What is in this leaflet
This leaflet is designed to provide answers to some common questions about this medicine. It does not contain all the available information.
All medicines have risks and benefits. Your doctor has weighed the risks of you taking Amisulpride Sandoz against the benefits this medicine is expected to have for you.
If you have any concerns about taking this medicine, ask your doctor or pharmacist.
Keep this leaflet with this medicine. You may need to read it again.
What Amisulpride Sandoz is used for
The name of your medicine is Amisulpride Sandoz. It contains the active ingredient called amisulpride.
Amisulpride Sandoz belongs to a group of medicines called antipsychotics. Amisulpride Sandoz is used to treat symptoms of schizophrenia.
Schizophrenia is a condition, which affects the way you think, feel and/or act. Schizophrenia may cause symptoms such as hallucinations (eg hearing, seeing or sensing things which are not there), delusions, unusual suspiciousness, emotional and social withdrawal. People with schizophrenia may also feel depressed, anxious or tense.
Your doctor may have prescribed Amisulpride Sandoz for another reason.
Ask your doctor if you have any questions about why Amisulpride Sandoz has been prescribed for you.
Before taking it
When you must not take it
Do not take Amisulpride Sandoz if:
-
you have an ALLERGIC REACTION to Amisulpride Sandoz or any of the ingredients listed at the end of this leaflet.
Signs of an allergic reaction may include a skin rash, itching, shortness of breath or swelling of the face, lips or tongue. - you are breastfeeding or plan to breastfeed
-
you are taking the following medicines
- medicines used to treat irregular heart rhythm such as quinidine, disopyramide, amiodarone and sotalol
- cisapride
- antibiotics such as erythromycin and pentamidine, given as an injection into the veins
- levodopa, a medicine used in Parkinson's disease
- thioridazone, an antipsychotic
- methadone, medicine used to treat pain or addiction - the packaging is torn or shows signs of tampering or the tablets do not look quite right
- the expiry date on the pack has passed.
Do not take Amisulpride Sandoz if you have or have had any of the following medical conditions:
- phaeochromocytoma, a rare tumour of the adrenal glands which sit near the kidneys
- tumour of the pituitary gland, a small gland at the base of the brain
- breast cancer
- liver disease.
Amisulpride Sandoz must not be taken by children up to the age of puberty. There is limited information on the use of Amisulpride Sandoz in adolescents and its use is not recommended from puberty to the age of 18 years. If you are not yet 18 years of age, ask your doctor if Amisulpride Sandoz is right for you.
Before you start to take it
Your doctor must know about all the following before you start to take Amisulpride Sandoz.
Tell your doctor if:
- you have had an allergic reaction to any medicine which you have taken previously to treat your current condition.
- you are pregnant, think you may be pregnant or intend to become pregnant. Amisulpride Sandoz is not recommended for use in pregnancy. If you need to take Amisulpride Sandoz during pregnancy you should discuss the benefits and risks of taking it with your doctor.
- you suffer from lactose intolerance because Amisulpride Sandoz tablets contain lactose.
- you have kidney or liver disease, Parkinson's disease or fits (seizures).
- you have problems with the heart and blood vessels.
- you have, or have a history of blood clots.
- you have hyperglycaemia (high sugar levels in the blood) or a family history of diabetes. Your doctor may recommend monitoring your blood sugar levels while you are taking Amisulpride Sandoz.
- you suffer from dementia
- you have any mental/mood changes or suicidal thoughts. Patients (and caregivers of patients) need to monitor for any worsening of their condition and/or the development of thoughts of suicide, suicidal behaviour or thoughts of harming themselves. Seek medical advice immediately if these symptoms present.
- you have risk factors for stroke.
- you have a history, or family history of breast cancer
- you have a history of sleep apnoea.
Taking other medicines
Tell your doctor or pharmacist if you are taking any other medicines, including any that you buy without a prescription from your pharmacy, supermarket or health food store.
Some medicines and Amisulpride Sandoz may interfere with each other. These include:
- other medicines used to treat heart problems such as diltiazem, verapamil, clonidine, digoxin and drugs known as beta blockers (e.g. propranolol)
- medicines used to treat irregular heart rhythm such as quinidine, disopyramide, amiodarone and sotalol
- intravenous amphotericin B, an anti-fungal given by injection into the veins
- other antipsychotics such as thioridazine, clozapine, chlorpromazine, trifluperazine, pimozide, haloperidol, imipramine and lithium
- diuretics
- stimulant laxatives
- glucocorticosteroids
- diagnostics drugs such as tetracosactides
- medicines taken for anxiety or to help you sleep (central nervous system depressants)
- anaesthetics (a medicine used during surgery_
- medicines taken for depression
- some strong pain killers
- antihistamines, medicines to treat allergies, which cause drowsiness
- some medicines taken to control blood pressure.
If you are unsure about any medicine you are taking, you should check with your doctor or pharmacist. They will have more information on medicines to be careful of while you are taking Amisulpride Sandoz.
How to take it
How much to take
Your doctor will tell you how many Amisulpride Sandoz tablets you should take. The dosage is adjusted for each individual and can range from 50mg a day up to 800mg a day. In some cases your doctor may increase the dose to 1200mg a day.
Amisulpride Sandoz tablets should be taken once or twice a day as advised by your doctor. Your doctor may increase or decrease your dose depending on your condition.
Do not take more than the dose your doctor has recommended.
How to take it
Amisulpride Sandoz tablets should be swallowed whole with a glass of water.
When to take it
Amisulpride Sandoz tablets should preferably be taken before meals. Take your prescribed dose at about the same time each day.
How long do I take it
It is important that you do NOT stop taking Amisulpride Sandoz unless your doctor tells you. Do not stop taking your Amisulpride Sandoz just because you feel better. It is very important to continue Amisulpride Sandoz because it will help you stay well.
If you forget to take it
If you forget to take your medicine, take your dose as soon as you remember. Do not take a double dose to make up for the dose that you missed.
If you take too much (overdose)
Immediately telephone your doctor or the Poisons Information Centre (telephone Australia 13 11 26 or New Zealand 0800 POISON or 0800 764766), or go to Accident and Emergency at your nearest hospital, if you think that you or anyone else may have taken too much Amisulpride Sandoz. Show the doctor your pack of tablets. Do this even if there are no signs of discomfort or poisoning.
If you have taken too much Amisulpride Sandoz, the most common signs are drowsiness and slurred speech.
While you are using it
Things you must do
It is very important to continue taking Amisulpride Sandoz because it will help you stay well.
Tell all doctors, dentists and pharmacists who are treating you that you are taking Amisulpride Sandoz.
While you are taking Amisulpride Sandoz, tell your doctor or pharmacist before you start any new medicine.
Make sure you use a contraceptive to prevent pregnancy during treatment with Amisulpride Sandoz. If you become pregnant while taking this medicine, tell your doctor immediately.
Tell your doctor immediately, or go to the nearest hospital, if you have any of the following suicidal thoughts or mental/mood changes:
- thoughts or talk of death or suicide
- thoughts or talk of self-harm or harm to others
- any recent attempts of self-harm
- increase in aggressive behaviour, irritability or agitation
- depressed mood or worsening of depression
Occasionally, the symptoms of depression may include thoughts of suicide or self-harm. These symptoms may continue to get worse during the early stages of treatment until the effect of the medicine becomes apparent. All mentions of suicide or violence must be taken seriously.
Things to be careful of
Amisulpride Sandoz may cause drowsiness in some people.
Be careful driving or operating machinery until you know how Amisulpride Sandoz affects you.
Be careful if you are elderly or unwell.
Some people may experience side effects such as drowsiness, confusion, dizziness and unsteadiness. Amisulpride Sandoz may affect your ability to move or balance. This may increase the risk of a fall, sometimes leading to fractures.
The effects of alcohol could be made worse while taking Amisulpride Sandoz. It is NOT recommended that you drink alcohol while taking Amisulpride Sandoz.
Be careful while taking antihistamines, sleeping tablets or tablets to relieve pain while taking this medicine. Amisulpride Sandoz can increase drowsiness caused by medicines affecting your nervous system.
Things you must NOT do
Do not drive or operate machinery until you know how Amisulpride Sandoz affects you.
Do not give Amisulpride Sandoz to anyone else. Your doctor has prescribed it for you and your condition.
Side Effects
Tell your doctor or pharmacist as soon as possible if you do not feel well while you are taking Amisulpride Sandoz.
Like other medicines, Amisulpride Sandoz can cause some side effects. If they occur, most are likely to be minor and temporary. However, some may be serious and may need medical attention. Some of the side effects are dose related, so it is important that you never exceed your prescribed dose.
Tell your doctor if you notice any of the following and they worry you:
- drowsiness
- weight gain
- dizziness
- increased appetite
- nausea
- vomiting
- constipation
- dry mouth
- blurred vision
- insomnia
- anxiety
- agitation
- problems with orgasm.
These are the most common side effects of Amisulpride Sandoz.
Rare side effects include sleep walking and sleep eating.
Some people may feel dizzy in the early stages of treatment, especially when getting up from a lying or sitting position. This side effect usually passes after taking Amisulpride Sandoz for a few days.
Sometimes trembling, noticeable muscle stiffness or spasm, slowness of movement, excess saliva, restlessness, an overwhelming urge to move and either distress or movements such as pacing, swinging of the legs while seated, rocking from foot to foot, or both can occur. This will usually be reduced if your dose of Amisulpride Sandoz is lowered by your doctor or if your doctor prescribes you an additional medicine.
High blood sugar has been reported in patients taking Amisulpride Sandoz. Symptoms of high sugar levels in the blood include passing more urine than normal, persistent excessive thirst, increased appetite with a loss in weight and weakness.
Some people experience increased sensitivity to the sun or notice symptoms of sunburn (such as redness, itching, swelling, blistering) which may occur more quickly than normal.
Tell your doctor immediately or go to Accident and Emergency at your nearest hospital if you notice any of the following:
- muscle twitching
- abnormal movements mainly of the face or tongue
- fever
- unexplained infections
- faster breathing
- sweating
- muscle stiffness.
- yellowing of the skin and eyes, also called jaundice
- light coloured bowel motions
- dark coloured urine
If this occurs, stop taking Amisulpride Sandoz immediately and contact your doctor.
After prolonged use in women, medicines of this type can cause:
- breast pain
- milk secretion
- an absence of their monthly period
- changes in the regularity of their periods.
Tell your doctor if your monthly periods are absent for six months or more.
After prolonged use in men, medicines of this type can cause breast enlargement or impotence.
Incidences of abnormal liver function have been occasionally reported.
Do not be alarmed by this list of possible side effects. You may not experience any of them.
Tell your doctor if you notice any symptoms that worry you, even if you think the problems are not connected with the medicine or are not listed in this leaflet.
After taking it
Storage
Keep your tablets in the blister pack until it is time to take them. If you take the tablets out of the blister pack they may not keep well.
Keep Amisulpride Sandoz tablets in a cool, dry place where the temperature stays below 30°C.
Do not store Amisulpride Sandoz or any other medicine in the bathroom or near a sink.
Do not leave it in the car or on window sills. Heat and dampness can destroy some medicines.
Keep it where children cannot reach it. A locked cupboard at least one-and-a-half metres above the ground is a good place to store medicines.
There will be an expiry date (month, year) on your Amisulpride Sandoz container. The medicine should not be taken after this date.
Disposal
If your doctor tells you to stop taking Amisulpride Sandoz or the tablets have passed their expiry date, ask your pharmacist what to do with the amount left over.
Product description
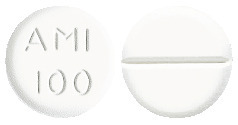
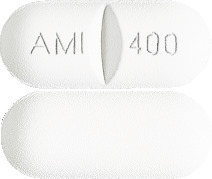
What it looks like
Amisulpride Sandoz tablets are available in three different strengths:
The 100 mg strength is a white, flat faced, breakable tablet, marked "AMI 100".
The 200 mg strength is a white, flat faced, breakable tablet, marked "AMI 200".
The 400 mg strength is a white, film-coated, breakable, oblong tablet, marked "AMI 400".
The 100 mg strength is available in a pack size of 30 tablets.
The 200 mg strength is available in a pack size of 60 tablets.
The 400 mg strength is available in a pack size of 60 tablets.
Ingredients
Active Ingredient
Amisulpride Sandoz 100mg tablets contain 100 mg amisulpride.
Amisulpride Sandoz 200mg tablets contain 200 mg amisulpride.
Amisulpride Sandoz 400mg tablets contain 400 mg amisulpride.
Inactive Ingredients
The tablets also contain:
- sodium starch glycollate type A
- lactose monohydrate
- microcrystalline cellulose (E 460)
- hypromellose (E 464)
- magnesium stearate (E 470).
The 400 mg tablets also contain:
- PEG 40 stearate
- titanium dioxide (E 171).
Manufacturer
Amisulpride Sandoz is distributed in Australia by:
Sandoz Pty Ltd
ABN 60 075 449 553
54 Waterloo Road
Macquarie Park,
NSW 2113
AUSTRALIA
Tel: 1800 634 500
The Australian Registration numbers for Amisulpride Sandoz are as follows:
Amisulpride Sandoz 100mg:
AUST R 128985
Amisulpride Sandoz 200mg:
AUST R 128993
Amisulpride Sandoz 400mg:
AUST R 128994
This leaflet was prepared in September 2020.
®Registered Trademark.
amisulpride-sandoz-ccdsv14-cmiv10-27oct20.
Published by MIMS December 2020


 The following CIOMS frequency rating is used, when applicable: very common ≥ 10%; common ≥ 1 and < 10%; uncommon ≥ 0.1 and < 1%; rare ≥ 0.01 and < 0.1%; very rare < 0.01%; not known (cannot be estimated from available data).
The following CIOMS frequency rating is used, when applicable: very common ≥ 10%; common ≥ 1 and < 10%; uncommon ≥ 0.1 and < 1%; rare ≥ 0.01 and < 0.1%; very rare < 0.01%; not known (cannot be estimated from available data).
