What is in this leaflet
This leaflet answers some common questions about this medicine. It does not contain all the available information. It does not take the place of talking to your doctor or pharmacist.
All medicines have risks and benefits. Your doctor has weighed the risks of you taking this medicine against the benefits they expect it will have for you.
If you have any concerns about taking this medicine, ask your doctor or pharmacist.
Keep this leaflet with the medicine. You may need to read it again.
What this medicine is used for
The name of your medicine is APO-Frusemide. It contains the active ingredient furosemide (frusemide).
Furosemide (frusemide) belongs to a family of drugs called diuretics. A diuretic helps reduce the amount of excess fluid in the body by increasing the amount of urine produced.
Furosemide (frusemide) is used to treat swelling of the ankles, feet, legs or even the brain or lungs. This swelling is called oedema and can occur in some heart, lung, liver or kidney conditions.
Furosemide (frusemide) may be used in some patients with more serious kidney problems who may have some fluid retention.
Furosemide (frusemide) may also be used to lower high blood pressure (which is also called hypertension).
Everyone has blood pressure. This pressure helps move your blood around your body. Your blood pressure may be different at different times of the day, depending on how busy or worried you are. You have hypertension (high blood pressure) when your blood pressure stays higher than is needed, even when you are calm and relaxed.
If high blood pressure is not treated it can lead to serious health problems, including stroke, heart disease and kidney failure.
Furosemide (frusemide) may be taken alone or in combination with other medicines to treat your condition.
Your doctor may have prescribed furosemide (frusemide) for another purpose.
Ask your doctor if you have any questions about why it has been prescribed for you.
This medicine is not addictive.
This medicine is only available with a doctor's prescription.
Before you take this medicine
When you must not take it
Do not take this medicine if you have an allergy to:
- furosemide (frusemide)
- medicines called sulfonamides (e.g. some types of antibiotics which are also referred to as 'sulfur antibiotics') or sulfonylureas which are medicines used to treat diabetes
- any of the ingredients listed at the end of this leaflet.
Some of the symptoms of an allergic reaction may include:
- shortness of breath
- wheezing or difficulty breathing
- swelling of the face, lips, tongue or other parts of the body
- rash, itching or hives on the skin
Do not take this medicine if you have any of the following medical conditions:
- certain kidney and liver problems
- no production or no passing of urine
- low blood pressure (hypotension)
- low sodium levels in your blood
- low potassium levels in your blood
- dehydration
- jaundice or history of jaundice in newborns or infants
- hepatic coma or precoma
Do not take this medicine if you are pregnant. Furosemide (frusemide) should not be used during pregnancy as it may affect your developing baby.
Do not breastfeed if you are taking this medicine. Furosemide (frusemide) passes into breast milk and may affect your baby.
Do not take this medicine after the expiry date printed on the pack or if the packaging is torn or shows signs of tampering. If it has expired or is damaged, return it to your pharmacist for disposal.
If you are not sure whether you should start taking this medicine, talk to your doctor.
Before you start to take it
Tell your doctor if you have allergies to any other medicines, foods, preservatives or dyes.
Tell your doctor if you have or have had any of the following medical conditions:
- liver problems
- kidney problems
- heart problems
- high cholesterol levels
- asthma
- diabetes
- gout, a disease with painful, swollen joints
- passing less urine than is normal or difficulty passing urine
- prostate problems
- Systemic Lupus Erythematosus (SLE), a disease affecting the skin, joints and kidneys.
Tell your doctor if you are pregnant or plan to become pregnant or are breastfeeding. Your doctor can discuss with you the risks and benefits involved.
Tell your doctor if you are on a salt restricted diet.
If you have not told your doctor about any of the above, tell them before you start taking this medicine.
Taking other medicines
Tell your doctor or pharmacist if you are taking any other medicines, including any that you get without a prescription from your pharmacy, supermarket or health food shop.
Some medicines and furosemide (frusemide) may interfere with each other. These include:
- certain other fluid tablets or diuretic medicines such as ethacrynic acid
- medicines used to treat high blood pressure and some other heart conditions, especially ACE inhibitors or angiotensin receptor antagonists
- digoxin and other medicines used to treat heart failure
- non-steroidal anti-inflammatory drugs (NSAIDs) and aspirin, medicines used to relieve pain, swelling and other symptoms of inflammation, including arthritis
- medicines used to relax muscles such as tubocurarine and succinylcholine
- lithium, a medicine used to treat mood swings and some types of depression
- medicines used in emergency situations such as adrenaline and noradrenaline
- cisplatin, a medicine used to treat cancer
- theophylline, a medicine used to treat asthma
- certain antibiotics, especially cephalosporins and aminoglycosides
- amphotericin, a medicine used to treat fungal infections
- barbiturates, medicine used to treat epilepsy, to produce calmness or to help you sleep
- narcotic/strong pain killers such as codeine and morphine
- medicines used to treat diabetes such as insulin
- sucralfate, a medicine used to treat stomach ulcers
- anticonvulsant medicines such as chloral hydrate or phenytoin
- corticosteroids such as cortisone, prednisone or dexamethasone
- medicines used during scans to see the images of your body
- methotrexate and cyclosporine, medicines that suppress the immune system
- carbenoxolone, used to treat ulcers of the mouth or oesophagus
- medicines used to treat thyroid conditions
- risperidone, used to treat mood disorders
- large amounts of laxatives, medicines for constipation
These medicines may be affected by furosemide (frusemide) or may affect how well it works. You may need different amounts of your medicines, or you may need to take different medicines.
You should not eat large amounts of liquorice when you are taking furosemide (frusemide).
Your doctor and pharmacist have more information on medicines to be careful with or avoid while taking this medicine.
How to take this medicine
Follow the directions given to you by your doctor carefully. They may differ from the information contained in this leaflet.
If you do not understand the instructions on the label, ask your doctor or pharmacist for help.
How much to take
Your doctor will tell you how much of this medicine you should take. This will depend on your condition and whether you are taking any other medicines.
Oedema
Adults: 20 to 80 mg as a single dose. The dose may be increased in exceptional cases up to 400 mg per day.
Children: 2 mg per kg bodyweight per day. The dose may be increased by 1-2mg per kg and should not exceed 6mg per kg bodyweight.
Hypertension
Adults: The recommended dosage is 40 mg twice daily. The dose may be adjusted according to the patient's response.
How to take it
Swallow furosemide (frusemide) tablets with a glass of water.
When to take it
Furosemide (frusemide) tablets are usually taken once or twice a day.
Take furosemide (frusemide) tablets on an empty stomach. For example, one hour before food or two hours after food. Food can interfere with the absorption of furosemide (frusemide) tablets.
Take furosemide (frusemide) tablets at about the same time each day unless your doctor tells you otherwise. Taking it at the same time each day will have the best effect. It will also help you remember when to take it.
If you are taking a single dose a day, take it in the morning, for example before breakfast.
If you are taking more than one dose a day, take the last dose no later than 2 pm, unless your doctor tells you otherwise. Furosemide (frusemide) may increase the amount of urine you pass; it will also increase the number of times you need to go to the toilet. By taking your last dose around 2 pm, there may be less chance that your sleep is disturbed.
How long to take it for
Continue taking your medicine for as long as your doctor tells you.
Ask your doctor if you are not sure how long to take the medicine for.
If you forget to take it
If it is almost time to take your next dose, skip the dose you missed and take your next dose when you are meant to.
Otherwise, take it as soon as you remember, and then go back to taking your medicine as you would normally.
Do not take a double dose to make up for the dose that you missed. This may increase the chance of you getting an unwanted side effect.
If you are not sure what to do, ask your doctor or pharmacist.
If you have trouble remembering to take your medicine, ask your pharmacist for some hints.
If you take too much (overdose)
Immediately telephone your doctor or the Poisons Information Centre (telephone 13 11 26) for advice or go to Accident and Emergency at the nearest hospital, if you think that you or anyone else may have taken too much of this medicine. Do this even if there are no signs of discomfort or poisoning. You may need urgent medical attention.
If you take too much furosemide (frusemide), you may feel confused, dehydrated, dizzy or you may pass excessive urine.
While you are taking this medicine
Things you must do
If you are about to be started on any new medicine, remind your doctor and pharmacist that you are taking this medicine.
Tell any other doctors, dentists, and pharmacists who treat you that you are taking this medicine.
If you are going to have surgery, tell the surgeon or anaesthetist that you are taking this medicine. It may affect other medicines used during surgery.
If you become pregnant or start to breastfeed while taking this medicine, tell your doctor immediately.
If you are about to have any blood tests, tell your doctor that you are taking this medicine. It may interfere with the results of some tests.
Keep all your doctor's appointments so that your progress can be checked. Your doctor may do some tests from time to time to make sure the medicine is working and to prevent unwanted side effects.
Tell your doctor if you have excessive vomiting or diarrhoea while taking this medicine or if you experience any of the following symptoms:
- dry mouth or thirst
- fainting
- weakness, tiredness or drowsiness
- muscle pain or cramps
- fast heart beat
- passing less urine than normal
If you experience these symptoms, you may be dehydrated because you are losing too much water.
Things you must not do
Do not take this medicine to treat any other complaints unless your doctor tells you to.
Do not give your medicine to anyone else, even if they have the same condition as you.
Do not stop taking your medicine or lower the dosage without checking with your doctor.
Things to be careful of
Make sure you drink enough water during any exercise and during hot weather when you are taking furosemide (frusemide), especially if you sweat a lot. If you do not drink enough water while taking furosemide (frusemide), you may feel faint or light-headed or sick. This is because your blood pressure is dropping suddenly, and you are dehydrating. If you continue to feel unwell, tell your doctor.
If you feel light-headed, dizzy or faint, get up slowly when getting out of bed or standing up. You may feel light-headed or dizzy when you begin to take furosemide (frusemide). This is because your blood pressure is falling suddenly. Standing up slowly, especially when you get up from beds or chairs, will help your body get used to the change in position and blood pressure. If this problem continues or gets worse, talk to your doctor.
Be careful driving or operating machinery until you know how furosemide (frusemide) affects you. Diuretic medicines may cause dizziness or light-headedness in some people. Make sure you know how you react to your medicine before you drive a car, operate machinery, or do anything else that could be dangerous if you are dizzy or lightheaded.
If this occurs do not drive.
If you drink alcohol or take strong painkillers, dizziness or light-headedness may be worse.
The effects of alcohol could be made worse while taking furosemide (frusemide). It is not recommended that you drink alcohol while taking furosemide (frusemide).
If you are taking furosemide (frusemide) for a long period of time, you should check with your doctor to determine whether you should eat more potassium-containing foods or take potassium supplements. However, increasing the amount of potassium in your diet may not be necessary and could be harmful. Check with your doctor.
Furosemide (frusemide) may cause your skin to become more sensitive to the sun. If this happens you should take care to wear protective clothing including a hat and sun block when you are outside.
Side effects
Tell your doctor or pharmacist as soon as possible if you do not feel well while you are taking this medicine.
All medicines can have side effects. Sometimes they are serious, most of the time they are not. You may need medical attention if you get some of the side effects.
Do not be alarmed by the following lists of side effects. You may not experience any of them.
Ask your doctor or pharmacist to answer any questions you may have.
Tell your doctor if you notice any of the following and they worry you:
- very dry mouth or unusual thirst
- weight loss
- weakness or tiredness
- numbness or tingling in the hands and/or feet
- calf muscle spasms
- muscle pains or cramps
- joint pain or stiffness
- restlessness
- drowsiness or a lack of energy
- dizziness or light-headedness
- headache
- fever
- vomiting or nausea
- diarrhoea
- blurred or impaired vision
- unusual bleeding or bruising under the skin
- ringing or buzzing in the ears
- confusion.
Tell your doctor as soon as possible if you notice any of the following:
- irregular or fast heart beat
- passing less urine than is normal for you
- severe stomach pain, often with nausea or vomiting
- severe dizziness or a spinning sensation
- increased sensitivity to sunlight
- flaking or peeling of the skin
- symptoms of anaemia such as tiredness, being short of breath when exercising, dizziness and looking pale
- frequent infections such as fever, severe chills, sore throat or mouth ulcers
- bleeding or bruising more easily than normal, nose bleeds
- loss of control of your bladder or bowels (incontinence)
- gout, a disease with painful, swollen joints
- deafness or ringing in the ears.
These may be serious side effects of furosemide (frusemide) and you may need urgent medical attention.
If any of the following happen, tell your doctor immediately or go to Accident and Emergency at your nearest hospital:
- chest pain
- fainting or having a rapid, weak pulse
- lockjaw
- red, often itchy spots similar to the rash seen with measles which starts on the limbs and sometimes on the face and body. The spots may blister and may progress to form raised red, pale-centred marks. Those affected may have fever, sore throat, headache with or without diarrhoea.
- yellowing of the skin and/or eyes (jaundice).
These are very serious side effects and you may need urgent medical attention or hospitalisation.
Tell your doctor or pharmacist if you notice anything that is making you feel unwell.
Other side effects not listed above may occur in some people.
Storage and disposal
Storage
Keep your furosemide (frusemide) tablets in the bottle until it is time to take them. If you store your furosemide (frusemide) tablets out of the container they may not keep well.
Keep your medicine in a cool dry place where the temperature stays below 25°C.
Do not store this medicine or any other medicine in the bathroom or near a sink. Do not leave it on a window sill or in the car. Heat, sunlight and dampness can destroy some medicines.
Keep it where children cannot reach it. A locked cupboard at least one-and-a-half metres above the ground is a good place to store medicines.
Disposal
If your doctor tells you to stop taking this medicine or the expiry date has passed, ask your pharmacist what to do with any medicine that is left over.
Product description
What APO-Frusemide looks like
20 mg tablets:
White to off-white round tablets, debossed with 'F2' on one side and plain on the other side. AUST R 186517.
Packaged in bottles of 50 and 100 tablets.
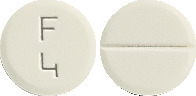
40 mg tablets:
White to off-white round tablets, debossed with 'F4' on one side and breakline on the other side. AUST R 186516.
Packaged in bottles of 30, 50, 60 and 100 tablets.
* Not all strengths and/or pack sizes may be available.
Ingredients
Each tablet contains 20 mg or 40 mg of furosemide (frusemide) as the active ingredient.
It also contains the following inactive ingredients:
- lactose monohydrate
- maize starch
- pregelatinised maize starch,
- sodium starch glycollate (type A)
- magnesium stearate.
This medicine contains sugars as lactose. It is gluten free and free of azo dyes.
Sponsor
Arrotex Pharmaceuticals Pty Ltd
15-17 Chapel Street
Cremorne VIC 3121
www.arrotex.com.au
This leaflet was last updated in October 2023.
Published by MIMS November 2023


 Chemical name: 4-chloro-2-(furan-2-ylmethylamino)-5-sulfamoylbenzoic acid.
Chemical name: 4-chloro-2-(furan-2-ylmethylamino)-5-sulfamoylbenzoic acid.