What is in this leaflet
Read this leaflet carefully before taking your medicine. This leaflet answers some common questions about candesartan. It does not contain all the available information.
It does not take the place of talking to your doctor or pharmacist.
The information in this leaflet was last updated on the date listed on the last page. More recent information on this medicine may be available.
Ask your doctor or pharmacist:
- if there is anything you do not understand in this leaflet,
- if you are worried about taking your medicine, or
- to obtain the most up-to-date information.
You can also download the most up to date leaflet from www.apotex.com.au.
All medicines have risks and benefits. Your doctor has weighed the risks of you using this medicine against the benefits they expect it will have for you.
Pharmaceutical companies cannot give you medical advice or an individual diagnosis.
Keep this leaflet with your medicine. You may want to read it again.
What this medicine is used for
The name of your medicine is APO-Candesartan. It contains the active ingredient candesartan cilexetil.
It is used to treat:
- high blood pressure, also called hypertension.
- heart failure - increase survival, reduce hospitalisation and improve symptoms. It is used in combination with other medicines to treat your condition.
Ask your doctor if you have any questions about why this medicine has been prescribed for you.
Your doctor may have prescribed this medicine for another reason.
This medicine is available only with a doctor's prescription.
There is no evidence that this medicine is addictive.
How it works
Candesartan is a type of medicine called an angiotensin II receptor inhibitor (or antagonist).
Hypertension:
All people have blood pressure. This pressure helps to push blood all around your body. Your blood pressure changes during the day, depending on how busy you are or how you are feeling.
You have hypertension (high blood pressure) when your blood pressure stays higher than is needed, even when you are calm and relaxed.
Regular blood pressure checks are the only way of knowing that you have hypertension. There are usually no symptoms of hypertension and you may feel fine. If hypertension is not treated, serious health problems such as stroke or heart attack and heart or kidney failure may occur.
Candesartan lowers blood pressure by dilating (expanding) small blood vessels from the heart, letting the blood be pumped around the body more easily.
Heart Failure:
Heart failure means that the heart muscle cannot pump blood strongly enough to supply all the blood needed throughout the body. Heart failure is not the same as heart attack and does not mean that the heart stops working.
Heart failure may start off with no symptoms, but as the condition progresses, patients may feel short of breath or may get tired easily after light physical activity such as walking. Some patients may wake up short of breath at night. Fluid may collect in different parts of the body, often first noticed as swollen ankles and feet.
Candesartan helps to treat heart failure and may improve your symptoms.
One of the ways candesartan helps heart failure is that it widens the blood vessels, so that the heart does not have to pump as hard to move the blood around the body. This also means that when you place extra demands on your heart, such as during exercise, the heart may cope better so you may not get short of breath as easily.
When used to treat heart failure, candesartan is almost always used with other medicines called diuretics or fluid tablets. These medicines help the kidney to get rid of excess fluid from the body.
Use in children
There is no information about its use in children, so candesartan is not recommended for children
Before you use this medicine
When you must not use it
Do not use this medicine if you have an allergy to:
- candesartan cilexetil or any of the ingredients listed at the end of this leaflet.
- angiotensin II receptor inhibitor (or antagonist), e.g. telmisartan, irbesartan, olmesartan etc.
Symptoms of an allergic reaction may include: shortness of breath, wheezing or difficulty breathing; swelling of the face, lips, tongue, throat or other parts of the body; rash, itching or hives on the skin.
If you think you are having an allergic reaction, contact your doctor immediately or go to the Accident and Emergency department at the nearest hospital. - Do not use candesartan if you are also taking aliskiren-containing medications and have kidney problems or diabetes.
- Do not use candesartan if you have severe hepatic impairment (live disease) and/or cholestasis (a condition where bile does not flow from the liver)
- Do not use candesartan if you are pregnant or planning to become pregnant
It may affect your baby if you take it during pregnancy. - Do not breast-feed if you are taking candesartan.
It is not known if candesartan passes into breast milk. - Do not use this medicine if the expiry date (EXP) printed on the pack has passed.
- Do not use this medicine if the packaging is torn, shows signs of tampering or it does not look quite right.
Before you start to take it
Before you start taking this medicine, tell your doctor if:
- You have allergies to:
- any other medicines
- any other substances, such as foods, preservatives or dyes.
- You have or have had any medical conditions, especially the following:
- kidney problems
- liver problems
- heart or blood vessel problems
- recent excessive vomiting or diarrhoea
- a condition called primary hyperaldosteronism
You may have to take a lower dose of candesartan if you have these conditions.
- You are planning to have surgery or an anaesthetic.
If you have not told your doctor about any of the above, tell them before you use this medicine.
Taking other medicines
Tell your doctor if you are taking any other medicines, including any that you buy at the chemist, supermarket or health food shop.
Some medicines and candesartan may interfere with each other. These include:
- Medicines containing potassium, including salt substitutes
- Diuretics (fluid tablets)
- Lithium, a medicine used to treat mood swings and some types of depression
- Non-steroidal anti-inflammatory drugs (NSAIDs), medicines used to relieve pain, swelling and other symptoms of inflammation, including arthritis.
- Angiotensin converting enzyme (ACE) inhibitors e.g. perindopril, ramipril and captopril.
- Mineralocorticoid receptor antagonists (MRSs), such as spironolactone and eplerenone, medicines used to treat heart failure.
These medicines may be affected by candesartan or may affect the way candesartan works. You may need different amounts of your medicines, or may need to take different medicines.
Your doctor and pharmacist have more information on medicines to be careful with or avoid while taking this medicine.
It may be necessary to have regular blood tests done if you take any of these medicines.
How to take this medicine
Follow carefully all directions given to you by your doctor. Their instructions may be different to the information in this leaflet.
If you are not sure how to take this medicine, ask your doctor or pharmacist for help.
How to take it
Your doctor or pharmacist will tell you how much of this medicine you should take. This will depend on your condition and whether you are taking any other medicines.
Do not stop taking your medicine or change your dosage without first checking with your doctor.
Take candesartan once a day, at about the same time each day. Taking candesartan at the same time each day will help you remember when to take it.
It does not matter whether you take candesartan with food or on an empty stomach.
How long to take it
Continue taking this medicine for as long as your doctor tells you.
This medicine controls your condition but does not cure it. It is important to keep taking your medicine even if you feel well.
If you forget to take it
If it is almost time to take your next dose, skip the missed dose and take your next dose at the usual time.
Otherwise take it as soon as you remember and then go back to taking your medicine as you would normally.
Do not take a double dose to make up for missed doses. If you are not sure what to do, ask your doctor or pharmacist.
If you have trouble remembering when to take your medicine, ask your pharmacist for some hints.
If you take too much (overdose)
If you think that you or anyone else may have taken too much of this medicine, immediately telephone your doctor or the Poisons Information Centre (Tel: 13 11 26 in Australia) for advice. Alternatively go to the Accident and Emergency Department at your nearest hospital.
Do this even if there are no signs of discomfort or poisoning. You may need urgent medical attention.
If you take too much candesartan you may get a headache and feel sick (nausea), dizzy and very tired.
While you are using this medicine
Things you must do
- Take candesartan exactly as your doctor has told you to. Your blood pressure will not be well controlled if you do not.
- If you become pregnant while you are using this medicine, tell your doctor.
- Tell all doctors, dentists and pharmacists who are treating you that you are using this medicine.
- If you are about to be started on any new medicine, tell your doctor or pharmacist that you are using this medicine.
- If you are going to have surgery, inform your doctor and tell the surgeon or anaesthetist that you are using this medicine.
Things you must not do
Do not:
- Give this medicine to anyone else, even if their symptoms seem similar to yours
- Take your medicine to treat any other condition unless your doctor or pharmacist tells you to
- Stop taking your medicine, or change the dosage, without first checking with your doctor.
Things to be careful of
Move slowly when getting out of bed or standing up if you feel faint, dizzy or light-headed.
Be careful driving or operating machinery until you know how candesartan affects you. You may feel dizzy when you start taking candesartan.
If you are taking candesartan for high blood pressure, drink plenty of water during exercise and hot weather, especially if you sweat a lot. If you do not drink enough water while taking candesartan, you may faint or feel light-headed or sick. This is because your body doesn't have enough fluid and your blood pressure is low. If you continue to feel unwell, tell your doctor.
If you are taking candesartan for heart failure, restricted fluid intake is generally recommended. Speak with your doctor about how much water you should drink.
Please talk to your doctor or pharmacist about any concerns you may have about the above.
Possible side effects
Tell your doctor or pharmacist as soon as possible if you do not feel well while you are using this medicine.
Your doctor will decide whether any change in your treatment is needed.
All medicines can have side effects. Sometimes they are serious, most of the time they are not. You may need medical treatment if you get some of the side effects.
If you are over 65 years of age, you may have an increased chance of getting side effects.
Candesartan helps most people, but it may have side effects in a few people.
Ask your doctor or pharmacist to answer any questions you may have.
Tell your doctor if you notice any of the following and they worry you:
- headache
- chest or throat infection
- flu-like symptoms
- feeling sick (nausea, vomiting)
- back pain
- dizziness
These are all mild side effects of candesartan.
The following side effects have been reported very rarely by patients taking candesartan: palpitations, agitation, anxiety, depression, trouble sleeping (insomnia), drowsiness (somnolence), nervousness, nightmare and sleep disorder. It is not known if these side effects are caused by candesartan.
Tell your doctor as soon as possible if you notice any of the following:
- aching muscles, tenderness or weakness in the muscle
The above list includes serious side effects that may require medical attention. These side effects are rare.
If any of the following happen, tell your doctor immediately or go to Accident and Emergency at your nearest hospital.
- swelling of the face, lips, tongue or throat which may cause difficulty in swallowing or breathing
- swelling of the hands, feet or ankles
- harsh sounds when breathing
- signs of frequent infections such as fever, severe chills, sore throat or mouth ulcers
- jaundice (yellowing of the skin and/or eyes)
- unusual skin reactions (severe and sudden onset of rash), itchiness, hives (itchy swellings on the skin)
- easy bruising or bleeding more easily than normal
- extreme fatigue, tiredness, weakness
- worsening kidney function, including passing little or no urine, drowsiness, nausea, vomiting, breathlessness, loss of appetite and weakness (especially in patients with existing kidney problems or heart failure)
- changes in your potassium, sodium and red or white blood cell levels may occur. Such changes are usually detected by a blood test
- symptoms that may indicate high potassium levels in the blood include nausea, diarrhoea, muscle weakness and changes in heart rhythm
The above list includes very serious side effects. You may need urgent medical attention or hospitalisation.
These side effects are very rare.
Do not be alarmed by this list of possible side effects. You may not experience any of them.
Other side effects not listed above may occur in some people. Tell your doctor if you notice any other side effects.
Storage and disposal
Storage
Keep your tablets in the blister pack until it is time to take them. If you take candesartan out of the blister pack it will not keep well.
Keep your tablets in a cool dry place where the temperature will stay below 25°C. Do not store your medicine, or any other medicine, in the bathroom or near a sink. Do not leave it on a window sill or in the car. Heat and dampness can destroy some medicines.
Keep this medicine where children cannot reach it. A locked cupboard at least one-and-a-half metres above the ground is a good place to store medicines.
Disposal
If your doctor or pharmacist tells you to stop taking this medicine or they have passed their expiry date, your pharmacist can dispose of the remaining medicine safely.
Product description
What APO-Candesartan looks like
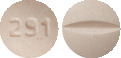
APO-Candesartan 4 mg tablets: Light pink, round, biconvex uncoated mottled tablet with '291' on one side and a break line on the other side
APO-Candesartan 8mg tablets: Light pink, round, biconvex, uncoated mottled tablet with '292' on one side and a break line on the other side
APO-Candesartan 16 mg tablets: Light pink, round, biconvex uncoated mottled tablet with 'L293' on one side and a break line on the other side
APO-Candesartan 32 mg tablets: Light pink, round, biconvex uncoated mottled tablet with 'L294' on one side and a break line on the other side.
Ingredients
Each tablet contains 4mg or 8mg or 16mg or 32mg of the active ingredient candesartan cilexetil.
It also contains the following inactive ingredients:
- lactose
- maize starch
- hyprolose
- carmellose calcium
- magnesium stearate
- Pigment Blend PB-24880 Pink (iron oxide red and lactose).
- macrogol 8000
This medicine is gluten-free, tartrazine-free and free of other azo dyes and contains sugar as lactose.
APO-Candesartan is available in:
Blister packs of 7, 28 and 30 tablets.
Not all strengths, pack types and/or pack sizes may be available
Australian Registration Numbers
APO-Candesartan 4 mg blister pack: AUST R 210529
APO-Candesartan 8 mg blister pack: AUST R 210530
APO-Candesartan 16 mg blister pack: AUST R 210531
APO-Candesartan 32 mg blister pack: AUST R 210532
Sponsor
Arrotex Pharmaceutical Pty Ltd
15-17 Chapel Street
Cremorne VIC 3121
Australia
www.arrotex.com.au
This leaflet was prepared in August 2023.
Published by MIMS November 2023





 Significant reduction in urinary albumin/ creatinine ratio (UACR), in both monotherapy treatment groups was observed, although no significant difference between treatment groups was seen. Combination therapy following monotherapy for 12 weeks showed significantly greater reduction in UACR (mean reduction of 50%) than candesartan cilexetil 16 mg monotherapy (mean reduction in UACR 24%) and numerically greater reduction than lisinopril 20 mg monotherapy (mean reduction in UACR 39%).
Significant reduction in urinary albumin/ creatinine ratio (UACR), in both monotherapy treatment groups was observed, although no significant difference between treatment groups was seen. Combination therapy following monotherapy for 12 weeks showed significantly greater reduction in UACR (mean reduction of 50%) than candesartan cilexetil 16 mg monotherapy (mean reduction in UACR 24%) and numerically greater reduction than lisinopril 20 mg monotherapy (mean reduction in UACR 39%).

 All cause mortality was also assessed in pooled populations, CHARM-Alternative and CHARM-Added (HR 0.88, 95% CI 0.79-0.98, p = 0.018) and all three studies (HR 0.91, 95% CI 0.83-1.00, p = 0.055). This corresponds to a relative risk reduction of 12% and 9% respectively and an absolute risk reduction of 2.9 and 1.6% respectively.
All cause mortality was also assessed in pooled populations, CHARM-Alternative and CHARM-Added (HR 0.88, 95% CI 0.79-0.98, p = 0.018) and all three studies (HR 0.91, 95% CI 0.83-1.00, p = 0.055). This corresponds to a relative risk reduction of 12% and 9% respectively and an absolute risk reduction of 2.9 and 1.6% respectively.
 Three polymorphic forms have been identified; crystal form I, crystal form II and an amorphous form. Crystalline form I is used in APO-Candesartan.
Three polymorphic forms have been identified; crystal form I, crystal form II and an amorphous form. Crystalline form I is used in APO-Candesartan. Chemical Name: (±)-1-(cyclohexyloxycarbonyl-oxy) ethyl 2-ethoxy-1-[[2'-(1H-tetrazol-5-yl) biphenyl-4-yl] methyl]-1H-benzimadozole-7-carboxylate.
Chemical Name: (±)-1-(cyclohexyloxycarbonyl-oxy) ethyl 2-ethoxy-1-[[2'-(1H-tetrazol-5-yl) biphenyl-4-yl] methyl]-1H-benzimadozole-7-carboxylate.