What is in this leaflet
This leaflet answers some common questions about this medicine. It does not contain all the available information. It does not take the place of talking to your doctor or pharmacist.
All medicines have risks and benefits. Your doctor has weighed the risks of you taking APO- OLMESARTAN/ AMLODIPINE/ HCTZ against the benefits they expect it will have for you.
If you have any concerns about taking this medicine, ask your doctor or pharmacist.
Keep this leaflet with the medicine. You may need to read it again.
What this medicine used for
APO-OLMESARTAN/ AMLODIPINE/ HCTZ is used to treat high blood pressure which is sometimes called hypertension.
Everyone has blood pressure. This pressure helps push blood all around your body. Your blood pressure changes at different times of the day, depending on how busy or worried you are. You have hypertension (high blood pressure) when your blood pressure stays higher than is needed, even when you are calm and relaxed.
There are usually no symptoms of hypertension. The only way of knowing that you have hypertension is to have your blood pressure checked on a regular basis. If high blood pressure is not treated it can lead to serious health problems, including stroke, heart disease and kidney failure.
How this medicine works
This medicine contains olmesartan medoxomil, which belongs to a group of medicines known as angiotensin-II receptor antagonists. Angiotensin-II is a substance produced in the body which causes blood vessels to tighten. This medicine blocks the action of angiotensin-II and therefore relaxes your blood vessels. This helps lower your blood pressure.
This medicine also contains amlodipine besilate, a calcium channel blocker. This reduces the movement of calcium into the cells of the heart and blood vessels. This also helps to lower blood pressure as it relaxes the blood vessels and increases the supply of blood and oxygen to the heart.
This medicine also contains hydrochlorothiazide, a diuretic which reduces the amount of fluid in the body. This also helps to lower blood pressure.
Your doctor may have prescribed this medicine for another reason. Ask your doctor if you have any questions about why this medicine has been prescribed for you.
This medicine is available only with a doctor's prescription.
The safety and effectiveness of this medicine in children and teenagers under the age of 18 years have not been established. This medicine is not addictive.
Before you take this medicine
When you must not take it
Do not take this medicine if you have an allergy to:
- Olmesartan,
- amlodipine besilate, medicines belonging to a group of chemicals called dihydropyridines used to treat blood pressure and other heart problems,
- hydrochlorothiazide, a diuretic
- or any of the ingredients listed at the end of this leaflet or other sulfonamide-derived drugs.
Symptoms of an allergic reaction to this medicine may include skin rash, itchiness, shortness of breath, swelling of the face, lips or tongue, muscle pain or tenderness or joint pain.
Do not take this medicine if:
- you have serious problems with your kidneys
- you have serious problems with your liver
- you have had recent serious heart problems
- you have low potassium or sodium levels in the blood
- you have high calcium or uric acid levels in the blood.
- you have diabetes and are taking a medicine called aliskiren to reduce blood pressure.
Do not take this medicine if you are pregnant or breastfeeding. This medicine may enter your womb, or it may pass into the breast milk and there is the possibility that your baby may be affected.
If pregnancy is discovered this medicine should be discontinued as soon as possible.
Do not take this medicine after the expiry date printed on the pack or if the packaging is torn or shows signs of tampering.
If you are not sure whether you should start taking this medicine, talk to your doctor.
Before you start to take it
Tell your doctor if you have allergies to:
- any other medicines
- any other substances, such as foods, preservatives or dyes.
Tell your doctor if you have or have had any medical conditions, especially the following:
- kidney problems
- liver problems
- heart problems
- diabetes
- excessive vomiting or diarrhoea recently
- high levels of potassium in your blood.
- problems with your adrenal glands (small glands above the kidneys)
- systemic lupus erythematosus, a disease affecting the skin, joints and kidneys
- gout
You must also tell your doctor if you:
- are following a very low salt diet
- are or intend to become pregnant or plan to breastfeed.
- you are taking potassium supplements, potassium-sparing agents, potassium-containing salt substitutes or other medicines that may increase serum potassium (e.g., trimethoprim-containing products)
- you have skin cancer or if you develop a new skin lesion during treatment. Treatment with hydrochlorothiazide, particularly long-term use with high doses, may increase the risk of some types of skin and lip cancer (nonmelanoma skin cancer). Discuss with your doctor how to protect your skin from sun exposure, and avoid artificial tanning
If you have not told your doctor about any of the above, tell him/ her before you start taking this medicine.
Taking other medicines
Tell your doctor or pharmacist if you are taking any other medicines, including any that you get without a prescription from your pharmacy, supermarket or health food shop.
Some medicines and this one may interfere with each other. These include:
- other medicines to treat high blood pressure
- digitalis glycosides, medicines used to treat heart problems
- medicines used to treat angina, such as diltiazem
- antiarrhythmics which treat irregular heartbeats
- non-steroid anti-inflammatory drugs (NSAIDs) or COX-2 inhibitors, medicines used to relieve pain, swelling and other symptoms of inflammation including arthritis
- antacids, medicines used to heartburn and indigestion
- simvastatin, a medicine used to help lower cholesterol levels
- potassium supplements or potassium-containing salt substitutes
- other medicines that may increase serum potassium (e.g., trimethoprim-containing products)
- calcium containing supplements
- lithium or antidepressant medicines
- some antibiotics, such as erythromycin or rifampicin
- some antifungals, such as ketoconazole or itraconazole
- anti-proteases, medicines used to treat HIV infection such as ritonavir
- other diuretics, also known as fluid or water tablets
- insulin and tablets used to treat diabetes
- medicines which lower your immune system, such as corticosteroids, ciclosporin, tacrolimus and cytotoxic medicines used to treat cancer (including radiation therapy)
- alcohol
- laxatives, medicines used to treat constipation
- medicines used to relieve pain
- medicines used to treat epilepsy
- muscle relaxants
- cholestyramine and colestipol, used to treat high cholesterol
- St John's Wort
- grapefruit or grapefruit juice
- medicines used to treat gout, such as allopurinol
- medicines used to treat Parkinson's Disease, such as amantadine
- any medicines that contain aliskiren
- any medicines that contain colesevelam.
These medicines may be affected by this medicine or may affect how well it works. You may need different amounts of your medicines, or you may need to take different medicines.
Other medicines not listed above may also interfere with this medicine.
Your doctor and pharmacist have more information on medicines to be careful with or avoid while taking this medicine.
Use in children
The safety and effectiveness of this medicine in children have not been established.
How to take this medicine
Follow all directions given to you by your doctor or pharmacist carefully. They may differ from the information contained in this leaflet. Your doctor or pharmacist will tell you which tablet you will need to take each day. This depends on your condition, and whether or not you are taking any other medicines.
If you do not understand the directions, ask your doctor or pharmacist for help.
How much to take
The dose of this medicine is one tablet to be taken once a day.
How to take it
Swallow the tablet whole with a full glass of water. Do not chew the tablets.
When to take it
Take this medicine at about the same time each day, with or without food. Taking it at the same time each day will have the best effect. It will also help you remember when to take the tablets.
It does not matter whether you take it with or without food.
How long to take it
This medicine helps to control your condition but does not cure it. Therefore, you must take your medicine every day.
Continue taking your medicine for as long as your doctor tells you.
If you forget to take it
If it is almost time to take your next dose, skip the dose you missed and take your next dose when you are meant to.
Otherwise, take it as soon as you remember, and then go back to taking your medicine as you would normally.
Do not take a double dose to make up for the dose that you missed. This may increase the chance of you getting an unwanted side effect.
If you are not sure what to do, ask your doctor or pharmacist.
If you have trouble remembering to take your medicine, ask your pharmacist for some hints.
If you take too much (overdose)
Immediately telephone your doctor or the Poisons Information Centre (telephone 13 11 26) for advice or go to Accident and Emergency at the nearest hospital, if you think that you or anyone else may have taken too much of this medicine. Do this even if there are no signs of discomfort or poisoning.
You may need urgent medical attention.
If you take too much of this medicine, you may feel light-headed, dizzy or you may faint. You may also have nausea, drowsiness, muscle spasm and a fast heartbeat.
While you are using this medicine
Things you must do
If you are about to be started on any new medicine, remind your doctor and pharmacist that you are taking this medicine.
Tell any other doctors, dentists, and pharmacists who treat you that you are taking this medicine. Make sure you drink enough water during exercise and hot weather when you are taking this medicine, especially if you sweat a lot. If you do not drink enough water while taking this medicine, you may feel light-headed or sick. This is because your blood pressure is dropping suddenly. If you continue to feel unwell, tell your doctor.
If you have excess vomiting and/or diarrhoea while taking this medicine tell your doctor. You may lose too much water and salt and your blood pressure may drop too much. You may also have dry mouth, weakness, drowsiness, confusion, muscle pain or cramps and seizures. Tell your doctor immediately if you experience any of these symptoms.
If you feel light-headed or dizzy after taking your first dose of this medicine, or when your dose is increased, tell your doctor immediately.
If you plan to have surgery that needs a general anaesthetic, tell your doctor or dentist that you are taking this medicine. Your blood pressure may drop suddenly.
If you become pregnant while taking this medicine, tell your doctor immediately.
If you are about to have any blood tests, tell your doctor that you are taking this medicine. It may interfere with the results of some tests.
Tell your doctor if photosensitivity reaction occurs during your treatment.
Tell your doctor immediately in case of acute onset of decreased visual acuity or ocular pain. These could be symptoms of fluid accumulation in the vascular layer of the eye (choroidal effusion) or an increase of pressure in your eye and can happen within hours to weeks of taking OLMEKAR HCT. This can lead to permanent vision loss, if not treated.
Tell your doctor immediately if you experience any fever, severe shortness of breath, breathing faster than normal, difficulty breathing, slightly blue fingertips and lips after taking this medicine. Stop the medication and seek medical attention immediately.
Have your blood pressure checked when your doctor says, to make sure this medicine is working.
Go to your doctor regularly for a check-up. Your doctor may occasionally do a blood test to check your potassium levels and see how your kidneys are working.
Things you must not do
Do not give your medicine to anyone else, even if they have the same condition as you.
Do not take this medicine to treat any other complaints unless your doctor tells you to.
Do not stop taking your medicine or change the dosage without checking with your doctor.
Things to be careful of
If you feel light-headed, dizzy or faint when getting out of bed or standing up, get up slowly. Standing up slowly, especially when you get up from bed or chairs, will help your body get used to the change in position and blood pressure. If this problem continues or gets worse, talk to your doctor.
Be careful driving or operating machinery until you know how this medicine affects you. As with other medicines in this class, this medicine may cause dizziness, light-headedness or tiredness in some people. Make sure you know how you react to this medicine before you drive a car, operate machinery, or do anything else that could be dangerous if you are dizzy or light- headed. If this occurs do not drive.
Be careful when drinking alcohol while you are taking this medicine. If you drink alcohol, dizziness or light- headedness may be worse.
Things that would be helpful for your blood pressure
Some self-help measures suggested below may help your condition. Talk to your doctor or pharmacist about these measures and for more information.
- Alcohol - your doctor may advise you to limit your alcohol intake.
- Weight - your doctor may suggest losing some weight to help lower your blood pressure and help lessen the amount of work your heart has to do. Some people may need a dietician's help to lose weight.
- Diet - eat a healthy diet which includes plenty of fresh vegetables, fruit, bread (preferably wholegrain), cereals and fish. Also eat less sugar and fat (especially saturated fat) which includes sausages, fatty meats, full cream dairy products, biscuits, cakes, pastries, chocolates, chips and coconut. Monounsaturated and polyunsaturated fats from olive oil, canola oil, avocado and nuts are beneficial in small quantities.
- Salt - your doctor may advise you to watch the amount of salt in your diet. To reduce your salt intake you should avoid using salt in cooking or at the table and avoid cooked or processed foods containing high sodium (salt) levels.
- Exercise - regular exercise, maintained over the long term, helps to reduce blood pressure and helps get the heart fitter. Regular exercise also improves your blood cholesterol levels, helps reduce your weight and stress levels, and improves your sleep, mood and ability to concentrate. However, it is important not to overdo it. Walking is good exercise, but try to find a route that is reasonably flat. Before starting any exercise, ask your doctor about the best kind of programme for you.
- Smoking - your doctor may advise you to stop smoking or at least cut down. There are enormous benefits to be gained from giving up smoking. There are many professionals, organisations and strategies to help you quit. Ask your doctor or pharmacist for further information and advice.
Side effects
Tell your doctor or pharmacist as soon as possible if you do not feel well while you are taking this medicine.
This medicine helps most people with high blood pressure, but it may have unwanted side effects in a few people. All medicines can have side effects. Sometimes they are serious, most of the time they are not. You may need medical attention if you get some of the side effects.
If you are over 65 years of age you may have an increased chance of getting side effects.
Hydrochlorothiazide, a component of this medicine, increases sensitivity of the skin to the sun and may increase the risk of some types of skin and lip cancer (non-melanoma skin cancer).
Hydrochlorothiazide, a component of this medicine, may cause a decrease in vision or pain in your eyes due to high pressure (possible signs of fluid accumulation in the vascular layer of the eye (choroidal effusion) or acute angle-closure glaucoma.
Hydrochlorothiazide, a component of this medicine, may cause fever, severe shortness of breath, breathing faster than normal, difficulty breathing, slightly blue fingertips and lips.
Ask your doctor or pharmacist to answer any questions you may have.
The following is a list of possible side effects. Do not be alarmed by the following lists of side effects. You may not experience any of them.
Tell your doctor or pharmacist if you notice any of the following and they worry you:
- feeling light-headed, dizzy or faint
- cough
- headache
- feeling sick (nausea) or vomiting
- stomach pain or discomfort
- diarrhoea
- unusual tiredness or weakness, fatigue
- 'flu-like' symptoms
- runny or blocked nose, or sneezing
- bronchitis
- sore throat and discomfort when swallowing (pharyngitis)
- back pain
- urinary tract infection
- jaundice
- blurred vision
- skin rashes or eczema
- sleep disturbance
- depression
- swelling of the ankles, feet, face or hands
- flushing
The above list includes the more common side effects of your medicine. They are usually mild and short-lived.
Tell your doctor as soon as possible if you notice any of the following:
- skin rash or itchiness
- aching, tender or weak muscles not caused by exercise
- painful joints
- fast heart beat
- shortness of breath or tightness in the chest
- swelling of the face, hands, feet or ankles
- yellowing of the whites of the eyes, dark urine and itching of the skin
- symptoms that may indicate high potassium levels in the blood, such as nausea, diarrhoea, muscle weakness, change in heart rhythm
- symptoms that may indicate water and salt imbalance such as dry mouth, weakness, drowsiness, confusion, muscle pain or cramps and seizures.
The above list includes serious side effects that may require medical attention. Serious side effects are rare.
If any of the following happen, tell your doctor immediately or go to Accident and Emergency at your nearest hospital:
- swelling of the face, lips, mouth, tongue or throat which may cause difficulty in swallowing or breathing
- chest pain
The above list includes very serious side effects. You may need urgent medical attention or hospitalisation. These side effects are very rare.
Tell your doctor or pharmacist if you notice anything that is making you feel unwell.
Other side effects not listed above may also occur in some people.
Storage and Disposal
Storage
Keep your tablets in the pack until it is time to take them. If you take the tablets out of the pack they may not keep well.
Keep your medicine in a cool dry place where the temperature stays below 25°C.
Do not store this medicine or any other medicine in the bathroom or near a sink. Do not leave it on a window sill or in the car. Heat and dampness can destroy some medicines.
Keep it where children cannot reach it. A locked cupboard at least one-and-a-half metres above the ground is a good place to store medicines.
Disposal
If your doctor tells you to stop taking this medicine or the expiry date has passed, ask your pharmacist what to do with any medicine that is left over.
Product description
What it looks like
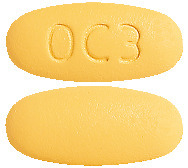
APO-OLMESARTAN/ AMLODIPINE/ HCTZ tablets come in five strengths and each has a different appearance:
APO-OLMESARTAN/ AMLODIPINE/ HCTZ 20/5/12.5 mg (AUST R 312002) is an off white to peach, round, bevel-edged, film- coated tablets debossed with "OC1" on one side and plain on other side.
APO-OLMESARTAN/ AMLODIPINE/ HCTZ 40/5/12.5 mg (AUST R 312010) is a light yellow, round, bevel-edged, film-coated tablets debossed with "OC2" on one side and plain on other side.
APO-OLMESARTAN/ AMLODIPINE/ HCTZ 40/5/25 mg (AUST R 312007) is a light yellow, oval, bevel-edged, film-coated tablets debossed with "OC3" on one side and plain on other side.
APO-OLMESARTAN/ AMLODIPINE/ HCTZ 40/10/12.5 mg (AUST R 312004) is a brick red, round, bevel-edged, film-coated tablets debossed with "OC4" on one side and plain on other side.
APO-OLMESARTAN/ AMLODIPINE/ HCTZ 40/10/25 mg (AUST R 311999) is a brick red, oval, bevel-edged, film-coated tablets debossed with "OC5" on one side and plain on other side.
The product is presented in Alu/Alu blister pack of 10 or 30 film-coated tablets.
Ingredients
APO-OLMESARTAN/ AMLODIPINE/ HCTZ 20/5/12.5 mg contains 20 mg olmesartan medoxomil, 5 mg amlodipine as besilate and 12.5 mg hydrochlorothiazide.
APO-OLMESARTAN/ AMLODIPINE/ HCTZ 40/5/12.5 mg contains 40 mg of olmesartan medoxomil, 5 mg amlodipine as besilate and 12.5 mg hydrochlorothiazide.
APO-OLMESARTAN/ AMLODIPINE/ HCTZ 40/5/25 mg contains 40 mg of olmesartan medoxomil, 5 mg amlodipine as besilate and 25 mg hydrochlorothiazide.
APO-OLMESARTAN/ AMLODIPINE/ HCTZ 40/10/12.5 mg contains 40 mg of olmesartan medoxomil, 10 mg amlodipine as besilate and 12.5 mg hydrochlorothiazide.
APO-OLMESARTAN/ AMLODIPINE/ HCTZ 40/10/25 mg contains 40 mg of olmesartan medoxomil, 10 mg amlodipine as besilate and 25 mg hydrochlorothiazide.
This medicine also contains the following:
- povidone
- pregelatinised maize starch
- silicified microcrystalline cellulose
- lactose monohydrate
- magnesium stearate
- opadry II complete film coating system 85F570046 TAN (20/5/12.5mg)
- opadry II complete film coating system 85F520133 YELLOW (40/5/12.5mg and 40/5/25mg)
- opadry II complete film coating system 85F540170 PINK (40/10/12.5mg and 40/10/25mg)
This medicine does not contain, sucrose, tartrazine or any other azo dyes.
Sponsor
Arrotex Pharmaceuticals Pty Ltd
15-17 Chapel Street,
Cremorne VIC 3121
www.arrotex.com.au
This leaflet was prepared in November 2023.
Published by MIMS December 2023





 Adverse events are listed below by system organ class. Frequencies are defined as: common (≥ 1/100 to < 1/10); uncommon (≥ 1/1,000 to < 1/100); rare (≥ 1/10,000 to < 1/1,000); very rare (< 1/10,000).
Adverse events are listed below by system organ class. Frequencies are defined as: common (≥ 1/100 to < 1/10); uncommon (≥ 1/1,000 to < 1/100); rare (≥ 1/10,000 to < 1/1,000); very rare (< 1/10,000). Other adverse experiences which were not clearly dose related but which were reported with an incidence greater than 1.0% in placebo controlled clinical trials include the following. See Table 3.
Other adverse experiences which were not clearly dose related but which were reported with an incidence greater than 1.0% in placebo controlled clinical trials include the following. See Table 3. The following events occurred in ≤ 1% but > 0.1% of patients in controlled clinical trials or under conditions of open trials or marketing experience where a causal relationship is uncertain; they are listed to alert the physician to a possible relationship:
The following events occurred in ≤ 1% but > 0.1% of patients in controlled clinical trials or under conditions of open trials or marketing experience where a causal relationship is uncertain; they are listed to alert the physician to a possible relationship: There were no apparent differences in terms of seated diastolic blood pressure (SeDBP) or seated systolic blood pressure (SeSBP) reductions in black and non-black patients treated with olmesartan medoxomil, amlodipine and hydrochlorothiazide tablets.
There were no apparent differences in terms of seated diastolic blood pressure (SeDBP) or seated systolic blood pressure (SeSBP) reductions in black and non-black patients treated with olmesartan medoxomil, amlodipine and hydrochlorothiazide tablets.
 In a second double-blind, randomised, parallel-group study [CS8635-A-E302] in 2690 patients (99.9% Caucasian patients), treatment with olmesartan medoxomil, amlodipine and hydrochlorothiazide tablets (20 mg/5 mg/12.5 mg, 40 mg/5 mg/12.5 mg, 40 mg/5 mg/25 mg, 40 mg/10 mg/12.5 mg, 40 mg/10 mg/25 mg) resulted in significantly greater reductions in diastolic and systolic blood pressure compared to the corresponding dual combinations, olmesartan medoxomil 20 mg plus amlodipine 5 mg, olmesartan medoxomil 40 mg plus 5 mg amlodipine and olmesartan medoxomil 40 mg plus 10 mg amlodipine, respectively, after 10 weeks of treatment.
In a second double-blind, randomised, parallel-group study [CS8635-A-E302] in 2690 patients (99.9% Caucasian patients), treatment with olmesartan medoxomil, amlodipine and hydrochlorothiazide tablets (20 mg/5 mg/12.5 mg, 40 mg/5 mg/12.5 mg, 40 mg/5 mg/25 mg, 40 mg/10 mg/12.5 mg, 40 mg/10 mg/25 mg) resulted in significantly greater reductions in diastolic and systolic blood pressure compared to the corresponding dual combinations, olmesartan medoxomil 20 mg plus amlodipine 5 mg, olmesartan medoxomil 40 mg plus 5 mg amlodipine and olmesartan medoxomil 40 mg plus 10 mg amlodipine, respectively, after 10 weeks of treatment. Amlodipine besilate has the following structural formula:
Amlodipine besilate has the following structural formula: Hydrochlorothiazide has the following structural formula:
Hydrochlorothiazide has the following structural formula:
