What is in this leaflet
This leaflet answers some common questions about Amizide.
It does not contain all of the available information. It does not take the place of talking to your doctor or pharmacist.
All medicines have benefits and risks. Your doctor has weighed the risks of you taking Amizide against the benefits they expect it will have for you.
If you have any concerns about taking this medicine, talk to your doctor or pharmacist.
Keep this leaflet with your medicine. You may need to read it again.
What Amizide is used for
Amizide is used for:
- oedema, swelling of the ankles, feet and legs
- ascites due to liver disease resulting in fluid accumulation in the stomach area
- lower high blood pressure (hypertension).
Amizide contains a combination of two diuretics, amiloride hydrochloride and hydrochlorothiazide as the active ingredients. It helps reduce the amount of excess fluid in the body by increasing the amount of urine produced, while at the same time, minimizing potassium loss.
Amizide works by making your kidneys pass more water and salt whilst retaining potassium. This helps reduce high blood pressure and some forms of swelling, while at the same time helping to maintain normal levels of potassium in your blood.
Amizide may be taken alone or in combination with other medicines to treat your condition.
Your doctor may have prescribed Amizide for another reason. Ask your doctor if you have any questions about why Amizide has been prescribed for you.
Amizide is available only with a doctor's prescription. There is no evidence that Amizide is addictive.
Before you take Amizide
When you must not take it
Do not take Amizide if you are allergic to medicines containing either amiloride or hydrochlorothiazide or any of the ingredients listed at the end of this leaflet.
Do not take Amizide if you are allergic to medicines which contain sulfur (sulfonamides).
Hydrochlorothiazide, one of the active ingredients of Amizide, is a sulfur containing medicine. Therefore, if you are allergic to sulfur medicines, such as some antibiotics, you are likely to be allergic to Amizide. If you are not sure if you have an allergy to sulfonamide medicines, check with your doctor or pharmacist.
Some of the symptoms of an allergic reaction may include skin rash, itching or hives, swelling of the face, lips or tongue which may cause difficulty in swallowing or breathing, wheezing or shortness of breath.
Do not take Amizide if you have:
- certain kidney problems
- no production of urine
- high potassium levels in your blood (hyperkalaemia), possibly due to a high potassium diet, taking potassium supplements, or other potassium-sparing medication.
Amizide helps maintain normal levels of potassium in your blood. If you are taking potassium tablets or supplements, other potassium-conserving medicines or a potassium rich diet, your potassium levels may increase too much.
Ask your doctor or pharmacist if you are not sure whether you are taking too much potassium.
Do not take Amizide if you are pregnant or intend to become pregnant unless you and your doctor have discussed the risks and benefits involved.
Like most diuretic medicines, Amizide is not recommended for use during pregnancy.
Do not take Amizide if you are breastfeeding or plan to breastfeed.
Amizide passes into breast milk and may affect your baby.
Do not take Amizide if the expiry date (Exp.) printed on the pack has passed.
Do not take Amizide if the packaging shows signs of tampering or the tablets do not look quite right.
Do not give Amizide to children.
The safety of Amizide in children has not been established.
Before you start to take it
Tell your doctor if you are allergic to any other medicines, foods, dyes or preservatives.
Tell your doctor if you have, or have had, any medical conditions, especially the following:
- diabetes
- kidney problems
- liver problems
- heart and lung problems
- asthma
- gout or hyperuricaemia
- systemic lupus erythematosus
- high cholesterol levels.
Your doctor may want to take special care if you have any of these conditions.
If you have not told your doctor about any of the above, tell them before you start taking Amizide.
Taking other medicines
Tell your doctor if you are taking any other medicines, including any that you buy without a prescription from a pharmacy, supermarket or health food shop.
Some medicines may be affected by Amizide, or may affect how well it works. These include:
- preparations which contain potassium
- potassium conserving medicines
- angiotensin converting enzyme (ACE) inhibitors and angiotensin receptor antagonists, a group of medicines used to treat high blood pressure and some heart conditions
- other medicines to treat high blood pressure
- cyclosporin, tacrolimus, medicines used to suppress the immune system
- lithium, a medicine used in the treatment of mood swings and some types of depression
- non-steroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen, naproxen, diclofenac, indomethacin, medicines used to relieve pain, swelling and other symptoms of inflammation including arthritis
- barbiturates such as phenobarbitone, and carbamazepine, medicines used to treat epilepsy
- strong pain killers such as codeine, morphine and dextropropoxyphene
- insulin and tablets used to treat diabetes
- steroid-based medicines such as prednisone, dexamethasone
- adrenaline, a medicine used in emergency situations such as an anaphylactic reaction
- cholestyramine, colestipol resins, medicines used to lower blood cholesterol levels
- medicines used to relax muscles before and during surgery
- medicines used in emergency situations such as adrenaline
- alcohol
These medicines may be affected by Amizide or may affect how well it works. You may need to take different amounts of your medicine, or may need to take different medicines.
Your doctor can tell you what to do if you are taking any of these medicines.
If you are not sure whether you are taking any of these medicines, check with your doctor or pharmacist.
Your doctor and pharmacist have more information on medicines to be careful with or avoid while taking Amizide.
How to take Amizide
How much to take
The usual dose is one or two tablets daily.
Your doctor may advise you to take a different dose. This depends on your condition and whether or not you are taking any other medicines. Your initial dose will be maintained or adjusted until a satisfactory response is noted, but should not exceed 4 tablets per day.
Your doctor may increase your dose if necessary. No more than four tablets a day should be taken.
Follow all directions given to you by your doctor and pharmacist carefully.
They may differ from the information contained in this leaflet.
How to take Amizide
Swallow the tablets with a glass of water.
When to take Amizide
If you are taking Amizide once a day, take it in the morning, for example, at breakfast time.
Amizide takes about two hours to start working.
If you are taking more than one dose a day, take the last dose no later than 6 p.m, unless your doctor tells you otherwise.
Amizide may increase the amount of water (urine) you pass and also the number of times you go to the toilet. By taking the last dose no later than 6 p.m there may be less chance of your sleep being disturbed.
If you forget to take Amizide
If it is almost time for your next dose, skip the dose you missed and take your next dose when you are meant to.
Otherwise, take the missed dose as soon as you remember, and then go back to taking your tablets as you would normally.
Do not take a double dose to make up for the dose you missed.
If you are not sure what to do, ask your doctor or pharmacist.
If you have any questions about this, check with your doctor or pharmacist.
How long to take Amizide for
It is important to take Amizide every day as it helps control your condition and lower the fluid build-up in your body.
Keep taking Amizide for as long as your doctor recommends.
If you take too much Amizide (overdose)
Immediately telephone your doctor, or the Poisons Information Centre (telephone 13 11 26), or go to Accident and Emergency at the nearest hospital, if you think you or anyone else may have taken too much Amizide. Do this even if there are no signs of discomfort or poisoning.
You may need urgent medical attention.
If you take too much Amizide, you may feel thirsty, tired, confused, dizzy, nausea, vomiting, have muscle cramps and a very fast heart rate.
While you are taking Amizide
Things you must do
Before starting any new medicine, tell your doctor or pharmacist that you are taking Amizide.
Tell all the doctors, dentists and pharmacists who are treating you that you are taking Amizide.
If you become pregnant while taking Amizide, tell your doctor immediately.
Tell your doctor if you have any of the following dehydration symptoms:
- excessive vomiting or diarrhoea
- dry mouth, thirst
- weakness, tiredness, drowsiness
- muscle pain or cramps
- fast heart beat
- passing less urine than normal.
You may be dehydrated from losing too much water if you experience any of these symptoms.
If you plan to have surgery, including dental surgery, which needs a general anaesthetic, tell your doctor or dentist that you are taking Amizide.
If you have to have any blood tests, tell your doctor that you are taking Amizide.
Amizide may affect the results of some tests.
Visit your doctor regularly so they can check on your progress.
Your doctor may want to check your blood pressure and potassium levels regularly to make sure Amizide is working properly for you.
Things you must not do
Do not stop taking Amizide, or change the dose, without checking with your doctor.
Do not use Amizide to treat any other conditions unless your doctor tells you to.
Do not give Amizide to anyone else, even if they have the same condition as you.
Things to be careful of
Be careful driving or operating machinery until you know how Amizide affects you.
Amizide may cause drowsiness, dizziness or lightheadedness in some people. If any of these occur, do not drive, operate machinery or do anything else that could be dangerous. Make sure you know how you react to it before you drive a car, operate machinery or do anything else that could be dangerous if you are dizzy or lightheaded.
Be careful getting up from a sitting or lying position.
Dizziness, lightheadedness or fainting may occur, especially when you get up quickly. Getting up slowly may help. If this problem gets worse or continues, talk to your doctor.
Be careful when drinking alcohol or taking strong pain killers while taking Amizide.
Combining Amizide with alcohol or strong pain killers can make you more dizzy or lightheaded.
Be aware of foods or drinks that have a high potassium content.
Amizide helps to maintain normal potassium levels in your body. However, if you eat foods or have drinks that are high in potassium this may lead to an increase of potassium in your body. Too much potassium can be harmful, therefore it is important to discuss your diet with your doctor or pharmacist.
Monitor your blood sugar levels carefully if you are a diabetic.
Amizide may change how well your diabetes is controlled. Your doses of diabetic medicines, including insulin, may need to change.
Things that would be helpful for your blood pressure
Some self-help measures suggested below may help your blood pressure.
Talk to your doctor or pharmacist about these measures and for more information.
- Alcohol: your doctor may advise you to limit your alcohol intake.
- Diet: eat a healthy diet which includes plenty of fresh vegetables, fruit, bread, cereals and fish. Also eat less fat and sugar.
- Exercise: regular exercise helps to reduce blood pressure. Try regular walking, swimming, cycling or games such as tennis and golf. Before starting any exercise, ask your doctor about the best kind of programme for you.
- Salt: your doctor may advise you to watch the amount of salt in your diet. To reduce your salt intake you should avoid using salt in cooking or at the table.
- Smoking: your doctor may advise you to stop smoking or at least cut down.
- Weight: your doctor may suggest losing some weight to help lower your blood pressure. Some people may need a dietician's help to lose weight.
Side effects
Tell your doctor or pharmacist as soon as possible if you do not feel well while you are taking Amizide.
Like all other medicines, Amizide may have unwanted side effects in some people. Sometimes they are serious, most of the time they are not. You may need medical treatment if you get some of the side effects.
Do not be alarmed by this list of possible side effects.
You may not experience any of them.
Ask your doctor or pharmacist to answer any questions you may have.
Tell your doctor if you notice any of the following and they worry you:
- dizziness or light-headedness
- drowsiness, lack of energy, weakness
- restlessness
- nausea, vomiting, change in appetite
- diarrhoea or constipation
- stomach discomfort or fullness
- passing wind
- bad taste in the mouth, visual disturbances, such as blurred vision or yellow vision
- passing less urine than normal.
Tell your doctor as soon as possible if you notice any of the following:
- very dry mouth or unusual thirst
- severe dizziness, spinning sensation
- fainting
- muscle pain or cramps, swollen or painful joints
- numbness or tingling in the hands or feet
- irregular or very fast heart beat
- chest pain
- mental confusion
- pain when passing urine, loss of control of your bladder or bowels
- yellowing of the skin or eyes (jaundice)
- signs of frequent infections such as fever, severe chills, sore throat or mouth ulcers
- bruising or bleeding more easily than normal, nose bleeds
- changes in heart beat
Tell your doctor immediately or go to Accident and Emergency at the nearest hospital if you notice any of the following:
- rash, itching or hives
- severe skin reactions which starts with painful red areas, then large blisters and ends with peeling of layers of skin. This is accompanied by fever and chills, aching muscles and generally feeling unwell.
- swelling of the face, lips, tongue or other parts of the body, shortness of breath, wheezing or trouble breathing
- fits or seizures
- vomiting blood or material that looks like coffee grounds
- bleeding from the back passage, black, sticky bowel motions (stools) or bloody diarrhoea.
These are serious side effects. You may need urgent medical attention or hospitalisation. These side effects are rare.
Other side effects not listed above may also occur in some patients. Tell your doctor if you notice anything that is making you feel unwell.
After taking Amizide
Storage
Keep Amizide where children cannot reach it.
A locked cupboard at least one-and-a-half metres above the ground is a good place to store medicines.
Keep your tablets in the bottle until it is time to take them.
If you take the tablets out of the bottle they may not keep well.
Keep your tablets in a cool dry place where the temperature stays below 30°C.
Do not store Amizide or any other medicine in the bathroom or near a sink.
Do not leave Amizide in the car or on window sills.
Heat and dampness can destroy some medicines.
Disposal
If your doctor tells you to stop taking Amizide, or your tablets have passed their expiry date, ask your pharmacist what to do with any that are left over.
Product description
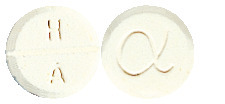
What it looks like
Amizide is a round, off-white, scored tablet marked H|A on one side and a on the reverse.
Each pack contains 50 tablets.
Ingredients
Amizide contains two active ingredients:
- hydrochlorothiazide 50 mg
- amiloride hydrochloride 5 mg.
The tablets also contain:
- lactose
- starch - wheat
- povidone
- sodium starch glycollate
- magnesium stearate.
Manufacturer
Amizide is made in Australia by:
Alphapharm Pty Limited
(ABN 93 002 359 739)
Level 1, 30 The Bond
30 - 34 Hickson Road
Millers Point NSW 2000
Phone: (02) 9298 3999
www.alphapharm.com.au
Australian registration numbers:
Amizide - Aust R 17702
This leaflet was prepared on
19 August 2013.
Amizide_cmi\aug13/00