hygiene and regular dental check-ups while you are using Actonel.
If you are about to be started on any new medicine, tell your doctor, dentist or pharmacist that you are taking Actonel.
If you become pregnant while taking Actonel tell your doctor or pharmacist.
If you develop new or unusual pain in your hip or thigh, tell your doctor.
Rarely, patients have experienced fracture in a specific part of the thigh bone.
Things you must not do
Do not lie down for 30 minutes after taking Actonel.
Do not have any food or drink, except for plain water for 30 minutes after taking Actonel.
Do not give Actonel to anyone else, even if they have the same condition as you.
Do not take Actonel to treat any other complaints unless your doctor or pharmacist tells you to.
Do not stop taking Actonel without checking with your doctor or pharmacist.
Side Effects
Tell your doctor or pharmacist as soon as possible if you do not feel well while you are taking Actonel.
All medicines can have side effects. Sometimes they are serious, most of the time they are not. You may need medical treatment if you get some of the side effects.
Ask your doctor or pharmacist to answer any questions you may have.
Tell your doctor or pharmacist if you notice any of the following and they worry you:
- stomach pain
- diarrhoea
- aching muscles, joints or bones
- headache
- nausea
- runny nose
- sore throat
- dizziness
These side effects are usually mild.
Tell your doctor immediately if you notice any of the following:
- skin rash or redness of the skin, sometimes made worse by sunlight, itchiness
- blurred vision, pain or redness in the eyes
- problems with your jaw or teeth, associated with delayed healing and/or infection often following a tooth extraction or invasive dental work
These side-effects are rare.
If any of the following happen, stop taking Actonel and tell your doctor immediately:
- difficulty or pain on swallowing
- chest pain
- new or worsening heartburn
These side effects may be due to irritation or ulceration of the food pipe. They may worsen if you continue taking the tablets. These side effects are rare.
If any of the following happen, stop taking Actonel and tell your doctor immediately or go to accident and emergency at your nearest hospital:
- swelling of the face, lips, mouth, throat or tongue
- severe skin reactions
These may be serious side effects. You may need urgent medical attention.
Other side effects not listed above may occur in some patients.
Tell your doctor or pharmacist if you notice anything that is making you feel unwell.
Do not be alarmed by this list of possible side effects. You may not experience any of them.
After using Actonel
Storage
Keep your tablets in the pack until it is time to take them. If you take the tablets out of the pack they may not keep well.
Keep your tablets in a cool dry place where the temperature stays below 25°C.
Do not store Actonel or any other medicine in the bathroom or near a sink.
Do not leave medicines in the car on hot days or on window sills. Heat and dampness can destroy some medicines.
Keep medicines where children cannot reach it. A locked cupboard at least one-and-a-half metres above the ground is a good place to store medicines.
Disposal
If your doctor or pharmacist tells you to stop taking Actonel or the tablets have passed their expiry date, ask your pharmacist what to do with any tablets that are left over.
Product description
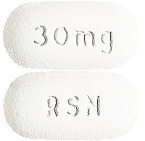
What Actonel looks like
Actonel is available in four types of tablets:
- Actonel 5mg - oval yellow tablet, with RSN marked on one side and 5mg marked on the other
- Actonel 30mg - oval white tablet, with RSN marked on one side and 30mg marked on the other
- Actonel 35mg Once-a-Week - oval light orange tablet, with RSN marked on one side and 35mg marked on the other
- Actonel 150mg - oval light blue tablet, with RSN marked on one side and 150 marked on the other.
Ingredients
Active ingredient:
Each Actonel 5mg tablet contains 5mg risedronate sodium per tablet
Each Actonel 30mg tablet contains 30mg risedronate sodium per tablet
Each Actonel 35mg Once-a-Week tablet contains 35 mg risedronate sodium per tablet
Actonel 150mg Once-a-Month tablets: 150mg risedronate sodium per tablet
Other inactive ingredients include:
- microcrystalline cellulose
- lactose (5mg, 30mg and 35mg only)
- crospovidone
- magnesium stearate
- hypromellose
- macrogol 400
- macrogol 8000
- silicon dioxide
- titanium dioxide
- hydroxypropylcellulose
- iron oxide yellow (5mg and 35mg only)
- iron oxide red (35mg tablet only)
- indigo carmine CI73015 (150mg tablet only)
Actonel does not contain sucrose, gluten, tartrazine or any other azo dyes.
The 5mg and 30mg tablets are supplied in pack sizes of 28 tablets.
The 35mg tablets are supplied in pack sizes of 1 and 4 tablets.
The 150mg tablets are supplied in a pack size of 1 tablet.
Australian Registration Numbers:
Actonel 5 mg - AUST R 74135
Actonel 30 mg - AUST R 74136
Actonel 35 mg - AUST R 82746
Actonel 150 mg - AUST R 150618
Supplier
Actonel is supplied in Australia by:
Theramex Australia Pty Ltd
Level 34, 60 Margaret Street,
Sydney NSW 2000
1800 THERAMEX or 1800 843 726
This leaflet was revised in February 2019
Published by MIMS June 2019




 Three patients that received Actonel 30 mg/day experienced acute iritis in one supportive study. All three patients recovered from their events; however, in one of these patients, the event recurred during Actonel treatment and again during treatment with pamidronate. All patients were effectively treated with topical steroids.
Three patients that received Actonel 30 mg/day experienced acute iritis in one supportive study. All three patients recovered from their events; however, in one of these patients, the event recurred during Actonel treatment and again during treatment with pamidronate. All patients were effectively treated with topical steroids.
 The incidence of nonvertebral fractures in the pooled analysis (RVN and RVE) was lower in the 5 mg risedronate group than in the placebo group for all fractures at these sites combined, as well as for the wrist, humerus, pelvis and leg separately. This difference was significant for all nonvertebral osteoporosis related fractures (p = 0.005), as well as for the humerus (p = 0.024) and pelvis (p = 0.044), while a trend was seen at the wrist (p = 0.075) (Table 4).
The incidence of nonvertebral fractures in the pooled analysis (RVN and RVE) was lower in the 5 mg risedronate group than in the placebo group for all fractures at these sites combined, as well as for the wrist, humerus, pelvis and leg separately. This difference was significant for all nonvertebral osteoporosis related fractures (p = 0.005), as well as for the humerus (p = 0.024) and pelvis (p = 0.044), while a trend was seen at the wrist (p = 0.075) (Table 4).

 A second study of similar design enrolled 290 patients with continuing, long-term use (> 6 months) of corticosteroids for rheumatic, skin and pulmonary diseases. The baseline mean lumbar spine BMD was low (1.64 SD below the young healthy population mean), with 28% of the patients more than 2.5 SD below the mean. All patients in this study received supplemental calcium 1000 mg/day. Patients also received supplemental vitamin D 400 IU/day. After 1 year of treatment, the BMD of the placebo group remained near baseline levels at the lumbar spine, femoral neck and trochanter. Actonel 5 mg once daily improved bone mass with a statistically significant mean increase compared to placebo of 2.7% at the lumbar spine and 1.9% at the femoral neck as shown in Figure 5. At the trochanter, a statistically significant increase from baseline was demonstrated (2.4%). Actonel was effective regardless of age, race, gender, underlying disease, corticosteroid dose or baseline BMD.
A second study of similar design enrolled 290 patients with continuing, long-term use (> 6 months) of corticosteroids for rheumatic, skin and pulmonary diseases. The baseline mean lumbar spine BMD was low (1.64 SD below the young healthy population mean), with 28% of the patients more than 2.5 SD below the mean. All patients in this study received supplemental calcium 1000 mg/day. Patients also received supplemental vitamin D 400 IU/day. After 1 year of treatment, the BMD of the placebo group remained near baseline levels at the lumbar spine, femoral neck and trochanter. Actonel 5 mg once daily improved bone mass with a statistically significant mean increase compared to placebo of 2.7% at the lumbar spine and 1.9% at the femoral neck as shown in Figure 5. At the trochanter, a statistically significant increase from baseline was demonstrated (2.4%). Actonel was effective regardless of age, race, gender, underlying disease, corticosteroid dose or baseline BMD.
 During the first 180 days of the active controlled study, 85% (51/60) of Actonel treated patients demonstrated a ≥ 75% reduction from baseline in excessive SAP levels (difference between measured level and midpoint of the normal range). This was achieved with 2 months of treatment compared to 20% (12/60) in the etidronate treated group with 6 months of treatment (p < 0.001).
During the first 180 days of the active controlled study, 85% (51/60) of Actonel treated patients demonstrated a ≥ 75% reduction from baseline in excessive SAP levels (difference between measured level and midpoint of the normal range). This was achieved with 2 months of treatment compared to 20% (12/60) in the etidronate treated group with 6 months of treatment (p < 0.001). Response to Actonel therapy was similar in patients with Paget's disease, irrespective of disease severity. Table 5 shows the mean percent reduction from baseline at day 180 in excess SAP levels in patients with mild, moderate or severe disease.
Response to Actonel therapy was similar in patients with Paget's disease, irrespective of disease severity. Table 5 shows the mean percent reduction from baseline at day 180 in excess SAP levels in patients with mild, moderate or severe disease. Response to Actonel was similar between patients who had previously received antipagetic therapy and those who had not. In the active controlled study, four patients previously nonresponsive to one or more courses of antipagetic therapy (calcitonin, etidronate) responded to treatment with Actonel 30 mg daily (defined by at least a 30% change from baseline). Each of these patients achieved at least 90% reduction from baseline in excess serum alkaline phosphatase levels with three patients achieving normalisation of serum alkaline phosphatase levels.
Response to Actonel was similar between patients who had previously received antipagetic therapy and those who had not. In the active controlled study, four patients previously nonresponsive to one or more courses of antipagetic therapy (calcitonin, etidronate) responded to treatment with Actonel 30 mg daily (defined by at least a 30% change from baseline). Each of these patients achieved at least 90% reduction from baseline in excess serum alkaline phosphatase levels with three patients achieving normalisation of serum alkaline phosphatase levels.
