What is in this leaflet
Read this leaflet carefully before taking your medicine. This leaflet answers some common questions about APO-Nifedipine XR. It does not contain all the available information. It does not take the place of talking to your doctor or pharmacist.
The information in this leaflet was last updated on the date listed on the last page. More recent information on this medicine may be available.
Ask your doctor or pharmacist:
- if there is anything you do not understand in this leaflet,
- if you are worried about taking your medicine, or
- to obtain the most up-to-date information.
You can also download the most up to date leaflet from www.arrotex.com.au.
All medicines have risks and benefits. Your doctor has weighed the risks of you using this medicine against the benefits they expect it will have for you.
Pharmaceutical companies cannot give you medical advice or an individual diagnosis.
Keep this leaflet with your medicine. You may want to read it again.
What this medicine is used for
The name of your medicine is APO-Nifedipine XR. It contains the active ingredient, nifedipine.
It is used to treat hypertension (high blood pressure) or to prevent chronic stable angina, a type of angina.
APO-Nifedipine XR is not used for the relief of a sudden attack of angina or to manage unstable angina.
Ask your doctor if you have any questions about why this medicine has been prescribed for you. Your doctor may have prescribed this medicine for another reason.
This medicine is available only with a doctor's prescription.
How it works
Nifedipine belongs to a group of medicines called calcium channel blockers. They work by relaxing and opening up the blood vessels in the body to lower blood pressure and to improve the supply of blood and oxygen to the heart.
APO-Nifedipine XR is designed to allow the slow release of the nifedipine from the tablet after it is taken.
There is no evidence that this medicine is addictive.
Before you take this medicine
When you must not take it
Do not take this medicine if:
- You have or have had any of the following:
- a heart attack in the last 8 days
- cardiogenic shock (very low blood pressure due to a failing heart)
- a Kock Pouch (an ileostomy)
- the rare inherited problems of galactose intolerance, Lapp lactase deficiency, or glucose-galactose malabsorption. These tablets contain lactose. - You are taking another medicine called rifampicin, an antibiotic used to treat various infections
- You are pregnant.
Nifedipine may affect your developing baby if you take it during pregnancy. - You are breast-feeding.
Nifedipine may pass into human breast milk. - The expiry date (EXP) printed on the pack has passed.
- The packaging is torn, shows signs of tampering or it does not look quite right.
- You have had an allergic reaction to nifedipine , similar medicines such as amlodipine, felodipine, lercanidipine, nimodipine and isradipine or any of the ingredients listed at the end of this leaflet.
Symptoms of an allergic reaction may include cough, shortness of breath, wheezing or difficulty breathing; swelling of the face, lips, tongue, throat or other parts of the body; rash, itching or hives on the skin; fainting or hayfever-like symptoms.
If you think you are having an allergic reaction, contact your doctor immediately or go to the Accident and Emergency department at the nearest hospital.
Before you start to take it
Before you start taking this medicine, tell your doctor if:
- You have allergies to:
- any other medicines
- any other substances, such as foods, preservatives or dyes.
- You have or have had any medical conditions, especially the following:
- heart problems such as heart failure, angina or narrowing of any of the blood vessels going into or out of the heart
- other heart or blood vessel disorders
- low blood pressure
- stroke
- mini-stroke (also known as TIA transient ischaemic attack)
- diabetes
- liver problems
- kidney disease or having dialysis
- narrowing of your oesophagus or intestine, e.g. due to previous injury, infection or surgery
- prolonged diarrhoea or other bowel problems, e.g. Crohn’s Disease or Ulcerative Colitis
- surgery on your bowel.
- You are currently pregnant or breast-feeding or you plan to become pregnant or breast-feed. Your doctor will discuss alternative medicines with you, as you must not take nifedipine whilst pregnant or breast feeding.
- You are planning to have surgery or an anaesthetic or are going into hospital.
- You are currently receiving or are planning to receive dental treatment.
- You are taking or are planning to take any other medicines, This includes vitamins and supplements that are available from your pharmacy, supermarket or health food shop.
Taking other medicines
Some medicines may interact with nifedipine. These include:
- beta blockers, e.g. metoprolol, atenolol
- other medicines used to treat high blood pressure or angina, e.g. diltiazem
- medicines used to treat arrhythmia (fast or irregular heartbeats), e.g. quinidine
- other medicines used to treat heart disease, e.g. digoxin
- some medicines used to treat stomach ulcers and heartburn, e.g. cimetidine, cisapride
- rifampicin, used to treat tuberculosis and other serious infections
- other medicines used to treat bacterial infections, e.g. erythromycin, quinupristin, dalfopristin
- medicines used to treat fungal infections, e.g. ketoconazole
- medicines used to treat HIV, e.g. ritonavir
- medicines used to treat epilepsy, e.g. phenytoin, carbamazepine, valproic acid, phenobarbitone
- anti-depressants, e.g. fluoxetine, nefazodone
- tacrolimus, used to prevent rejection after organ transplant tacrolimus, a medicine used after organ transplants.
You should not eat grapefruit or drink grapefruit juice while you are taking nifedipine or for 3 days before starting to take nifedipine, because this may cause your blood pressure to drop too low.
If you are taking any of these you may need a different dose or you may need to take different medicines.
Other medicines not listed above may also interact with nifedipine.
How to take this medicine
Follow carefully all directions given to you by your doctor or pharmacist. Their instructions may be different to the information in this leaflet.
How much to take
Your doctor or pharmacist will tell you how much of this medicine you should take. This will depend on your condition and whether you are taking any other medicines.
The usual starting dose is 30 mg (one 30 mg tablet) daily.
Your doctor may increase the dose slowly over several weeks depending on how you respond to this medicine. If you are being treated for high blood pressure the maximum dose is 120 mg, and if you have chronic angina, the maximum dose is 90 mg.
If a dose less than 30 mg is needed you will have to take a different brand of nifedipine.
If you have liver problems or are taking certain other medicines or you are elderly or of South Asian origin, your doctor may prescribe a lower dose.
Children under 18 years of age must not take this medicine.
Do not stop taking your medicine suddenly or change your dosage without first checking with your doctor.
How to take it
Swallow the tablets whole with a glass of liquid.
Do not crush, chew or break up the tablets.
Avoid drinking grapefruit juice whilst taking this medicine.
When to take it
Take this medicine at the same time each day, usually in the morning.
Taking it at the same time each day will have the best effect and will also help you remember when to take it.
It does not matter if you take it before, with or after food.
How long to take it for
APO-Nifedipine XR helps control your condition, but does not cure it. Therefore, you must take it every day.
Continue taking your medicine for as long as your doctor tells you.
Make sure you have enough to last over weekends and holidays.
Do not stop taking the tablets suddenly unless you are told to by your doctor.
If you forget to take it and it is almost time (within 12 hours) to take your next dose, skip the missed dose and take your next dose at the usual time. Otherwise (if more than 12 hours to the next dose), take it as soon as you remember and then go back to taking your medicine as you would normally.
Do not take a double dose to make up for missed doses. This may increase the chance of unwanted side effects.
If you have trouble remembering to take your medicine, ask your pharmacist for some hints to help you remember.
If you take too much (overdose)
If you think that you or anyone else may have taken too much of this medicine, immediately telephone your doctor or the Poisons Information Centre (Tel: 13 11 26 in Australia) for advice. Alternatively go to the Accident and Emergency Department at your nearest hospital.
Do this even if there are no signs of discomfort or poisoning. You may need urgent medical attention.
If you take too much nifedipine, you may feel dizzy or experience flushing and fainting due to a drop in blood pressure, irregular or fast or slow heart beats; fast or troubled breathing and even loss of consciousness.
While you are taking this medicine
Things you must do
Take the tablets exactly as you are told to by your doctor.
If you do not follow your doctor’s instruction you may not get control of your blood pressure or angina.
Tell your doctor if you continue to have chest pain or angina attacks or if they become more frequent while you are taking APO-Nifedipine XR.
Tell your doctor that you are taking this medicine if:
- you are about to be started on any new medicine
- you are pregnant or are planning to become pregnant
- you are breast-feeding or are planning to breast-feed
- you are about to have any blood or urine tests, or a Barium Contrast X ray
- you are going to have surgery or an anaesthetic or are going into hospital.
If you are taking a beta-blocker and you doctor has told you to stop taking it, make sure you gradually stop taking the beta blocker over a few days,
Your doctor may do tests to make sure the medicine is working and to prevent side effects, especially if you are taking other tablets as well or you have other medical conditions. Go to your doctor regularly for a check-up.
Tell any other doctors, dentists and pharmacists who are treating you that you take this medicine.
Get up slowly when getting out of bed or standing up. This is to avoid becoming light-headed, dizzy or faint.
If you feel light-headed or dizzy, this may be because your blood pressure is falling suddenly. Standing up slowly, especially when you get up from sleeping or sitting, will help your body get used to the change in position and blood pressure. If this problem gets worse or continues, talk to your doctor.
Tell your doctor if, for any reason, you have not taken your medicine exactly as directed.
Otherwise, your doctor may think that it is not working and change your treatment unnecessarily.
Things you must not do
Do not:
- Give this medicine to anyone else, even if their symptoms seem similar to yours
- Take your medicine to treat any other condition unless your doctor or pharmacist tells you to
- Stop taking your medicine suddenly, or change the dosage, without first checking with your doctor.
Things to be careful of
Be careful when driving or operating machinery until you know how this medicine affects you.
Nifedipine may cause dizziness, light-headedness or fainting in some patients, especially when they first start taking the medicine, when changing the dose or in some cases when taking it with alcohol. If affected, do not drive a vehicle, operate machinery or do anything else that could be dangerous.
If you have been taking this medicine regularly for several weeks, do not suddenly stop using it.
Stopping suddenly may bring on your previous problem. Check with your doctor for the best way to reduce gradually the amount you are taking before stopping completely.
If you have angina, be careful not to overdo physical activities when you first start taking APO-Nifedipine XR.
You may feel better when you start taking it, but you will need time to improve your physical fitness.
Things that may help your condition
Some self-help measures suggested below may help your condition.
Talk to your doctor or pharmacist about them:
- Alcohol - your doctor may advise you to limit your alcohol intake.
- Smoking - your doctor may advise you to stop smoking or at least cut down.
- Exercise - regular exercise helps reduce blood pressure and helps get the heart fitter, but it is important not to overdo it. Walking is good exercise, but try to find a route that is fairly flat. Before starting any exercise, ask your doctor for the program that best suits you.
- Weight – if you are overweight, your doctor may suggest losing some weight to help lower your blood pressure and lessen the amount of work your heart has to do. Some people may need a dietician’s help to lose weight.
- Diet - eat a healthy low-fat diet that includes plenty of fresh vegetables, fruit, bread, cereals and fish. Also eat less fat and sugar.
- Salt - your doctor may advise you to watch the amount of salt in your diet. To reduce your salt intake, you can use minimum salt in cooking and avoid salt at the table.
Possible side effects
Tell your doctor or pharmacist as soon as possible if you do not feel well while you are taking APO-Nifedipine XR or if you have any questions or concerns.
Do not be alarmed by the following lists of side effects. You may not experience any of them. All medicines can have side effects.
Sometimes they are serious but most of the time they are not.
Tell your doctor or pharmacist if you notice any of the following and they worry you.
This list includes the more common side effects. Mostly, these are mild:
- Headache
- Feeling dizzy
- Fast or irregular heartbeats
- constipation
- general swelling and/or swelling of arms, ankles or legs
- generally feeling unwell or in pain
- jaundice
Your doctor may need to monitor your liver function, as APO-Nifedipine can increase your liver enzymes. You may not experience any specific symptoms.
If you experience any of the following, stop taking your medicine and contact your doctor immediately or go to the Accident and Emergency department at your nearest hospital.
These are very serious side effects and are usually very rare. You may need urgent medical attention or hospitalisation.
- fast, thumping or irregular heartbeat
- problems breathing
- rash, itching or hives on the skin.
- swelling of the face, lips, tongue, or other parts of the body
- signs of liver problems such as yellowing of the skin and/or eyes(jaundice)
- chest pain
- signs of frequent infections such as fever, severe chills, sore throat, or mouth ulcers.
These serious side effects are not common. If you have these side effects, you may need urgent medical attention.
There have been reports of purple/brown discolouration of the skin or redness, flaking and itching of the skin. Also, it has been reported that some people develop a rash or blistering of the skin when they are exposed to sunlight.
In very rare cases, the undissolved shell of the Apo-Nifedipine tablet or “ghosttablets” may not be excreted in the faeces and may collect in the stomach. Tell your doctor if you experience symptoms of bowel blockage. Surgery may be necessary to remove these shells.
In a small number of cases of in vitro fertilisation, medicines like nifedipine appeared to have interfered with the normal function of sperm. This effect went away after the medicine was stopped. In those men who are taking APO-Nifedipine XR and are repeatedly unsuccessful in fathering a child by in vitro fertilisation, the medicine should be considered as one of the possible causes if no other explanation can be found.
Tell your doctor or pharmacist if you notice anything that is making you feel unwell. Other side effects not listed above may also occur in some people.
Allergic reactions
If you think you are having an allergic reaction to APO-Nifedipine XR, do not take any more of this medicine and tell your doctor immediately or go to the Accident and Emergency department at your nearest hospital.
Symptoms of an allergic reaction may include some or all of the following:
- cough, shortness of breath, wheezing or difficulty breathing.
- swelling of the face, lips, tongue, or other parts of the body
- rash, itching or hives on the skin
- fainting
- hayfever-like symptoms
Storage and disposal
Storage
Keep your medicine in its original packaging until it is time to take it.
If you take your medicine out of its original packaging it may not keep well.
Keep your medicine in a cool dry place where the temperature will stay below 25°C.
Do not store your medicine, or any other medicine, in the bathroom or near a sink. Do not leave it on a window sill or in the car. Heat and dampness can destroy some medicines.
Keep this medicine where children cannot reach it. A locked cupboard at least one-and-a-half metres above the ground is a good place to store medicines.
Disposal
If your doctor or pharmacist tells you to stop taking this medicine or it has passed its expiry date, your pharmacist can dispose of the remaining medicine safely.
Product description
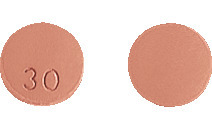
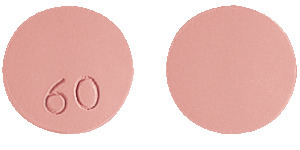
What APO- Nifedipine XR looks like
APO-NIFEDIPINE XR 30 mg tablets: Round, pale red tablet marked “30” on one side.
APO-NIFEDIPINE XR 60 mg tablets: Round, pale red tablet marked “60” on one side.
Not all strengths, pack types and/or pack sizes may be available.
Ingredients
Each tablet contains 30 mg or 60 mg of nifedipine as the active ingredient.
It also contains the following inactive ingredients:
- purified talc
- lactose monohydrate
- povidone
- carbomer 934P
- hypromellose
- colloidal anhydrous silica
- magnesium stearate
- titanium dioxide
- iron oxide red CI77491
- macrogol 4000
- Eudragit E100.
APO-Nifedipine XR tablets contains lactose. This medicine is gluten-free, sucrose-free, tartrazine-free and free from other azo dyes.
Australian Registration Numbers
APO-Nifedipine XR 30 mg Tablets
AUST R number 152207
APO-Nifedipine XR 60 mg Tablets
AUST R number 152208
Sponsor
Arrotex Pharmaceuticals Pty Ltd
15-17 Chapel Street
Cremorne VIC 3121
Distributor
Arrotex Pharmaceuticals Pty Ltd
15-17 Chapel Street Cremorne
VIC 3121
Arrotex Pharmaceuticals Pty Ltd is the licensee of the registered APO trademark.
This leaflet was last updated in July 2022.
Published by MIMS September 2022


 Molecular Formula: C17H18N2O6.
Molecular Formula: C17H18N2O6.