What is in this leaflet
Read this leaflet carefully before taking your medicine.
This leaflet answers some common questions about aripiprazole. It does not contain all the available information.
It does not take the place of talking to your doctor or pharmacist.
All medicines have risks and benefits. Your doctor has weighed the risks of you using this medicine against the benefits they expect it will have for you.
If you have any concerns about taking this medicine, ask your doctor or pharmacist.
Keep this leaflet with your medicine. You may want to read it again.
What this medicine is used for
This medicine contains the active ingredient aripiprazole.
Aripiprazole belongs to a group of medicines called antipsychotic agents.
It is used to treat schizophrenia.
Ask your doctor if you have any questions about why this medicine has been prescribed for you.
This medicine is available only with a doctor's prescription.
There is no evidence that this medicine is addictive.
This medicine is not recommended for use in children under the age of 18, as safety and efficacy have not been established in this age group.
Before you take this medicine
When you must not take it
Do not take this medicine if you have an allergy to:
- aripiprazole
- any of the ingredients listed at the end of this leaflet
- Always check the ingredients to make sure you can use this medicine.
Some of the symptoms of an allergic reaction may include:
- shortness of breath
- wheezing or difficulty breathing
- swelling of the face, lips, tongue, throat or other parts of the body
- rash, itching or hives on the skin
Do not breastfeed if you are taking this medicine. Aripiprazole passes into breast milk. and there is a possibility that your baby may be affected.
Do not take this medicine after the expiry date printed on the pack or if the packaging is torn or shows signs of tampering. If it has expired or is damaged, return it to your pharmacist for disposal.
If you are not sure whether you should start taking this medicine, talk to your doctor.
Before you start to take it
Tell your doctor if you have allergies to any other medicines, foods, preservatives or dyes.
Tell your doctor if you have or have had any of the following medical conditions:
- a reaction to some medicines with a sudden increase in body temperature, sweating, fast heart beat, muscle stiffness and fluctuating blood pressure, which may lead to coma. This reaction is called neuroleptic malignant syndrome
- a reaction to some medicines with abnormal movements of the tongue, or other uncontrolled movements of the mouth, tongue, cheeks, eyes or jaw which may progress to the arms and legs. This reaction is called tardive dyskinesia
- low blood pressure
- problems with your heart or blood vessels
- epilepsy, seizures or fits
- problems with your oesophagus (food pipe), such as difficulty in swallowing
- high blood sugar or diabetes mellitus
- Alzheimer's disease or dementia
- alcohol or drug abuse, or dependence or a history of one of these
- venous thromboembolism or are at risk of venous thromboembolism
- have a history of or are at risk of sleep apnoea (a sleep disorder where your breathing is interrupted during sleep)
Tell your doctor if you are pregnant or plan to become pregnant. Aripiprazole is not recommended in pregnancy.
Do not take this medicine whilst pregnant until you and your doctor have discussed the risks and benefits involved.
Babies exposed to antipsychotics (including aripiprazole) during the third trimester of pregnancy are at risk or experiencing shaking, muscle stiffness, difficulty in feeding and/or withdrawal symptoms. These symptoms may resolve spontaneously or require medical treatment.
Tell your doctor or pharmacist if you are breast-feeding or plan to breast-feed.
It is recommended that you do not breast-feed while taking this medicine, as it may pass into breast milk and therefore there is a possibility that the breast-fed baby may be affected.
Tell your doctor if you have a history of excessive gambling.
Tell your doctor if you drink alcohol. Your doctor may advise you to avoid alcohol as it can magnify the side effects of this medicine.
This medicine may cause sleepiness, fall in blood pressure when standing up, dizziness and changes in your ability to move and balance, which may lead to falls. Caution should be taken.
If you have not told your doctor about any of the above, tell them before you start taking this medicine.
Taking other medicines
Tell your doctor or pharmacist if you are taking any other medicines, including any that you get without a prescription from your pharmacy, supermarket or health food shop.
Some medicines may interact with aripiprazole and affect how it works. These include:
- medicines used to treat brain disorders such as, anxiety, depression, mood swings, epilepsy or seizures, Parkinson’s disease or insomnia
- medicines for treating high blood pressure or heart problems (beta-blockers, calcium antagonists, ACE-inhibitors; anti-arrhythmics such as quinidine and amiodarone)
- alcohol or medicines which can make you sleepy
- fluoxetine, paroxetine or nefazodone, used for treating depression
- carbamazepine or phenytoin, used for epilepsy
- drugs for Parkinson’s Disease
- ketoconazole, fluconazole or itraconazole, medicines used for fungal infections
- medicines used to treat heart rhythm disturbances
- rifampicin, clarithromycin and erythromycin, used for treating bacterial infections
- efavirenz, nevirapine, ritonavir and indinavir, used for treating viral infections
- cyclosporin, used by patients who have had organ transplants, or who have rheumatoid arthritis or other rheumatic conditions
- cimetidine, used for treating stomach ulcers and other problems with the digestive tract
- St John’s Wort, a herbal preparation used for mood
- grapefruit and grapefruit juice, which may affect the blood levels of aripiprazole in the body
These medicines may be affected by aripiprazole or may affect how well it works. You may need different amounts of your medicines, or you may need to take different medicines.
Your doctor and pharmacist have more information on medicines to be careful with or avoid while taking this medicine.
How to take this medicine
Follow carefully all directions given to you by your doctor. Their instructions may be different to the information in this leaflet.
If you do not understand the directions, ask your doctor or pharmacist for help.
How much to take
Your doctor will tell you how much of this medicine you should take. This will depend on your condition and whether you are taking any other medicines.
How to take it
Swallow the tablets whole with a glass of water.
It does not matter if you take this medicine before or after food but try to be consistent each dose.
When to take it
Take this medicine at the same time each day. Taking it at the same time each day will have the best effect and will also help you remember when to take it.
The tablets are usually taken once a day, unless your doctor gives you different instructions.
It does not matter if you take it before, with or after food.
How long to take it for
Continue taking your medicine for as long as your doctor tells you, unless you have any problems. In that case, check with your doctor.
Aripiprazole tablets may control schizophrenia, but they do not cure it. Therefore, you must take this medicine every day. Stopping aripiprazole suddenly can mean your schizophrenia becomes uncontrolled. Improvements in symptoms may take some time to occur. Even if you feel better do not stop taking this medicine unless your doctor tells you to.
Make sure you have enough of this medicine to last over weekends and holidays.
If you forget to take it
If it is almost time to take your next dose, skip the missed dose and take your next dose at the usual time.
Otherwise, take it as soon as you remember and then go back to taking your medicine as you would normally.
Do not take a double dose to make up for missed doses. This may increase the chance of you experiencing side effects.
If you are not sure what to do, ask your doctor or pharmacist.
If you have trouble remembering to take your medicine, ask your pharmacist for some hints to help you remember.
If you take too much (overdose)
If you think that you or anyone else may have taken too much of this medicine, immediately telephone your doctor or the Poisons Information Centre (Tel: 13 11 26 in Australia) for advice. Alternatively, go to the Accident and Emergency department at your nearest hospital.
Do this even if there are no signs of discomfort or poisoning. You may need urgent medical attention.
While you are taking this medicine
Things you must do
If you are about to be started on any new medicine, remind your doctor, dentist and pharmacist that you are taking this medicine.
Tell any other doctors, dentists, and pharmacists who treat you that you are taking this medicine.
If you are going to have any kind of surgery that needs a general anaesthetic, tell the surgeon, dentist or anaesthetist that you are taking this medicine. It may affect other medicines used during surgery.
If you become pregnant or start to breastfeed while taking this medicine, tell your doctor immediately.
If you are about to have any blood tests, tell your doctor that you are taking this medicine. It may interfere with the results of some tests.
Keep all your doctor's appointments so that your progress can be checked. Your doctor may do some tests from time to time to make sure the medicine is working and to prevent unwanted side effects.
Things you must not do
Do not give this medicine to anyone else, even if their symptoms seem similar or they have the same condition as you.
Do not take your medicine to treat any other condition unless your doctor tells you to.
Do no stop taking your medicine, or change the dosage, even if you are feeling better, without first checking with your doctor.
If you stop taking this medicine suddenly your condition may worsen.
Do not take more of this medicine and do not take it more often than your doctor has ordered.
Things to be careful of
Make sure that you know how you react to this medicine before you drive a car, operate machinery or do anything else that could be dangerous if you are dizzy or light headed or not alert. Aripiprazole may cause some people to become drowsy or less alert than they are normally or cause lightheadedness, dizziness or tiredness. If this occurs do not undertake the activity.
Be careful when drinking alcohol while you are being treated with this medicine. Your doctor may suggest you avoid alcohol while taking aripiprazole.
If this medicine makes you feel light- headed, dizzy or faint, be careful when getting up from a sitting or lying position.
Getting up slowly may help.
Make sure you keep cool in hot weather and keep warm in cool weather. Aripiprazole may affect the way your body reacts to temperature changes. It may prevent sweating, even during heatwaves. You may feel dizzy or faint if you are too hot.
To stay cool in hot weather, try to do the following:
- wear light clothing
- spend time in air-conditioned environments (or keep windows open and use electric fans)
- drink plenty of water
- take cool baths or showers and avoid hot baths and saunas
- try to restrict exercise or heavy work to cool parts of the day
Side effects
Tell your doctor or pharmacist as soon as possible if you do not feel well while you are taking aripiprazole or if you have any questions or concerns.
Like other medicines, this medicine may have some unwanted side effects. These are likely to vary from patient to patient. Sometimes they are serious but most of the time they are not. This medicine is generally well-tolerated and the side effects are often hard to distinguish from disease symptoms. It is important that you tell your doctor as soon as possible about any unwanted effects.
Do not be alarmed by the following lists of side effects. You may not experience any of them.
Ask your doctor or pharmacist to answer any questions you may have.
Tell your doctor if you notice any of the following and they worry you:
- headache
- chest pain
- indigestion
- nausea
- vomiting
- insomnia
- constipation
- light-headedness
- agitation
- anxiety
- inability to sit or stand still; restless movement of the arms and legs such as tapping, marching in places, rocking, crossing and uncrossing the legs
- drowsiness
These are the more common side effects of this medicine.
Tell your doctor as soon as possible if you notice any of the following:
- feeling dizzy especially when getting up from a lying or sitting position
- altered or increased sexual interest
These side effects are uncommon.
- high blood sugar (excessive thirst, hunger and weakness) or the onset or worsening of diabetes
This side effect is rare.
- weight gain
- weight loss
- loss of appetite
- excessive sweating
- drowsiness
- high blood pressure
- chest pain
- frequent infections such as fever, severe chills, sore throat or mouth ulcers
- bleeding or bruising more easily than normal
- speech disorder
- urinary incontinence
- difficulty swallowing.
- hiccups
These side effects are very rare.
The above list includes serious side effects that may require medical attention.
Tell your doctor if you have obsessive (recurring) thoughts or behaviours, or trouble controlling impulsive urges or while taking this medicine. Obsessive compulsive behaviours (feeling the need to check things repeatedly or having certain thoughts repeatedly), gambling urges, sexual urges, compulsive spending, binge or compulsive eating and other urges have occurred in some patients
If any of the following happen, tell your doctor immediately or go to Accident and Emergency at your nearest hospital:
- seizure, fits or convulsions
- fainting
- abnormal movements of the tongue, or other uncontrolled movements of the tongue, mouth, cheeks, eyes or jaw which may progress to the arms and legs
- sudden increase in body temperature, sweating, fast heart beat, muscle stiffness, high blood pressure and convulsions
- rash
- muscle pain, muscle weakness or muscle stiffness
- inflammation of the pancreas, severe upper stomach pain often with nausea and vomiting
- disorder of body temperature regulation resulting in low body temperature or high body temperature
- painful irreversible erection
- difficulty in passing urine
- yellowing of the skin and/or eyes (also called jaundice), with or without nausea, vomiting, loss of appetite, feeling generally unwell, fever, itching and dark coloured urine
- serious lung infection with fever, chills, shortness of breath, cough, chest pain and blood streaked phlegm
- thoughts or talk about death or suicide; thoughts or talk about self-harm or doing harm to others; any recent attempts at self-harm; an increase in aggressive behaviour, irritability or agitation. If you or someone you know is showing these signs, contact your doctor or a mental health advisor right away or go to the nearest hospital for treatment
- symptoms of an allergic reaction including shortness of breath, wheezing, difficulty breathing; swelling of the face, lips, tongue or throat; rash, itching, hives on the skin; fainting, and/or hayfever
These are very serious side effects. You may need urgent medical attention or hospitalisation.
All of these side effects are very rare.
Other side effects not listed above may occur in some patients.
Some of these side effects can only be found when your doctor does tests from time to time to check your progress.
While taking aripiprazole, some elderly patients with dementia have suffered serious side effects such as a "mini" stroke, stroke, pneumonia or heart problems. These serious side effects can be life threatening.
Tell your doctor or pharmacist if you notice anything that is making you feel unwell.
Storage and disposal
Storage
Keep your medicine in its original packaging until it is time to take it. If you take your medicine out of its original packaging it may not keep well.
Keep your medicine in a cool dry place where the temperature will stay below 25°C.
Do not store your medicine, or any other medicine, in the bathroom or near a sink. Do not leave it on a window sill or in the car. Heat and dampness can destroy some medicines.
Keep this medicine where children cannot reach it. A locked cupboard at least one-and-a-half metres above the ground is a good place to store medicines.
Disposal
If your doctor tells you to stop taking this medicine or the expiry date has passed, ask your pharmacist what to do with any medicine that is left over.
Product description
What APO-Aripiprazole Tablets look like
2 mg tablets:
Green, rectangular, slightly biconvex tablets engraved “2” on one side, “A” on the other side. AUST R 152903. AUST R 152917.
5 mg tablets:
Blue, rectangular, slightly biconvex tablets engraved “5” on one side, “A” on the other side. AUST R 152904. AUST R 152911.
10 mg tablets:
Pink, rectangular, slightly biconvex tablets, engraved “10” on one side, “A” on the other side. AUST R 152908. AUST R 152920.
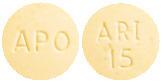
15 mg tablets:
Yellow, round, slightly biconvex tablets, engraved “ARI” over “15” on one side, “APO” on the other side. AUST R 152924. AUST R 152898.
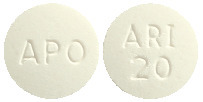
20 mg tablets:
White to off-white, round, slightly biconvex tablets, engraved “ARI” over “20” on one side, “APO” on the other side. AUST R 152899. AUST R 152932.
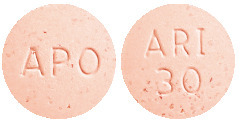
30 mg tablets:
Pink, round, slightly biconvex tablets, engraved “ARI” over “30” on one side, “APO” on the other side. AUST R 152905. AUST R 152929.
Available in blister packs of 30 tablets, or bottles of 30 or 100 tablets.
* Not all strengths, pack types and/or pack sizes may be available.
Ingredients
Each tablet contains 2 mg, 5 mg, 10 mg, 15 mg, 20 mg or 30 mg of aripiprazole as the active ingredient. It also contains the following inactive ingredients:
- Microcrystalline Cellulose
- Tartaric Acid
- Magnesium Stearate
- Croscarmellose Sodium
- Indigo Carmine aluminium lake (2 mg and 5 mg strength only)
- Iron Oxide Yellow (2 mg and 15 mg strength only)
- Iron Oxide Red (10 mg and 30 mg strength only)
This medicine is gluten-free, lactose-free, sucrose-free, tartrazine-free and free of other azo dyes.
Sponsor
Apotex Pty Ltd
16 Giffnock Avenue
Macquarie Park NSW 2113
Australia
Tel: (02) 8877 8333
Web: www1.apotex.com/au
APO and APOTEX are registered trademarks of Apotex Inc.
This leaflet was last updated in October 2021.
Published by MIMS December 2021




 An examination of population subgroups did not reveal any clear evidence of differential adverse reaction incidence on the basis of age, gender or race.
An examination of population subgroups did not reveal any clear evidence of differential adverse reaction incidence on the basis of age, gender or race.

 A 52-week, haloperidol-controlled, long-term, maintenance trial (n = 1294) was performed in patients with acute relapse of chronic schizophrenia. The trial involved the administration of aripiprazole 30 mg/day and haloperidol 10 mg/day, with a one time option to decrease aripiprazole to 20 mg/day and haloperidol to 7 mg/day, aripiprazole was at least comparable to haloperidol in time-to-failure to maintain response in responders. Based on patients who responded at any time during the 52-week study (610/853, 72% in the aripiprazole group and 298/430, 69% in the haloperidol group), there was a 12% lower risk of subsequent failure with aripiprazole relative to haloperidol (relative risk: 0.881, 95% CI: 0.645 - 1.204). In all randomised patients, aripiprazole was comparable to haloperidol in time-to-failure to maintain response. Patients in the aripiprazole group had a 14% lower risk of failure compared with the haloperidol group (relative risk: 0.858, 95% CI: 0.721, 1.021). Aripiprazole was statistically superior to haloperidol in the analysis of the proportion of patients on treatment and in response at Weeks 8, 26, and 52 (prespecified key time points). At Week 52, 40% of aripiprazole patients were still on-study and in response compared to 27% of haloperidol patients (p < 0.001). Aripiprazole-treated patients had a statistically significant lower risk (31%) of discontinuations due to lack of efficacy or adverse event relative to haloperidol treated patients (relative risk 0.692; 95% CI: 0.573 - 0.837). In terms of change from baseline PANSS total scores, PANSS positive subscores, CGI-severity or improvement scores, there were no significant differences between aripiprazole and haloperidol groups. However, aripiprazole treatment resulted in a significantly greater improvement in the PANSS negative subscores at weeks 26 and 52 and the MADRS total score at Weeks 8, 26, and 52. [Mean change PANSS negative subscale score (week 26: p = 0.029; 95% CI: -1.52, -0.08) (week 52: p = 0.011; 95% CI: -1.73, -0.23). Mean change MADRS total score (week 8: p = 0.027; 95% CI: -1.74, -0.11) (week 26: p = 0.22; 95% CI: -1.95, -0.15) (week 52: p = 0.031; 95% CI: -1.97, -0.09).]
A 52-week, haloperidol-controlled, long-term, maintenance trial (n = 1294) was performed in patients with acute relapse of chronic schizophrenia. The trial involved the administration of aripiprazole 30 mg/day and haloperidol 10 mg/day, with a one time option to decrease aripiprazole to 20 mg/day and haloperidol to 7 mg/day, aripiprazole was at least comparable to haloperidol in time-to-failure to maintain response in responders. Based on patients who responded at any time during the 52-week study (610/853, 72% in the aripiprazole group and 298/430, 69% in the haloperidol group), there was a 12% lower risk of subsequent failure with aripiprazole relative to haloperidol (relative risk: 0.881, 95% CI: 0.645 - 1.204). In all randomised patients, aripiprazole was comparable to haloperidol in time-to-failure to maintain response. Patients in the aripiprazole group had a 14% lower risk of failure compared with the haloperidol group (relative risk: 0.858, 95% CI: 0.721, 1.021). Aripiprazole was statistically superior to haloperidol in the analysis of the proportion of patients on treatment and in response at Weeks 8, 26, and 52 (prespecified key time points). At Week 52, 40% of aripiprazole patients were still on-study and in response compared to 27% of haloperidol patients (p < 0.001). Aripiprazole-treated patients had a statistically significant lower risk (31%) of discontinuations due to lack of efficacy or adverse event relative to haloperidol treated patients (relative risk 0.692; 95% CI: 0.573 - 0.837). In terms of change from baseline PANSS total scores, PANSS positive subscores, CGI-severity or improvement scores, there were no significant differences between aripiprazole and haloperidol groups. However, aripiprazole treatment resulted in a significantly greater improvement in the PANSS negative subscores at weeks 26 and 52 and the MADRS total score at Weeks 8, 26, and 52. [Mean change PANSS negative subscale score (week 26: p = 0.029; 95% CI: -1.52, -0.08) (week 52: p = 0.011; 95% CI: -1.73, -0.23). Mean change MADRS total score (week 8: p = 0.027; 95% CI: -1.74, -0.11) (week 26: p = 0.22; 95% CI: -1.95, -0.15) (week 52: p = 0.031; 95% CI: -1.97, -0.09).] Chemical Name: 7-[4-[4-(2,3-dichlorophenyl)-1-piperazinyl]butoxy]-3,4-dihydro-2(1H)-quinolinone.
Chemical Name: 7-[4-[4-(2,3-dichlorophenyl)-1-piperazinyl]butoxy]-3,4-dihydro-2(1H)-quinolinone.