What is in this leaflet
This leaflet answers some common questions about ADESAN.
It does not contain all the available information. It does not take the place of talking to your doctor or pharmacist.
All medicines have benefits and risks. Your doctor has weighed the risks of you taking ADESAN against the benefits expected for you.
If you have any concerns about taking this medicine, talk to your doctor or pharmacist.
Keep this leaflet with your medicine. You may need to read it again.
What ADESAN is used for
ADESAN is a type of medicine called an angiotensin II receptor antagonist (or blocker).
ADESAN is used to treat high blood pressure, also called hypertension.
ADESAN is also used to treat heart failure. It is used in combination with other medicines to treat your condition.
Hypertension:
All people have blood pressure. This pressure helps to push blood all around your body. Your blood pressure changes during the day, depending on how busy you are or how you are feeling.
You have hypertension (high blood pressure) when your blood pressure stays higher than is needed, even when you are calm and relaxed.
Regular blood pressure checks are the only way of knowing that you have hypertension. There are usually no symptoms of hypertension and you may feel fine. If hypertension is not treated, serious health problems such as stroke or heart attack and heart or kidney failure may occur.
ADESAN lowers blood pressure by dilating (expanding) small blood vessels from the heart, letting the blood be pumped around the body more easily.
Heart Failure:
Heart failure means that the heart muscle cannot pump blood strongly enough to supply all the blood needed throughout the body. Heart failure is not the same as heart attack and does not mean that the heart stops working.
Heart failure may start off with no symptoms, but as the condition progresses, patients may feel short of breath or may get tired easily after light physical activity such as walking. Some patients may wake up short of breath at night. Fluid may collect in different parts of the body, often first noticed as swollen ankles and feet.
ADESAN helps to treat heart failure and may improve your symptoms.
One of the ways ADESAN helps heart failure is that it widens the blood vessels, so that the heart does not have to pump as hard to move the blood around the body. This also means that when you place extra demands on your heart, such as during exercise, the heart may cope better so you may not get short of breath as easily.
When used to treat heart failure, ADESAN is almost always used with other medicines called diuretics or fluid tablets. These medicines help the kidney get rid of excess fluid from the body.
Your doctor will have explained why you are being treated with ADESAN and told you what dose to take.
Ask your doctor if you have any questions about why this medicine has been prescribed for you. Your doctor may prescribe it for another reason.
This medicine is not addictive.
It is available only with a doctor's prescription.
This medicine may affect your ability to drive a car or operate machinery.
There is not enough information to recommend the use of this medicine for children.
Before you take ADESAN
When you must not take it
Do not take ADESAN if you have an allergy to:
- any medicine containing candesartan cilexetil
- any of the ingredients listed at the end of this leaflet
- any medicine containing an angiotensin II receptor antagonist (or blocker)
Some of the symptoms of an allergic reaction may include
- shortness of breath
- wheezing or difficulty breathing
- swelling of the face, lips, tongue or other parts of the body
- rash, itching or hives on the skin
Do not take ADESAN if you have:
- severe liver disease and/or conditions associated with impaired bile flow (cholestasis)
Do not take ADESAN if you are taking blood pressure medicine containing aliskiren, especially if you have diabetes mellitus or have kidney problems.
Do not take this medicine if you are pregnant or planning to become pregnant. It may affect your baby if you take it during pregnancy.
Do not breast-feed if you are taking this medicine. It is not known if ADESAN passes into breast milk.
Do not give ADESAN to children. There is no information about its use in children, so ADESAN is not recommended for children.
Do not take this medicine after the expiry date printed on the pack or if the packaging is torn or shows signs of tampering. If it has expired or is damaged, return it to your pharmacist for disposal.
If you are not sure whether you should take this medicine, talk to your doctor.
Before you start to take it
Tell your doctor if you have allergies to any other medicines, foods, preservatives or dyes.
Tell your doctor if you have any of the following medical conditions:
- kidney problems
- liver problems
- heart problems
- recent excessive vomiting or diarrhoea
- a condition called primary hyperaldosteronism
You may have to take a lower dose of ADESAN if you have these conditions.
If you have not told your doctor about any of the above, tell him/her before you start taking ADESAN.
Taking other medicines
Tell your doctor or pharmacist if you are taking any other medicines, including any that you get without a prescription from a pharmacy, supermarket or health food shop.
Some medicines and ADESAN may interfere with each other. These include:
- any medicines containing potassium, including salt substitutes
- diuretics (fluid tablets)
- lithium, a medicine used to treat mood swings and some types of depression
- Non-steroidal anti-inflammatory drugs (NSAIDs), medicines used to relieve pain, swelling and other symptoms of inflammation, including arthritis
- Angiotensin-converting-enzyme (ACE) inhibitors, medicines used to help lower blood pressure, especially if you have diabetes-related kidney problems
- Mineralocorticoid receptor antagonists (MRAs), such as spironolactone and eplerenone, medicines used to treat heart failure
These medicines may be affected by ADESAN or may affect the way ADESAN works. You may need different amounts of your medicines, or you may need to take different medicines.
It may be necessary to have regular blood tests done if you take any of these medicines.
Your doctor and pharmacist have more information on medicines to be careful with or avoid while taking this medicine.
How to take ADESAN
Follow all directions given to you by your doctor and pharmacist carefully. They may differ from the information contained in this leaflet.
If you do not understand the instructions on the box/bottle, ask your doctor or pharmacist for help.
How much to take
The usual dose is one 8 mg tablet or one 16 mg tablet taken daily. Sometimes an increase in dose to 32 mg once daily is needed. Your doctor will tell you the dose of ADESAN you should take.
How to take it
Swallow the tablets whole with a full glass of water.
Do not crush or chew the tablets.
When to take it
Take ADESAN once a day, at about the same time each day. Taking it at the same time each day will have the best effect. It will also help you remember when to take it.
It does not matter if you take ADESAN with food or on an empty stomach.
How long to take it
Continue taking your medicine for as long as your doctor tells you to.
This medicine helps to control your condition, but does not cure it. It is important to keep taking your medicine even if you feel well.
If you forget to take it
If you forget to take a dose, take it as soon as you remember, as long as it is at least 12 hours before your next dose is due. Then go back to taking your medicine as you would normally.
If it is almost time for your next dose, skip the dose you missed and take the next dose when you are meant to.
Do not take a double dose to make up for the dose you missed.
If you are not sure what to do, ask your doctor or pharmacist.
If you have trouble remembering to take your medicine, ask your pharmacist for some hints.
If you take too much (overdose)
Immediately telephone your doctor or the Poisons Information Centre (telephone 13 11 26) for advice, or go to Accident and Emergency at the nearest hospital, if you think that you or anyone else may have taken too much ADESAN. Do this even if there are no signs of discomfort or poisoning. You may need urgent medical attention.
Symptoms of an overdose may include headache and feel sick (nausea), dizzy and very tired.
While you are taking ADESAN
Things you must do
Take ADESAN exactly as your doctor has told you, Your blood pressure will not be well controlled if you do not.
If you are about to be started on any new medicine, remind your doctor and pharmacist that you are taking ADESAN.
Tell any other doctors, dentists and pharmacists who treat you that you are taking this medicine.
If you plan to have surgery (even at the dentist) that needs a general anaesthetic, tell your doctor or dentist that you are taking this medicine. It may affect other medicines used during surgery.
Tell your doctor immediately if you become pregnant or plan to become pregnant while taking this ADESAN. You should not use ADESAN if you are pregnant or thinking about becoming pregnant. Your doctor can discuss treatment options with you.
Be sure to keep all of your doctor's appointments so that your progress can be checked. Your doctor will check your progress and may want to do some tests (e.g. blood tests, blood pressure) from time to time. These tests may help to prevent side effects.
Things you must not do
Do not take ADESAN to treat any other complaints unless your doctor tells you to.
Do not give your medicine to anyone else, even if they have the same condition as you.
Do not stop taking your medicine or change the dosage unless you have discussed it with your doctor.
Things to be careful of
If you feel light-headed, dizzy or faint when getting out of bed or standing up, get up slowly.
Be careful driving or operating machinery until you know how ADESAN affects you. You may feel dizzy when you start taking ADESAN.
If you are taking ADESAN for high blood pressure, drink plenty of water during exercise and hot weather, especially if you sweat a lot. If you do not drink enough water while taking ADESAN, you may faint or feel light-headed or sick. This is because your body doesn't have enough fluid and your blood pressure is low. If you continue to feel unwell, tell your doctor.
If you are taking ADESAN for heart failure, restricted fluid intake is generally recommended. Speak with your doctor about how much water you should drink.
Please talk to your doctor or pharmacist about these possibilities if you think they may bother you.
Lifestyle measures that help reduce heart disease risk
By following these simple measures, you can further reduce the risk from heart disease.
- Quit smoking and avoid second-hand smoke.
- Limit alcohol intake.
- Enjoy healthy eating by:
- eating plenty of vegetables and fruit;
- reducing your saturated fat intake (eat less fatty meats, full fat dairy products, butter, coconut and palm oils, most take-away foods, commercially-baked products). - Be active. Progress, over time, to at least 30 minutes of moderate-intensity physical activity on 5 or more days each week. Can be accumulated in shorter bouts of 10 minutes duration. If you have been prescribed anti-angina medicine, carry it with you when you are being physically active.
- Maintain a healthy weight.
- Discuss your lifestyle and lifestyle plans with your doctor.
- For more information and tools to improve your heart health, call Heartline, the Heart Foundation's national telephone information service, on 1300 36 27 87 (local call cost).
Know warning signs of heart attack and what to do:
- Tightness, fullness, pressure, squeezing, heaviness or pain in your chest, neck, jaw, throat, shoulders, arms or back.
- You may also have difficulty breathing, or have a cold sweat or feel dizzy or light headed or feel like vomiting (or actually vomit).
- If you have heart attack warning signs that are severe, get worse or last for 10 minutes even if they are mild, call triple zero (000). Every minute counts.
Side effects
Tell your doctor or pharmacist as soon as possible if you do not feel well while you are taking ADESAN.
This medicine helps most people but it may have unwanted side effects in a few people.
All medicines can have side effects. Sometimes they are serious, most of the time they are not. You may need medical treatment if you get some of the side effects.
Do not be alarmed by the following list of side effects. You may not experience any of them.
Ask your doctor or pharmacist to answer any questions you may have.
Tell your doctor if you notice any of the following and they worry you:
- headache
- chest or throat infection
- flu-like symptoms
- feeling sick (nausea, vomiting)
- back pain
- dizziness
These side effects are usually mild.
Tell your doctor as soon as possible if you notice any of the following:
- aching muscles, tenderness or weakness in the muscle
The above list includes serious side effects that may require medical attention. Serious side effects are rare.
If any of the following happen, tell your doctor immediately or go to Accident and Emergency at your nearest hospital:
- swelling of the face, lips, tongue or throat
- swelling of the hands, feet or ankles
- harsh sounds when breathing
- rash, itchiness or hives
- jaundice (yellowing of the skin and/or eyes).
- easy bruising or bleeding more easily than normal
- extreme fatigue, tiredness, weakness
- signs of frequent infections such as fever, severe chills, sore throat or mouth ulcers
- worsening of the kidney function (including passing little or no urine, drowsiness, nausea, vomiting breathlessness, loss of appetite and weakness (especially in patients with existing kidney problems or heart failure).
- changes in your potassium, sodium and red or white blood cell levels may occur. Such changes are usually detected by a blood test.
- symptoms that may indicate high potassium levels in the blood include nausea, diarrhoea, muscle weakness and changes in heart rhythm.
The above list includes very serious side effects. You may need urgent medical attention or hospitalisation. These side effects are very rare.
Tell your doctor if you notice anything else that is making you feel unwell. Other side effects not listed above may also occur in some people.
After taking ADESAN
Storage
Keep your tablets in the pack until it is time to take them. If you take the tablets out of the pack they may not keep well.
Keep your tablets in a cool dry place where the temperature stays below 25°C. Protect from light.
Do not store ADESAN or any other medicine in the bathroom or near a sink. Do not leave it on a window sill or in the car. Heat and dampness can destroy some medicines.
Keep it where children cannot reach it. A locked cupboard at least one-and-a-half metres above the ground is a good place to store medicines.
Disposal
If your doctor tells you to stop taking this medicine or the expiry date has passed, ask your pharmacist what to do with any medicine that is left over.
Product description
What it looks like
ADESAN 4 mg: A white to off white round, biconvex tablet debossed with "M" on left side of the breakline and "C" on the right side of the breakline on one side of the tablet and "24" on the other side.
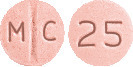
ADESAN 8 mg: A mottled pink, round, biconvex tablet debossed with "M" on left side of the breakline and "C" on right side of the breakline on one side of the tablet and "25" on the other side.
ADESAN 16 mg: A mottled pink, round, biconvex tablet debossed with "M" on left side of the breakline and "C" on right side of the breakline on one side of the tablet and "31" on the other side.
ADESAN 32 mg: A mottled pink, round, biconvex tablet debossed with "MC" above the breakline and "32" below the break line on one side of the tablet and plain on the other side.
All strengths are available in blister pack of 30 tablets.
Ingredients
ADESAN tablet contains 4, 8, 16 or 32 mg of candesartan cilexetil as the active ingredient.
It also contains the following inactive ingredients:
- lactose monohydrate
- carmellose calcium
- glyceryl monostearate
- hyprolose
- iron oxide red CI77491 (ADESAN 8 mg, 16 mg and 32 mg only)
- maize starch
- magnesium stearate
ADESAN tablets contain sugars as lactose.
Supplier
ADESAN is supplied in Australia by:
Alphapharm Pty Ltd trading as Viatris
Level 1, 30 The Bond
30-34 Hickson Road
Millers Point NSW 2000
www.viatris.com.au
Phone: 1800 274 276
This leaflet was prepared in December 2022.
Australian registration numbers:
ADESAN 4 mg: AUST R 171019
ADESAN 8 mg: AUST R 171022
ADESAN 16 mg: AUST R 171016
ADESAN 32 mg: AUST R 171017
ADESAN® is a Viatris company trade mark
ADESAN_cmi\Dec22/00
Published by MIMS February 2023





 The antihypertensive effects of candesartan cilexetil and losartan potassium at their highest recommended doses administered once daily were compared in two randomised, double-blind trials. In a total of 1,268 patients with mild to moderate hypertension who were not receiving other antihypertensive therapy, candesartan cilexetil 32 mg lowered systolic and diastolic blood pressure by 2 to 3 mmHg on average more than losartan potassium 100 mg, when measured at the time of either peak or trough effect.
The antihypertensive effects of candesartan cilexetil and losartan potassium at their highest recommended doses administered once daily were compared in two randomised, double-blind trials. In a total of 1,268 patients with mild to moderate hypertension who were not receiving other antihypertensive therapy, candesartan cilexetil 32 mg lowered systolic and diastolic blood pressure by 2 to 3 mmHg on average more than losartan potassium 100 mg, when measured at the time of either peak or trough effect.

 All-cause mortality was also assessed in pooled populations, CHARM-Alternative and CHARM-Added (HR 0.88, 95% CI 0.79-0.98, p = 0.018) and all three studies (HR 0.91, 95% CI 0.83-1.00, p = 0.055). This corresponds to a relative risk reduction of 12% and 9% respectively and an absolute risk reduction of 2.9 and 1.6% respectively.
All-cause mortality was also assessed in pooled populations, CHARM-Alternative and CHARM-Added (HR 0.88, 95% CI 0.79-0.98, p = 0.018) and all three studies (HR 0.91, 95% CI 0.83-1.00, p = 0.055). This corresponds to a relative risk reduction of 12% and 9% respectively and an absolute risk reduction of 2.9 and 1.6% respectively. Molecular formula: C33H34N6O6. Molecular weight: 610.67.
Molecular formula: C33H34N6O6. Molecular weight: 610.67.