What is in this leaflet
Read this leaflet carefully before taking your medicine.
This leaflet answers some common questions about memantine. It does not contain all the available information. It does not take the place of talking to your doctor, pharmacist or diabetes educator.
The information in this leaflet was last updated on the date listed on the last page. More recent information on this medicine may be available.
Ask your doctor or pharmacist:
- if there is anything you do not understand in this leaflet,
- if you are worried about taking your medicine, or
- to obtain the most up-to-date information.
You can also download the most up to date leaflet from www.apotex.com.au.
All medicines have risks and benefits. Your doctor has weighed the risks of you taking this medicine against the benefits expected for you.
Pharmaceutical companies cannot give you medical advice or an individual diagnosis.
Keep this leaflet with your medicine. You may need to read it again.
What this medicine is used for
The name of your medicine is APO-Memantine.
It contains the active ingredient, memantine (as memantine hydrochloride).
This medicine is used to treat moderately severe to severe Alzheimer's disease (AD). AD can be described as a general decline in all areas of mental ability.
Ask your doctor if you have any questions about why it has been prescribed for you. Your doctor may have prescribed this medicine for another reason.
This medicine is only available with a doctor's prescription.
How it works
Memantine belongs to a group of medicines called N-methyl-D-aspartate (NMDA) receptor antagonists. It is thought to work by protecting NMDA receptors in the brain against high levels of the chemical glutamate, which could be the cause of brain degeneration. NMDA receptors are involved in the transmission of nerve signals within the brain, e.g. in learning and memory.
This medicine should improve your thinking capacity and your ability to remember.
There is no evidence that this medicine is addictive.
Use in children
This medicine should not be used in children.
Before you take this medicine
When you must not take it
Do not take this medicine if:
- You have a seizure disorder or a history of seizures (fits or epilepsy).
- You are hypersensitive to, or have had an allergic reaction to, memantine or any of the ingredients listed at the end of this leaflet.
Symptoms of an allergic reaction may include: cough, shortness of breath, wheezing or difficulty breathing; swelling of the face, lips, tongue, throat or other parts of the body; rash, itching or hives on the skin; fainting; or hay fever-like symptoms.
If you think you are having an allergic reaction, do not take any more of the medicine and contact your doctor immediately or go to the Accident and Emergency department at the nearest hospital. - The expiry date (EXP) printed on the pack has passed.
- The packaging is torn, shows signs of tampering or it does not look quite right.
Before you start to take it
Before you start taking this medicine, tell your doctor if:
- You have allergies to:
- any other medicines
- any other substances, such as foods, preservatives or dyes.
- You have or have had any medical conditions, especially the following:
- a history of convulsions or are at risk of epilepsy
- kidney problems
- severe bladder infection
- liver problems
- heart or blood vessel problems
- high blood pressure.
- You are currently pregnant or you plan to become pregnant. Do not take this medicine whilst pregnant until you and your doctor have discussed the risks and benefits involved.
- You are currently breastfeeding or you plan to breast-feed. Do not take this medicine until you and your doctor have discussed the risks and benefits involved.
- You have recently changed your diet or intend to change your diet substantially, for example if you wish to become a vegetarian.
- If you are lactose intolerant, contact your doctor before taking this medicine. The 10mg strength tablet contains lactose.
- You are planning to have surgery or an anaesthetic.
- You are currently receiving or are planning to receive dental treatment.
- You are taking or are planning to take any other medicines. This includes vitamins and supplements that are available from your pharmacy, supermarket or health food shop.
Some medicines may interact with memantine. These include:
- medicines used to treat stomach cramps or spasms, or travel sickness (anticholinergics)
- atropine, a medicine used in some eye drops
- levodopa, bromocriptine, amantadine and other medicines for the treatment of Parkinson's disease
- anticonvulsants and barbiturates, used to treat epilepsy or fits
- ketamine, an anaesthetic agent
- medicines used to treat certain mental and emotional conditions (psychoses or schizophrenia)
- dantrolene and baclofen, used to treat leg cramps or to relax muscles
- dextromethorphan, contained in cough, cold and flu medicines
- quinidine and procainamide, used to treat irregular heart beat
- nicotine, contained in patches or gums or if you smoke
- cimetidine and ranitidine, used to treat stomach ulcers or reflux
- urinary alkalinisers, used to treat urinary tract infection
- quinine, a medicine used to treat malaria
- anticoagulant medications such as warfarin, used to prevent blood clots.
If you are taking any of these you may need a different dose or you may need to take different medicines.
Other medicines not listed above may also interact with memantine.
How to take this medicine
Follow carefully all directions given to you by your doctor. Their instructions may be different to the information in this leaflet.
How much to take
Your doctor will tell you how much of this medicine you should take. This will depend on your condition and whether you are taking any other medicines.
Your doctor will decide what dose you will receive. This depends on your condition and other factors, such as your weight and your response to the medicine.
Your doctor will start you on smaller doses which will be gradually increased for three weeks until the dose is reached where memantine works best for you.
- Week 1 (5 mg per day):
Take half a 10mg tablet (white). - Week 2 (10 mg per day):
Take one 10mg tablet (white). - Week 3 (15 mg per day):
Take one and a half 10mg tablet (white). - From week 4 onwards (20 mg per day):
Take two 10mg tablets (white) or one 20mg tablet (pale red).
Do not stop taking your medicine or change your dosage without first checking with your doctor.
When to take it
Swallow the tablets with a full glass of water. Do not chew them.
It does not matter if you take it before, with or after food.
How to take it
Taking your medicine at the same time each day will have the best effect. It will also help you remember when to take it.
How long to take it for
Continue taking your medicine for as long as your doctor tells you.
Make sure you have enough to last over weekends and holidays.
If you forget to take it
If it is almost time for your next dose, skip the dose you missed and take your next dose when you are meant to.
If you are not sure what to do, ask your doctor or pharmacist.
Do not take a double dose to make up for missed doses. This may increase the chance of you experiencing side effects.
If you have trouble remembering to take your medicine, ask your pharmacist for some hints.
If you take too much (overdose)
If you think that you or anyone else may have taken too much of this medicine, immediately telephone your doctor or the Poisons Information Centre (Tel: 13 11 26 for Australia) for advice. Alternatively, go to the Accident and Emergency Department at your nearest hospital.
Do this even if there are no signs of discomfort or poisoning. You may need urgent medical attention.
Symptoms of an overdose may include feeling dizzy, tired or having a headache. You may feel confused and see, feel or hear things that are not there. You could also have a seizure.
While you are taking this medicine
Things you must do
Tell your doctor that you are taking this medicine if:
- you are about to be started on any new medicine
- you are pregnant or are planning to become pregnant
- you are breastfeeding or are planning to breast-feed
- you are about to have any blood tests
- you are going to have surgery or an anaesthetic or are going into hospital.
Your doctor may occasionally do tests to make sure the medicine is working and to prevent side effects. Go to your doctor regularly for a check-up.
Tell any other doctors, dentists and pharmacists who are treating you that you take this medicine.
Things you must not do
Do not:
- Give this medicine to anyone else, even if their symptoms seem similar to yours.
- Take your medicine to treat any other complaints unless your doctor or pharmacist tells you to.
- Stop taking your medicine, or lower the dosage, without checking with your doctor.
Things to be careful of
Be careful when driving or operating machinery until you know how this medicine affects you.
Your doctor will discuss with you whether your condition allows you to drive or operate machinery safely. Furthermore, memantine may change your reactivity which may make driving or using machinery inappropriate.
Alzheimer's disease has been associated with depression and thoughts of suicide. All mentions of suicide or violence by a patient must be taken seriously.
If you or someone you know demonstrates suicide-related behaviour while taking memantine, contact a health care provider immediately, or go to the nearest hospital for treatment.
Possible side effects
Tell your doctor as soon as possible if you do not feel well while you are taking memantine or if you have any concerns.
Do not be alarmed by the following lists of side effects. You may not experience any of them. All medicines may have some unwanted side effects. Sometimes they are serious, but most of the time, they are not.
Tell your doctor if you notice any of the following:
- tiredness, sleeplessness or problems sleeping
- dizziness
- diarrhoea, vomiting, or nausea
- loss of appetite
- feeling anxious
- conjunctivitis
- inflammation of the liver and/or changes in liver function tests.
Tell your doctor as soon as possible if you notice any of the following.
These may be serious side effects. You may need urgent medical attention:
- swelling of hands, ankles or feet
- headache
- feeling confused
- seeing, feeling or hearing things that are not there
- having fixed, irrational ideas that are not shared by others
- depression or suicidal thoughts.
Other side effects not listed above may occur in some people.
Allergic reactions
If you think you are having an allergic reaction to memantine, do not take any more of this medicine and tell your doctor immediately or go to the Accident and Emergency department at your nearest hospital.
Symptoms of an allergic reaction may include some or all of the following:
- cough, shortness of breath, wheezing or difficulty breathing
- swelling of the face, lips, tongue, throat or other parts of the body
- rash, itching or hives on the skin
- fainting
- hay fever-like symptoms.
Storage and disposal
Storage
Keep your medicine in its original packaging until it is time to take them.
If you take the tablets out of their original packaging they may not keep well.
Keep your medicine in a cool dry place where the temperature will stay below 25°C.
Do not store your medicine, or any other medicine, in the bathroom or near a sink. Do not leave it on a window sill or in the car. Heat and dampness can destroy some medicines.
Keep it where children cannot reach it. A locked cupboard at least one-and-a-half metres above the ground is a good place to store medicines.
Disposal
If your doctor tells you to stop taking this medicine or it has passed its expiry date, your pharmacist can dispose of the remaining medicine safely.
Product description
What APO-Memantine looks like
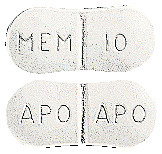
10 mg tablets:
White, peanut shaped, biconvex film coated tablet. Engraved "APO" bisect "APO" on one side, "MEM" bisect "10" on the other side.
They are packaged in a blister pack of 56 tablets
Also packaged in blister packs of 14, 30, 50, 100 tablets (not marketed).
Also packaged in bottles of 14, 30, 50, 56 & 1000 tablets (not marketed).
20 mg tablets:
Pale red, oval, biconvex, coated tablet. Engraved "MEM 20" on one side, "APO" on the other side.
They are packaged in a blister pack of 28 tablets
Ingredients
Each tablet contains 10 mg or 20mg of Memantine Hydrochloride, as the active ingredient.
The 10mg tablets also contain the following inactive ingredients:
- Lactose monohydrate
- Microcrystalline cellulose
- Croscarmellose sodium
- Magnesium stearate
- Hypromellose
- hyprolose
- Macrogol 8000
- Titanium dioxide.
The 20mg tablets also contain the following inactive ingredients:
- Microcrystalline cellulose
- Croscarmellose sodium
- Methylcellulose
- Magnesium stearate
- Hypromellose
- hyprolose
- Macrogol 8000
- Titanium dioxide
- Iron oxide red
- Iron oxide yellow.
This medicine is gluten-free, sucrose-free, tartrazine-free and free of other azo dyes.
The 10mg tablets contains sugars as lactose.
Australian Registration Numbers
APO-Memantine 10 mg tablets blister pack:
AUST R 159582.
APO-Memantine 10 mg tablets bottles:
AUST R 159576.
APO-Memantine 20 mg tablets blister pack:
AUST R 207782.
Sponsor
Arrotex Pharmaceuticals Pty Ltd
15-17 Chapel Street
Cremorne VIC 3121
www.arrotex.com.au
This leaflet was last updated in: September 2023.
Published by MIMS October 2023


 The following adverse events were reported with memantine at a frequency between 1% and < 2% at an incidence greater than placebo in patients with moderately severe to severe AD: pain, abnormal crying, influenza-like symptoms, leg pain, syncope, dependent oedema, hypertonia (increased muscle tone), gastroenteritis, bradycardia, hyperuricaemia, hypertension, dehydration, dyspnoea, hypokalaemia, arthrosis, angina pectoris, purpura, rash, basal cell carcinoma, cerebrovascular disorder, phlebitis, deep thrombophlebitis, tooth ache and tooth caries. As in Table 1, causality to memantine has not been established.
The following adverse events were reported with memantine at a frequency between 1% and < 2% at an incidence greater than placebo in patients with moderately severe to severe AD: pain, abnormal crying, influenza-like symptoms, leg pain, syncope, dependent oedema, hypertonia (increased muscle tone), gastroenteritis, bradycardia, hyperuricaemia, hypertension, dehydration, dyspnoea, hypokalaemia, arthrosis, angina pectoris, purpura, rash, basal cell carcinoma, cerebrovascular disorder, phlebitis, deep thrombophlebitis, tooth ache and tooth caries. As in Table 1, causality to memantine has not been established. Memantine was very well tolerated with similar frequency and type of adverse events observed with memantine compared with placebo.
Memantine was very well tolerated with similar frequency and type of adverse events observed with memantine compared with placebo. Memantine was well tolerated, with physicians rating tolerability as very good in 71% of memantine and 69% of placebo treated patients. In the remaining patients tolerability was assessed as good, with the exception of one memantine treated patient where it was assessed as moderate.
Memantine was well tolerated, with physicians rating tolerability as very good in 71% of memantine and 69% of placebo treated patients. In the remaining patients tolerability was assessed as good, with the exception of one memantine treated patient where it was assessed as moderate. Chemical Name: 1-amino-3, 5-dimethyl-adamantane hydrochloride.
Chemical Name: 1-amino-3, 5-dimethyl-adamantane hydrochloride.